Abstract
Summary
Type 2 diabetes mellitus (T2DM) is associated with an excess risk of fractures and overall mortality. This study compared hip fracture and post-hip fracture mortality in T2DM and non-diabetic subjects. The salient findings are that subjects in T2DM are at higher risk of dying after suffering a hip fracture.
Introduction
Previous research suggests that individuals with T2DM are at an excess risk of both fractures and overall mortality, but their combined effect is unknown. Using multi-state cohort analyses, we estimate the association between T2DM and the transition to hip fracture, post-hip fracture mortality, and hip fracture–free all-cause death.
Methods
Population-based cohort from Catalonia, Spain, including all individuals aged 65 to 80 years with a recorded diagnosis of T2DM on 1 January 2006; and non-T2DM matched (up to 2:1) by year of birth, gender, and primary care practice.
Results
A total of 44,802 T2DM and 81,233 matched controls (53% women, mean age 72 years old) were followed for a median of 8 years: 23,818 died without fracturing and 3317 broke a hip, of whom 838 subsequently died. Adjusted HRs for hip fracture–free mortality were 1.32 (95% CI 1.28 to 1.37) for men and 1.72 (95% CI 1.65 to 1.79) for women. HRs for hip fracture were 1.24 (95% CI 1.08 to 1.43) and 1.48 (95% CI 1.36 to 1.60), whilst HRs for post-hip fracture mortality were 1.28 (95% CI 1.02 to 1.60) and 1.57 (95% CI 1.31 to 1.88) in men and women, respectively.
Conclusion
T2DM individuals are at increased risk of hip fracture, post-hip fracture mortality, and hip fracture–free death. After adjustment, T2DM men were at a 28% higher risk of dying after suffering a hip fracture and women had 57% excess risk of post-hip fracture mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) is a serious chronic disease. Its prevalence has been steadily increasing over the past few decades but has risen faster in low- and middle-income countries than in high-income countries [1]. T2DM, if not treated properly, can lead to a wide range of serious health problems [2]. T2DM increases patient risk for cardiovascular diseases [3], nephropathy [4], neuropathy [5], retinopathy [6], and foot problems [7]. Fragility fractures have recently been incorporated into this collection [8, 9].
Fragility fractures are those caused by a low impact, such as a fall from a height corresponding to standing, mainly in the humerus, wrist, vertebrae, and hip [10]. Fragility fractures can be seen as a minor complication but have a great socio-economic impact due to direct and indirect costs [11, 12]. Moreover, fractures, especially hip fracture, have been associated with significant decrements in the patient’s quality of life, functional status, and life expectation [13]. In most occasions, the best treatment option for hip fractures is surgical [14]. Surgical treatment attempts to recover the function and quality of life of the patient prior to fracture. However, results will depend on age, comorbidity level, and the patient’s previous ambulation [15]. Hip fracture surgery techniques are somewhat aggressive and require expert hands to avoid secondary complications [16] such as excessive intraoperative bleeding, infections, or functional dependency [17]. Complications in older patients or with a fragile status of health could be fatal [18].
Thus, seeing T2DM as a progressive chronic illness, the increased hip fracture risk could have severe consequences in the patient’s life. However, there is little known on the effect of T2DM status on subsequent post-fracture mortality. The aim of this study was to estimate the impact of T2DM on hip fracture, hip fracture–free death, and post-hip fracture mortality (Fig. 1) in a large population-based cohort using multi-state [19, 20] model analysis.
Methodology
We conducted a population-based cohort study using data from the SIDIAP Database (www.sidiap.org). SIDIAP is an anonymized clinical database that contains information as coded by general practitioners in primary care practices in Catalonia, Spain. SIDIAP is representative of the overall population covering more than five million participants (80% of the Catalan population) [21]. SIDIAP is a validated source of information for epidemiological research and has been previously used to study T2DM as well as for fragility fractures [8, 22,23,24].
Eligible participants were men and women aged between 65 and 80 years with a diagnosis of T2DM on 1 January 2006. Up to two non-T2DM individuals, per each T2DM participant included, were matched by year of birth, sex, and primary care facility. All participants were followed up from 1 January 2006 until the earliest of death, transfer out/migration, or end of the study (31 December 2013).
Main outcomes were incident hip fracture and all-cause mortality. The date of hip fracture was defined as the date general practitioners registered the date of the event in SIDIAP. The date of death was defined as the date of death in the Spanish Mortality Register linked to SIDIAP database. Socio-demographics data, time from T2DM onset, diagnoses as coded using International Classification of Diseases, Tenth Revision (ICD-10), and clinical measurements amongst other clinical information were also included in the database. A validated list of ICD-10 codes was used to identify T2DM status, hip fracture, death, and confounding factors [22].
Statistical analysis
Baseline characteristics of T2DM and non-T2DM participants were described using mean and standard deviation for continuous variables and frequencies for categorical variables. We used multi-state [19] models to compare several transition risks in T2DM and non-T2DM participants. Multi-state models are time-inhomogeneous Markov processes, where the future state of an individual at time t only depends on the current time s (where s < t) and on individual’s state [25]. A progressive illness-death model without recovery was planned (Fig. 1) with the following transitions states: baseline to hip fracture, baseline to hip fracture–free death, and hip fracture to death (i.e. post-fracture mortality). Multi-state models allow simultaneous modelling of these different transitions and estimate cause-specific hazard ratios (HRs), cumulative hazards, and transition probabilities. Potential confounders considered for adjustment were those known clinically relevant for hip fracture risk, such as age, sex, previous major osteoporotic fracture, and previous glucocorticoid use, and for death risk in T2DM and post-hip fracture, such as previous nephropathy, previous ischemic heart disease (IHD), and previous cerebrovascular disease (CVD). All confounding factors were measured at baseline except age which was treated as a time-dependent factor.
Results from the models were presented as cause-specific hazard ratios for hip fracture, hip fracture–free death, and post-hip fracture death according to T2DM status. Graphs of cumulative incidence functions of each state (death, hip fracture, and no event until end of follow-up) were also presented. All analyses were stratified by sex, which otherwise violated proportionality of hazards (PH). PH assumption was tested graphically with the log-log plot of survival and analytically with the test of proportional hazards. The 95% confidence intervals were reported for all estimates. Statistical significance was defined at the P < 0.05 level. All statistical analyses were conducted using R version 3.4.5 for Windows using the mstate package.
Results
A total of 45,313 people aged between 65 and 80 years with a diagnosis of T2DM on 1 January 2006 and 88,729 matched non-diabetic subjects were eligible. Individuals not diagnosed with T2DM who were either users of anti-T2DM drugs or with two measures of glycated haemoglobin above 6.5% were excluded. Individuals with a recorded hip fracture or death on index date were excluded, irrespective of T2DM. Participants that ended unmatched (i.e. with no matched peer remaining) because of the above exclusion criteria were also excluded. Finally, a total of 44,802 T2DM and 81,233 matched non-T2DM participants were included in the study (Fig. 2). Participants were followed for a median (interquartile range) of 8 (7.3 to 8) years representing a total of 880,867 person-years (p-y) of observation: 304,538 p-y T2DM and 576,329 p-y non-T2DM.
In Table 1, baseline demographic and clinical characteristics of study participants are described stratified by T2DM status. Participants with T2DM had a higher prevalence of obesity, cataracts, cardiovascular disease, neuropathy, and nephropathy, and non-T2DM participants had a higher prevalence of anti-osteoporosis drugs and calcium + vitamin D complements. But similar prevalence was observed in terms of previous osteoporotic major fracture or glucocorticoid prescriptions.
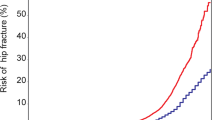
A total of 23,818 participants (10,745 T2DM and 13,073 non-T2DM) died hip fracture–free. Median time to death was 4.2 (interquartile range 1.9 to 6.2) years. Unadjusted mortality rates (in hip fracture–free participants) in T2DM participants were 36.1 (95% CI 35.4 to 36.7) per 1000 p-y and 23.0 (95% CI 22.6 to 23.4) per 1000 p-y for non-T2DM. In Fig. 3a, mortality rates are presented per age and T2DM status in men and women.
A total of 3317 participants (1424 T2DM and 1893 non-T2DM) suffered an incident hip fracture in the study period. Median (IQR) time from baseline to hip fracture was 4.8 (2.9 to 6.5) years. Unadjusted hip fracture incidence rates in T2DM and non-T2DM participants were 4.7 (95% CI 4.4 to 4.9) per 1000 p-y and 3.3 (95% CI 3.1 to 3.4) per 1000 p-y, respectively (Fig. 3b).
Of those 3317 participants who broke a hip, 838 (428 T2DM and 410 non-T2DM) subsequently died. Median (IQR) time from hip fracture to death was 1.5 (0.6 to 3) years. Unadjusted mortality rates in those participants who broke a hip were 66.5 (95% CI 60.4 to 73.0) per 1000 p-y and 46.8 (95% CI 42.2 to 51.5) per 1000 p-y for T2DM and non-T2DM participants, respectively (Fig. 3c).
Multi-state Cox model results are presented in Table 2, which shows the estimated HR, unadjusted and adjusted, for each transition, stratified by sex. After adjusting for age, previous IHD, previous CVD, previous major fracture, previous nephropathy, corticoid prescriptions, calcium + vitamin D, and anti-osteoporosis drugs, T2DM men had a 32% higher hip fracture–free mortality risk and a 24% excess risk of hip fracture, compared with matched non-T2DM during follow-up. In addition, T2DM men were at a 28% higher risk of dying after suffering a hip fracture. After adjusting for the same risk confounders, T2DM women appeared at a 72% higher risk of hip fracture–free death, at a 48% more risk of hip fracture, and at a 57% excess risk of post-hip fracture mortality during the follow-up period.
Cumulative incidence functions for each transition can be obtained from multi-state models. Thus, for a referent participant, it is possible to estimate the probability of being in each transition state (Fig. 4). Given 1000 T2DM women aged 72 and with none of the adjusting factors (previous IHD, previous CVD, previous major fracture, previous nephropathy, corticoid prescriptions, calcium + vitamin D, and anti-osteoporosis drugs) 5 years later from index date, 14 would break a hip and remain alive, 3 would break a hip and die, 83 would die hip fracture–free, and 900 would remain alive without fracturing (Fig. 4). Also, given 1000 T2DM men aged 72 years and with none of the adjusting factors 5 years later from index date, 5 would break a hip and remain alive, 2 would break a hip and die, 140 would die hip fracture–free, and 853 would remain alive without fracturing. Non-parametric estimates of cumulative hazards of the three transitions show also that T2DM participants with respect to non-T2DM had higher risks for hip fracture, hip fracture–free death, and death after hip fracture (supplemental figures).
Stacked prediction probabilities for a T2DM and non-T2DM reference (women or men aged 72 with none of the model adjusting factors (previous IHD, previous CVD, previous major fracture, previous nephropathy, corticoids prescriptions, calcium + vitamin D, and anti-osteoporosis drugs)) participant by sex
Discussion
This population-based cohort study shows that T2DM participants were at higher risk of death, of hip fracture, and of dying after suffering a hip fracture than matched non-T2DM participants. Estimated event probabilities at 5 years suggest that the risk of a hip fracture in T2DM participants is not negligible and neither the subsequent death risk. To our knowledge, this study is the first to explore simultaneously the competing role of death on the relationship of T2DM and hip fracture and the impact of hip fracture on death risk in T2DM participants.
Excess mortality in T2DM participants is well known and mainly associated to a higher risk to develop cardiovascular disease, blindness, kidney failure, and lower limb amputation. A recent meta-analysis [26] of 35 studies about mortality in T2DM participants showed an 85% increase risk for all-cause mortality (pooled HR 1.85, 95% CI 1.79–1.92). In men, excess of mortality was 57% and two-fold increase in women. In our study, this excess of mortality was similar as it was 40% in men and 85% in women.
Different systematic reviews and meta-analyses of observational studies have found a positive association between T2DM and hip fracture with a high variation in estimated effect: Janghorbani et al. [27] found a two-fold increase of hip fracture risk in T2DM men compared with non-T2DM and an almost three-fold increase of hip fracture risk in T2DM men compared with non-T2DM; Jia et al. [28] found an 8% increase of hip fracture risk in T2DM participants compared with non-T2DM; Moayeri et al. [29] found a 20% increase of hip fracture risk in T2DM participants compared with non-T2DM; Dytfeld and Michalak [30] have also shown that post-menopausal women with T2DM have higher hip fracture risk with a 30% increase compared with non-T2DM. Furthermore, a significant heterogeneity was found between studies in each meta-analysis. Explanations of this heterogeneity were in part due to differences on participant’s age, duration of diabetes, differences on follow-up, and local hip fracture incidence. Another key point is the role of death as a competing event, especially in older participants, largely unaccounted for in previous studies. A recent study has found that hip fracture risk in T2DM individuals has been overestimated due to the competing effect of death [31].
Mortality after hip fracture has been described before in general population [32,33,34,35]. In these studies, key preoperative characteristics associated with the risk of mortality up to 12 months were age, male gender, previous fracture functional status, and some comorbidity such as dementia or cognitive impairment, diabetes, cancer, chronic obstructive pulmonary disorder, and cardiac disease. Risk for death was found largely dependent on age. However, at any given age, excess of mortality after hip fracture was found higher in men than in women. In these studies, diabetes was identified as a risk factor in three studies [18, 36, 37], and conclusion was that T2DM individuals have a 44% excess risk of death compared with non-diabetic peers along the first year after hip fracture (pooled HR 1.44, 95% CI 1.13to 1.82). Our results are largely consistent with these published studies.
A relevant association between some anti-diabetic drugs and fracture risk has been described earlier [38, 39]. Further research on the role of anti-diabetic drugs in transition risks could be of great interest. Ferrari et al. [40] have recently proposed an algorithm for the management of bone fragility in diabetic subjects. The authors suggest treating all diabetic subjects with a previous history of hip, vertebral, or with two or more other fragility fractures. They also defend the use of a lower threshold for T-score and a modified version of FRAX to estimate 10-year risk to identify and treat diabetic subjects at increased fracture risk. Our findings, especially on increased death risk after a hip fracture, support these efforts to identify those subjects at increased fracture risk to prevent these from happening.
Individuals with serious chronic illness such as T2DM can experience different relevant events along progression. Assumptions need to be made about dependencies between events. Standard survival analysis involves the analysis of time to an event. Whatever was this event, any other event that precludes the interest event can bias results [41]. Multi-state analysis [19] adds complexity by allowing the analysis of several events for the same individual. Application of multi-state analysis is sparse in T2DM medical literature. Huang et al. [42] used multi-state models to investigate in chronic hepatitis C virus–infected participants the effect of T2DM on the development of hepatocellular carcinoma (HCC) and all-cause mortality after HCC.
Our study has some limitations. The data come from primary care records, no validation of each individual fracture was done, and ICD-10 does not distinguish between traumatic and fragility fractures. However, in SIDIAP, coding of fractures has been compared with hospital databases and shown to be highly specific (> 95% for all fracture sites tested) and moderately sensitive (almost 70% for hip fractures) [23]. This cohort was restricted to individuals older than 65, which imposed a left truncation to the observed time. Also, T2DM patients included prevalent cases, with a variable time of disease duration, a higher prevalence of obesity and cardiovascular risk, and a lower prevalence of use of anti-osteoporosis drugs and calcium + vitamin D supplements. Obesity is a well-known risk factor for the development of T2DM [43], and it is therefore not surprising that it was more commonly seen in our T2DM cohort. Similarly, cardiovascular disease is a known complication related to diabetes and appeared to be more prevalent in the T2DM population [44]. Additionally, a lower prevalence of anti-osteoporosis drugs and calcium/vitamin D supplements has been described in the T2DM previously [45]. This may be related to the underestimation of fracture risk in these subjects and to the lack of evidence available on their anti-fracture effectiveness in diabetic patients [46]. We adjusted for all these factors in our analysis, but yet residual confounding and related bias could persist due to misclassification or incomplete data in the estimation of the hazard ratios for mortality and death according to T2DM status. It is however also true that some of these factors could be in the causal pathway in the association between T2DM and these events, and overadjustment would not be desirable either.
Moreover, a recent work has described that 4 in 5 major fractures recorded in SIDIAP are due to fragility, with higher proportions for hip (92%) and vertebral (88%) fractures [22]. Residual confounding is possible in our study, as some potential risk factors for fracture such as bone mineral density or parental hip fracture history were not available in the database. However, T2DM participants are being associated with a higher bone mineral density [47].
In summary, we conclude that T2DM participants are at higher risk of hip fracture–free death, hip fracture death, and post-hip fracture death, and all these risks are higher in women. Multi-state analysis is a useful technique to analyse, compare, and estimate risks in progression chronic illness. Use of this methodology to assess and compare effectiveness of different therapeutic strategies (on men and women) on all these risks transitions is a must.
References
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, Malanda B (2018) IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 138:271–281. https://doi.org/10.1016/j.diabres.2018.02.023
Lutgers HL, Gerrits EG, Sluiter WJ, Ubink-Veltmaat LJ, Landman GWD, Links TP, Gans ROB, Smit AJ, Bilo HJG Life expectancy in a large cohort of type 2 diabetes patients treated in primary care (ZODIAC-10). Sorensen TIA, ed. PLoS One 2009;4(8):e6817. doi:https://doi.org/10.1371/journal.pone.0006817
Szuszkiewicz-Garcia MM, Davidson JA (2014) Cardiovascular disease in diabetes mellitus. Endocrinol Metab Clin N Am 43(1):25–40. https://doi.org/10.1016/j.ecl.2013.09.001
Narres M, Claessen H, Droste S, Kvitkina T, Koch M, Kuss O, Icks A (2016) The incidence of end-stage renal disease in the diabetic (compared to the non-diabetic) population: a systematic review. Jandeleit-Dahm K, ed. PLoS One 11(1):e0147329. https://doi.org/10.1371/journal.pone.0147329
Salvotelli L, Stoico V, Perrone F, Cacciatori V, Negri C, Brangani C, Pichiri I, Targher G, Bonora E, Zoppini G (2015) Prevalence of neuropathy in type 2 diabetic patients and its association with other diabetes complications: the Verona Diabetic Foot Screening Program. J Diabetes Complicat 29(8):1066–1070. https://doi.org/10.1016/j.jdiacomp.2015.06.014
Olafsdottir E, Andersson DKG, Dedorsson I, Stefánsson E (2014) The prevalence of retinopathy in subjects with and without type 2 diabetes mellitus. Acta Ophthalmol 92(2):133–137. https://doi.org/10.1111/aos.12095
Schaper NC, Van Netten JJ, Apelqvist J, Lipsky BA, Bakker K (2016) International Working Group on the Diabetic Foot. Prevention and management of foot problems in diabetes: a summary guidance for daily practice 2015, based on the IWGDF guidance documents. Diabetes Metab Res Rev 32:7–15. https://doi.org/10.1002/dmrr.2695
Martinez-Laguna D, Tebe C, Javaid MK, Nogues X, Arden NK, Cooper C, Diez-Perez A, Prieto-Alhambra D (2015) Incident type 2 diabetes and hip fracture risk: a population-based matched cohort study. Osteoporos Int 26(2):827–833. https://doi.org/10.1007/s00198-014-2986-9
Dede AD, Tournis S, Dontas I, Trovas G (2014) Type 2 diabetes mellitus and fracture risk. Metabolism. 63(12):1480–1490. https://doi.org/10.1016/j.metabol.2014.09.002
Friedman SM, Mendelson DA (2014) Epidemiology of fragility fractures. Clin Geriatr Med 30(2):175–181. https://doi.org/10.1016/j.cger.2014.01.001
Svedbom A, Hernlund E, Ivergård M et al (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8(1–2):137. https://doi.org/10.1007/s11657-013-0137-0
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. Arch Osteoporos 8(1–2):136. https://doi.org/10.1007/s11657-013-0136-1
Abimanyi-Ochom J, Watts JJ, Borgström F, Nicholson GC, Shore-Lorenti C, Stuart AL, Zhang Y, Iuliano S, Seeman E, Prince R, March L, Cross M, Winzenberg T, Laslett LL, Duque G, Ebeling PR, Sanders KM (2015) Changes in quality of life associated with fragility fractures: Australian arm of the International Cost and Utility Related to Osteoporotic Fractures Study (AusICUROS). Osteoporos Int 26(6):1781–1790. https://doi.org/10.1007/s00198-015-3088-z
LeBlanc KE, Muncie HL, LeBlanc LL (2014) Hip fracture: diagnosis, treatment, and secondary prevention. Am Fam Physician 89(12):945–951 http://www.ncbi.nlm.nih.gov/pubmed/25162161 .Accessed April 22, 2018
Burns A, Younger J, Morris J, Baldwin R, Tarrier N, Pendleton N, Cohen P, Horan M, Banerjee S (2014) Outcomes following hip fracture surgery: a 2-year prospective study. Am J Geriatr Psychiatry 22(8):838–844. https://doi.org/10.1016/j.jagp.2013.01.047
Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, DeBeer J, Bhandari M (2010) Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. Can Med Assoc J 182(15):1609–1616. https://doi.org/10.1503/cmaj.092220
Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M, Felsenthal G, Kenzora J (2000) Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci 55(9):M498–M507 http://www.ncbi.nlm.nih.gov/pubmed/10995047. Accessed April 22, 2018
Roche JJW, Wenn RT, Sahota O, Moran CG (2005) Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 331(7529):1374. https://doi.org/10.1136/bmj.38643.663843.55
Putter H, Fiocco M, Gekus RB (2007) Tutorial in biostatistics: competing risk and multi-state models. Stat Med 26(11):2389–2430. https://doi.org/10.1002/sim.2712
Schmoor C, Schumacher M, Finke J, Beyersmann J (2013) Competing risks and multistate models. Clin Cancer Res 19(1):12–21. https://doi.org/10.1158/1078-0432.CCR-12-1619
Bolíbar B, Fina Avilés F, Morros R, del Mar Garcia-Gil M, Hermosilla E, Ramos R, Rosell M, Rodríguez J, Medina M, Calero S, Prieto-Alhambra D (2012) SIDIAP database: electronic clinical records in primary care as a source of information for epidemiologic research. Med Clin (Barc) 138(14):617–621. https://doi.org/10.1016/j.medcli.2012.01.020
Martinez-Laguna D, Soria-Castro A, Carbonell-Abella C, Orozco-López P, Estrada-Laza P, Nogues X, Díez-Perez A, Prieto-Alhambra D (2017) Validation of fragility fractures in primary care electronic medical records: a population-based study. Reumatol Clin. https://doi.org/10.1016/j.reuma.2017.10.013
Pagès-Castell A, Carbonell-Abella C, Avilés FF et al (2012) Burden of osteoporotic fractures in primary health care in Catalonia (Spain): a population-based study. BMC Musculoskelet Disord 13(1):79. https://doi.org/10.1186/1471-2474-13-79
Tebé C, Martinez-Laguna D, Moreno V, Cooper C, Diez-Perez A, Collins GS, Prieto-Alhambra D (2018) Differential mortality and the excess rates of hip fracture associated with type 2 diabetes: accounting for competing risks in fracture prediction matters. J Bone Miner Res 33(8):1417–1421. https://doi.org/10.1002/jbmr.3435
Beyersmann J, Allignol A, Schumacher M (2012) Competing risks and multistate models with R. https://doi.org/10.1007/978-1-4614-2035-4
Nwaneri C, Cooper H, Bowen-Jones D (2013) Mortality in type 2 diabetes mellitus: magnitude of the evidence from a systematic review and meta-analysis. Br J Diabetes Vasc Dis 13(4):192–207. https://doi.org/10.1177/1474651413495703
Janghorbani M, Van Dam RM, Willett WC, Hu FB (2007) Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 166(5):495–505. https://doi.org/10.1093/aje/kwm106
Jia P, Bao L, Chen H, Yuan J, Liu W, Feng F, Li J, Tang H (2017) Risk of low-energy fracture in type 2 diabetes patients: a meta-analysis of observational studies. Osteoporos Int 28(11):3113–3121. https://doi.org/10.1007/s00198-017-4183-0
Moayeri A, Mohamadpour M, Mousavi SF, Shirzadpour E, Mohamadpour S, Amraei M (2017) Fracture risk in patients with type 2 diabetes mellitus and possible risk factors: a systematic review and meta-analysis. Ther Clin Risk Manag 13:455–468. https://doi.org/10.2147/TCRM.S131945
Dytfeld J, Michalak M (2017) Type 2 diabetes and risk of low-energy fractures in postmenopausal women: meta-analysis of observational studies. Aging Clin Exp Res 29(2):301–309. https://doi.org/10.1007/s40520-016-0562-1
Tebé C, Martinez-Laguna D, Moreno V, Cooper C, Diez-Perez A, Collins GS, Prieto-Alhambra D (2018) Differential mortality and the excess rates of hip fracture associated with type 2 diabetes: accounting for competing risks in fracture prediction matters. J Bone Miner Res 33:1417–1421. https://doi.org/10.1002/jbmr.3435
Khan MA, Hossain FS, Ahmed I, Muthukumar N, Mohsen A (2013) Predictors of early mortality after hip fracture surgery. Int Orthop 37(11):2119–2124. https://doi.org/10.1007/s00264-013-2068-1
Smith T, Pelpola K, Ball M, Ong A, Myint PK (2014) Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing 43(4):464–471. https://doi.org/10.1093/ageing/afu065
Hu F, Jiang C, Shen J, Tang P, Wang Y (2012) Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 43(6):676–685. https://doi.org/10.1016/j.injury.2011.05.017
Haentjens P, Magaziner J, Colón-Emeric CS et al (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152(6):380. https://doi.org/10.7326/0003-4819-152-6-201003160-00008
Muraki S, Yamamoto S, Ishibashi H, Nakamura K (2006) Factors associated with mortality following hip fracture in Japan. J Bone Miner Metab 24(2):100–104. https://doi.org/10.1007/s00774-005-0654-z
Paksima N, Koval KJ, Aharanoff G, Walsh M, Kubiak EN, Zuckerman JD, Egol KA (2008) Predictors of mortality after hip fracture: a 10-year prospective study. Bull NYU Hosp Jt Dis 66(2):111–117 http://www.ncbi.nlm.nih.gov/pubmed/18537780. Accessed April 24, 2018
Palermo A, D’Onofrio L, Eastell R, Schwartz AV, Pozzilli P, Napoli N (2015) Oral anti-diabetic drugs and fracture risk, cut to the bone: safe or dangerous? A narrative review. Osteoporos Int 26(8):2073–2089. https://doi.org/10.1007/s00198-015-3123-0
Zhu Z-N, Jiang Y-F, Ding T (2014) Risk of fracture with thiazolidinediones: an updated meta-analysis of randomized clinical trials. Bone. 68:115–123. https://doi.org/10.1016/j.bone.2014.08.010
Ferrari SL, Abrahamsen B, Napoli N et al (2018) Diagnosis and management of bone fragility in diabetes: an emerging challenge. Osteoporos Int 29(12):2585–2596. https://doi.org/10.1007/s00198-018-4650-2
Kleinbaum DG, Klein M (2012) Survival analysis : a self-learning text. Springer
Huang T-S, Lin C-L, Lu M-J, Yeh CT, Liang KH, Sun CC, Shyu YC, Chien RN (2017) Diabetes, hepatocellular carcinoma, and mortality in hepatitis C-infected patients: a population-based cohort study. J Gastroenterol Hepatol 32(7):1355–1362. https://doi.org/10.1111/jgh.13670
Ley SH, Hamdy O, Mohan V, Hu FB (2014) Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet. 383:1999–2007. https://doi.org/10.1016/S0140-6736(14)60613-9
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HAW (2008) 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 359(15):1577–1589. https://doi.org/10.1056/NEJMoa0806470
Martínez-Laguna D, Reyes C, Carbonell-Abella C et al (2017) Use of drugs for osteoporosis treatment in patients with type 2 diabetes mellitus: population-based cohort study. Rev Osteoporos y Metab Miner 9(4):107–112. https://doi.org/10.4321/S1889-836X2017000400002LK
Vestergaard P, Rejnmark L, Mosekilde L (2011) Are antiresorptive drugs effective against fractures in patients with diabetes? Calcif Tissue Int 88(3):209–214. https://doi.org/10.1007/s00223-010-9450-4
Tuominen JT, Impivaara O, Puukka P, Rönnemaa T (1999) Bone mineral density in patients with type 1 and type 2 diabetes. Diabetes Care 22(7):1196–1200
Acknowledgements
Cristian Tebé and Daniel Prieto-Alhambra designed the study, performed data management and statistical analysis, and drafted the paper. Daniel Martínez-Laguna, Cristina Carbonell-Abella, Carlen Reyes, Victor Moreno, Adolf Diez-Perez, and Gary Collins supervised epidemiological/analytical aspects, participated in the discussion and interpretation of results, and reviewed and critically edited the paper. All authors read the final version and approved submission.
The authors would like to acknowledge the significant contributions of Paloma O’Dogherty (Research Facilitator), Elaine Lilly, Ph.D. (English editor) and the SIDIAP data management team. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR or the Department of Health of the United Kingdom.
Funding
This work was supported by the NIHR Biomedical Research Centre, Oxford. DPA is funded by a National Institute for Health Research Clinician Scientist award (CS-2013-13-012). This article presents independent research funded by the National Institute for Health Research (NIHR). Also, CIBER (Instituto Carlos III) and FEDER funds contributed to the support of the investigation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Cristian Tebé has received lecture fees and honoraria from Boehringer Ingelheim and Amgen outside of the submitted work. Daniel Prieto-Alhambra has received lecture fees and honoraria from Servier, Amgen, and UCB Biopharma SRL outside of the submitted work. Adolf Diez has received lecture fees and honoraria from Amgen, Amgen, Lilly, Gilead, UCB, Roche, Amgen, and EchoLight outside of the submitted work. Daniel Martinez-Laguna, Cristina Carbonell, Carlen Reyes, Victor Moreno, and Gary S Collins declare that they have no conflict of interest.
Disclaimer
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tebé, C., Martínez-Laguna, D., Carbonell-Abella, C. et al. The association between type 2 diabetes mellitus, hip fracture, and post-hip fracture mortality: a multi-state cohort analysis. Osteoporos Int 30, 2407–2415 (2019). https://doi.org/10.1007/s00198-019-05122-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-05122-3