Abstract
Summary
Tc99m-sestamibi dual-time imaging is a standard tool for localization of adenomas/hyperplasia in hyperparathyroidism. We investigated the degree and causes of localization failure among different types of hyperparathyroidism. Pre-operative parathyroid hormone levels and size of the gland were major determinants of Tc99m-sestamibi positivity; 123I scan may be helpful in localization failures.
Introduction
Tc99m-sestamibi dual-time imaging is a standard tool for localization of adenomas/hyperplasia in hyperparathyroidism. However, parathyroid adenomas/hyperplasia has been reported to washout as fast as normal thyroid tissue (“rapid washout”) which may lead to diagnostic failure. We aimed to evaluate the determinants of rapid washout and to determine the role of subtraction imaging for detection of parathyroid adenomas/hyperplasia with rapid washout.
Methods
Retrospective analysis of patients with hyperparathyroidism who have undergone Tc99m-sestamibi dual-time imaging and parathyroid surgery. Rapid washout was correlated to the type of hyperparathyroidism in surgically confirmed cases. Biochemical and pathological data were reviewed.
Results
A total of 135 hyperparathyroidism patients met the inclusion criteria. Ninety-six (72%), 29 (21%), and 10 (7%) had primary, secondary, and tertiary hyperparathyroidisms, respectively. Rapid washout was identified in 28/87 glands (32%), 14/53 glands (26%), and 1/16 glands (6%) with primary, secondary, and tertiary hyperparathyroidisms, respectively. Glands that were positive on late-phase Tc99m-sestamibi scans were significantly large being 1.7 (IQR 1.4–2.3) vs. 1.45 (IQR 1–2) cm (p = 0.003). High parathyroid hormone levels (PTH) were associated with early-phase Tc99m-sestamibi positivity in both primary (p = 0.01) and secondary hyperparathyroidism (p = 0.03) but not with last phase (p = 0.11, p = 0.37, respectively). Correlative imaging with subtraction scintigraphy was positive in 14/16 (87.5%) parathyroid adenomas.
Conclusion
Pre-operative PTH levels and size of the gland were major determinants of Tc99m-sestamibi positivity on early-phase Tc99m-sestamibi scans, whereas size is an independent predictor of late-phase Tc99m-sestamibi positivity. Subtraction scintigraphy might be a useful tool in suspected cases of rapid washout adenomas/hyperplasia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In patients with hyperparathyroidism, apart from finding an experienced parathyroid surgeon, an accurate localization of hyper-functioning parathyroid gland(s) is essential for optimal surgical outcomes [1]. This is especially true in cases with failed initial parathyroid surgery where the presence of ectopic parathyroid glands is a possibility [2]. In general, technetium-99m-hexakis-isobutyl-isonitrite (Tc99m-sestamibi) is the preferred imaging modality of choice for initial pre-operative localization of hyperfunctioning parathyroid tissue in patients with biochemical hyperparathyroidism [3]. Tc99m-sestamibi imaging, first introduced by Coakley et al. in 1989, became rapidly the standard for diagnosis of hyperparathyroidism due to favorable results, superior image quality, better detection sensitivity, and more favorable dosimetry in comparison with previously used 201-thallium [4,5,6].
Tc99m-sestamibi is a monovalent lipophilic cation that passively diffuses through cell membrane with temperature-dependent and non-saturable transport and localizes mostly in the mitochondria due to its negative inner membrane potential [7]. Hence, 90% of Tc99m-sestamibi uptake is associated with mitochondrial load in uptaking cells—the higher the mitochondrial load, the higher the uptake is. The classical single-tracer, dual-phase method with Tc99m-sestamibi has wide-range sensitivity (55–94%) in localizing lesions in hyperparathyroidism [8, 9]. Parathyroid images were typically acquired at approximately 10–20 min and 2 h after administration of Tc99m-sestamibi scan in early and late phases of the scan, respectively. Since Tc99m-sestamibi accumulates in thyroid and parathyroid tissue, the localization of parathyroid adenoma depends on the difference between Tc99m-sestamibi washout form thyroid and parathyroid glands with classic early Tc99m-sestamibi washout from thyroid and late from parathyroid glands. This pattern occurs in 70–75% of cases. However, in some cases, Tc99m-sestamibi washout from parathyroid adenoma/tumor and thyroid gland occurs at the same time. This phenomenon called rapid washout, and it may lead to equivocal findings or diagnostic failure. The exact cause of rapid washout is still unclear, and proposed mechanisms are related to number of mitochondria-rich cells, degree of angiogenesis, percentage of ill formed blood vessels, high mitotic activity, PTH, calcium, phosphorus levels, effects of some medications, and the patients’ weight [10, 11]. In late-phase Tc99m-sestamibi scintigraphy, classic pattern of Tc99m-sestamibi retention by parathyroid adenomas/hyperplasia and washout from thyroid occurs in 60–75% of the cases. However, in some cases, parathyroid adenoma/hyperplasia can be missed due to radiotracer rapid washout. There is very limited literature on rapid Tc99m-sestamibi washout and correlation to the type of hyperparathyroidism.
In this retrospective analysis, we sought to determine the correlation of rapid washout of Tc99m-sestamibi with the type of hyperparathyroidism and the utility of dual radiopharmaceutical acquisition with 123I-Tc99m-sestamibi subtraction imaging for detection of parathyroid adenomas/hyperplasia with rapid washout. We also analyzed the correlation of other biochemical parameters such as calcium and PTH levels with the Tc99m-sestamibi positivity.
Materials and methods
Study design
We conducted a retrospective chart review of adult (≥ 18 years) patients with primary/secondary/tertiary hyperparathyroidism who had Tc99m-sestamibi parathyroid imaging for evaluation and subsequently proceeded to parathyroid surgery at the Washington Hospital Center/Georgetown University from January 1, 2012 to December 31, 2013. One nuclear medicine physician with more than 12-year experience blindly reviewed the Tc99m-sestamibi images. Rapid washout was defined as an area of Tc99m-sestamibi activity on the initial images that did not show any significant retention on delayed images. We also evaluated the utility of 123I-Tc99m-sestamibi subtraction scan in selected patients who had either a negative delayed phase Tc99m-sestamibi or negative scans (both early and delayed phase negative on Tc99m-sestamibi) and correlated the findings with histopathological findings of surgically removed parathyroid glands. The same nuclear medicine physician blindly reviewed the subtraction scan imaging.
Imaging technique
For the parathyroid scanning, a dual-phase single isotope protocol was adopted using 25 mCi of the Tc99m -sestamibi. Initial phase (5–10 min post injection) consisted of pinhole images of the neck in the anterior, right anterior oblique and left anterior oblique projections followed by SPECT-CT of the neck and chest. Delayed phase (2 to 2.5-h post injection) consisted of pinhole images in the anterior, right anterior oblique, and left anterior oblique projections.
In cases of suspected rapid washout and negative Tc99m-sestamibi on both early and delayed phases, patients were re-scanned using the dual isotope subtraction scan on a separate date. For this technique, 200–400 mCi of 123I was administered and patient returned approximately 24 h later for imaging. Pinhole images of the neck in the anterior, right anterior oblique and left anterior oblique projections were performed for 123I imaging. While maintaining the patient in one of the preferred position, Tc99m-sestamibi was injected and pinhole image using a Tc99m window in that preferred projection was performed. Digital subtraction of 123I imaging from Tc99m-sestamibi images was performed utilizing Medview software (Medimage, Ann Arbor, MI, USA). An area of uptake on the Tc99m sestamibi that was not seen on subtraction scan image was considered discordant and indicative of parathyroid adenoma or hyperplasia with rapid washout of Tc99m sestamibi.
Surgical technique and biochemical assays
Surgical treatment included minimally invasive parathyroidectomy, unilateral exploration, bilateral exploration with hemithyroidectomy, and/or near-total thyroidectomy. Thyroid surgery was performed in addition to parathyroid surgery in cases of thyroid nodules (when appropriately indicated). Intraoperative assays of serum PTH before and after tumor resection were performed. We used third-generation PTH assay to measure the PTH levels. A decrease in blood parathyroid hormone level of 50% or more was considered evidence of curative surgery.
Data collection
All available medical records including surgical report, pathology report, and pre- and post-surgical biochemical workups for hyperparathyroidism were reviewed. The diagnosis of parathyroid adenoma or hyperplasia was based primarily on the pathology report. We used the size criteria based on analysis of surgical specimens for accurate analysis of correlation between the adenoma size and Tc99m -sestamibi uptake.
Data analysis
Continuous variables were expressed as mean ± standard error (SE) and categorical and interval variables as frequencies or median and interquartile range (IQR). To compare the groups’ means, t test, ANOVA test, and Brown–Forsythe test were used, appropriately. A two-tailed Student’s t test and Mann–Whitney U test were used for intergroup comparisons of normally distributed and non-normally distributed continuous data, respectively. For categorical variables, we used Pearson’s chi-squared test. All analyses were performed with GraphPad Prism Software version 7.0a (GraphPad Software, San Diego, CA). Difference between groups of patients was considered significant with p < 0.05. The corresponding author’s (K.K) institutional review board approved the study.
Results
A total of 135 hyperparathyroidism patients (males 41; females 94) with 220 adenomas/hyperplasia met the selection criteria. Seventy-two percent of those patients (n = 103 glands in 96 patients) had primary hyperparathyroidism, 21% (n = 94 glands in 29 patients) had secondary hyperparathyroidism, whereas the remaining 7% (n = 23 glands in 10 patients) were diagnosed with tertiary hyperparathyroidism. Baseline characteristics of all the three groups are summarized in Table 1.
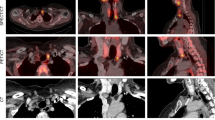
In primary, secondary, and tertiary hyperparathyroidisms, 87/103 (84%), 53/94 (56%), and 16/23 (69%) glands were positive on early-phase Tc99m-sestamibi imaging. Among these patients with positive early-phase Tc99m-sestamibi imaging, negative delayed phase (rapid washout) was identified in 32% (28/87), 26% (14/53), and 6% (1/16) of the glands in primary, secondary, and tertiary hyperparathyroidisms, respectively (primary vs secondary, p = 0.52; primary vs tertiary, p = 0.03; secondary vs tertiary, p = 0.08) (Table 2) (Fig. 1). On the other hand, no uptake of Tc99m sestamibi was identified on both early and delayed phases in 15.5% (16/103), 43.6% (41/94), and 30% (7/23) of the glands in primary, secondary, and tertiary hyperparathyroidisms, respectively (primary vs secondary, p < 0.001).
Frequency of rapid washout in groups of primary, secondary, and tertiary hyperparathyroidisms. Significant difference was noted between primary and tertiary hyperparathyroidisms (p = 0.03), whereas no significant difference was noted between primary and secondary hyperparathyroidisms (p = 0.52) and secondary and tertiary hyperparathyroidisms (p = 0.08)
Median PTH levels for primary, secondary, and tertiary hyperparathyroidisms were 142 pg/ml (IQR 110–240.3), 955 pg/ml (IQR 1865–2448), and 1394 pg/ml (IQR 949–2613), respectively (p < 0.001). In glands with primary hyperparathyroidism, though PTH levels correlated with early-phase Tc99m-sestamibi positivity (p = 0.01), no such correlation between delayed phase and 99mTc-sestamibi positivity was noticed (p = 0.11) (Fig. 2). Similar results were seen in glands with secondary hyperparathyroidism (p = 0.03 in early-phase positivity, p = 0.37 in delayed phase positivity). We could not analyze the correlation in glands with tertiary hyperparathyroidism due to small sample size in the cohort. Among 16 adenomas with rapid washout 99mTc-sestamibi scan, 87.5% (n = 14 adenomas) were discordant on subsequent dual isotope subtraction imaging and diagnostic of parathyroid origin (Table 3). Parathyroid adenomas that were positive on late-phase Tc99m-sestamibi imaging were significantly large being 1.7 cm (IQR 1.4–2.3) vs. 1.45 cm (IQR 1–2) (p = 0.003). Similar size correlation with early-phase Tc99m-sestimibi positivity was noted, with the average size of positive and negative scan being 1.7 cm (IQR 1.3–2.1) and 1.3 cm (IQR 0.8–2), respectively (p = 0.006) (Fig. 3). On the contrary, we did not notice any significant correlation between pre-operative calcium levels and Tc99m-sestamibi radiotracer retention in both early [10.5 mg/dl (IQR 9.45–11.1) vs. 10.75 mg/dl (IQR 9.9–12.58), (p = 0.54)] and late-phase scans [10.4 mg/dl (IQR 9.4–10.7) vs. 10.4 mg/dl (IQR 10–11.3), (p = 0.52)].
Discussion
Tc99m-sestamibi is a standard tool for localization of adenomas/hyperplasia in hyperparathyroidism designed on the difference between thyroid and parathyroid tissue radiotracer washout on early and late phases of scintigraphy. In our study, we found a significant association of type of hyperparathyroidism with rapid washout. Primary hyperparathyroidism had higher percentage of rapid washout (32%) as compared to that of tertiary hyperparathyroidism (6%). This is in contrast from the previous studies that have concluded that rapid washout in adenomas and hyperplasia was in the range of 8–40% and 75%, respectively [12,13,14]. However, it is important to note that the previous studies suffered from very small sample size. One of the plausible explanations for less rapid washout in secondary and tertiary hyperparathyroidism might be the presence of higher number of oxyphil cells in the later [15]. These oxyphil cells contain high number of mitochondria, which have high affinity of Tc99m -sestamibi radiotracer uptake leading to less degree of washout as seen in secondary and tertiary hyperparathyroidism in our study. Chief cells are the predominant cell type in the parathyroid glands of young, healthy subjects, and this number gradually decreases with age as they get transformed into oxyphil cells [16]. This transformation of chief cells to oxyphil cells is known to occur at a higher degree in patients with chronic kidney disease [17]. This may explain the lesser degree of rapid washout in tertiary hyperparathyroidism, which is commonly seen in chronic kidney disease.
In addition, we demonstrated that size of the parathyroid adenoma/hyperplasia is directly related to early- and late-phase uptakes on 99mTc-sestamibi scans—smaller adenomas were more often missed on early and late-phase scans. A study by Neumann et al. [12] has concluded that majority of adenomas that were greater than 600 mg were positive on 99mTc-sestamibi scans and adenomas less than 350 mg were more likely to be missed. Another study has showed that weight of adenoma greater than 1 g was associated with sensitivity greater than 95% [18]. In our study, rather than weight, we used the size criteria as it is easy to determine the size of the adenoma by pre-operative imaging studies. Again, this increased uptake in larger glands might be secondary to the presence of more number of mitochondria rich oxyphilic cells, which is an important factor for Tc99m-sestamibi uptake [19, 20]. We also found that high PTH levels were associated with positive uptake in early-phase Tc99m-sestamibi scans but not in late-phase scans. A small number of oxyphil cells in some adenomas may account for rapid washout [21]. This correlation Tc99m-sestamibi uptake with PTH levels has been proposed by some authors [22,23,24,25,26] but not others [10, 14]. These controversial results of the role of PTH and adenoma size on the uptake and accumulation of radiotracer in parathyroid lesions require the roles of other factors to be taken into consideration. One of such factors is the changes in serum calcium levels. Elevated calcium level has been shown to be significant for Tc99m-sestamibi uptake [27, 28], which again is contradicted by few studies [10, 26]. Some authors have found significant correlation only for early phase of scintigraphy [29]. Some authors debated that increased calcium concentration in mitochondria can block Tc99m-sestamibi uptake by mitochondria [7]. In our study, we did not find any significant association between pre-operative calcium levels and early/late Tc99m-sestamibi uptake. Hence, we think that the uptake of the radiotracer by the parathyroid glands is dependent of multiple factors. For instance, Lane MJ et al., reported that increased tissue perfusion is an important determinant factor in the uptake and retention of radiotracer [30]. In addition, the varied timing of acquisition of late-phase scan might also explain the contradictory results obtained in various studies.
Dual acquisition of Tc99m-sestamibi and 123I has been shown to be better in comparison to single trace dual-phase Tc99m-sestamibi with sensitivity ranging from 70 to 94% depending upon imaging protocols and histology [6, 8, 31,32,33]. Adding 123I as a thyroid tracer is helpful to distinguish thyroid from parathyroid uptake of Tc99m-sestamibi since thyroid nodules can account for about 20–30% of false positive parathyroid scans [32, 34]. This technique can be helpful in detection of adenomas with rapid washout. However, utility of dual Tc99m-sestamibi and 123I acquisition with focus on parathyroid rapid washout has been not investigated thus far, which we did in our study. In our study, dual isotope imaging as an additional diagnostic tool was positive in 87.5% of parathyroid adenomas/hyperplasia with rapid washout but was not effective in cases that were negative on both early- and late-phase Tc99m-sestamibi scintigraphies. The later finding might guide the different approach in terms of dual Tc99m-sestamibi and 123I acquisition application in practice.
Study limitations are inherent to retrospective study design and small sample size in tertiary hyperparathyroidism. However, it is important to note that our study cohort resembles the normal distribution in the incidence of primary, secondary, and tertiary hyperparathyroidisms in general population. Since this was a retrospective chart review, the decision to perform the additional dual isotope scan was made by the individual reviewing the scan rather than the investigator itself. However, during the chart review, all the scans were re-reviewed to assure that the defined criteria of rapid washout were met. The other limitation is lack of data on oxyphil cell count in parathyroid adenomas/hyperplasia scintigraphy. Nonetheless, to the best of our knowledge, in English literature, this is the first study to determine the association of type of hyperparathyroidism and rapid washout in Tc99m-sestimibi imaging.
Conclusions
Higher rates of rapid washout were seen in primary hyperparathyroidism followed by secondary and tertiary kind. Pre-operative PTH levels and size of the gland were major determinants of Tc99m-sestamibi positivity on early-phase Tc99m-sestamibi scans, whereas size is an independent predictor of late-phase Tc99m-sestamibi positivity. Tc99m sestamibi and 123I scintigraphy dual isotope imaging might be useful tool in confirmation of parathyroid origin of the disease in suspected cases of rapid washout. Future studies should include cytological analysis of adenomas/hyperplasia so that the possible explanation of direct association of oxyphil cell count with Tc99m-sestamibi uptake can be answered with accuracy.
References
Michaud L, Balogova S, Burgess A, Ohnona J, Huchet V, Kerrou K, Lefèvre M, Tassart M, Montravers F, Périé S, Talbot J-N (2015) A pilot comparison of (18)F-fluorocholine PET/CT, ultrasonography and (123)I/(99m)Tc-sestaMIBI dual-phase dual-isotope scintigraphy in the preoperative localization of hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism: influence of thyroid anomalies. Medicine 94(41):e1701. https://doi.org/10.1097/MD.0000000000001701
Pitt SC, Sippel RS, Chen H (2009) Secondary and tertiary hyperparathyroidism, state of the art surgical management. Surg Clin North Am 89(5):1227–1239. https://doi.org/10.1016/j.suc.2009.06.011
Kluijfhout WP, Vorselaars WM, Vriens MR, Borel Rinkes IH, Valk GD, de Keizer B (2015) Enabling minimal invasive parathyroidectomy for patients with primary hyperparathyroidism using Tc-99m-sestamibi SPECT-CT, ultrasound and first results of (18)F-fluorocholine PET-CT. Eur J Radiol 84(9):1745–1751. https://doi.org/10.1016/j.ejrad.2015.05.024
Coakley AJ, Kettle AG, Wells CP, O’Doherty MJ, Collins RE (1989) 99Tcm sestamibi—a new agent for parathyroid imaging. Nucl Med Commun 10(11):791–794
Bergenfelz A, Tennvall J, Valdermarsson S, Lindblom P, Tibblin S (1997) Sestamibi versus thallium subtraction scintigraphy in parathyroid localization: a prospective comparative study in patients with predominantly mild primary hyperparathyroidism. Surgery 121(6):601–605
Caveny SA, Klingensmith WC 3rd, Martin WE, Sage-El A, McIntyre RC Jr, Raeburn C, Wolfe P (2012) Parathyroid imaging: the importance of dual-radiopharmaceutical simultaneous acquisition with 99mTc-sestamibi and 123I. J Nucl Med Technol 40(2):104–110. https://doi.org/10.2967/jnmt.111.098400
Lopez AJ, Scheer JK, Leibl KE, Smith ZA, Dlouhy BJ, Dahdaleh NS (2015) Anatomy and biomechanics of the craniovertebral junction. Neurosurg Focus 38(4):E2. https://doi.org/10.3171/2015.1.FOCUS14807
Neumann DR, Obuchowski NA, Difilippo FP (2008) Preoperative 123I/99mTc-sestamibi subtraction SPECT and SPECT/CT in primary hyperparathyroidism. J Nucl Med 49(12):2012–2017. https://doi.org/10.2967/jnumed.108.054858
Chen CC, Holder LE, Scovill WA, Tehan AM, Gann DS (1997) Comparison of parathyroid imaging with technetium-99m-pertechnetate/sestamibi subtraction, double-phase technetium-99m-sestamibi and technetium-99m-sestamibi SPECT. J Nucl Med 38(6):834–839
Cermik TF, Puyan FO, Sezer A, Firat MF, Berkarda S (2005) Relation between Tc-99m sestamibi uptake and biological factors in hyperparathyroidism. Ann Nucl Med 19(5):387–392
Omar WS, Eissa S, Moustafa H, Farag H, Ezzat I, Abdel-Dayem HM (1997) Role of thallium-201 chloride and Tc-99m methoxy-isobutyl-isonitrite (sestaMIBI) in evaluation of breast masses: correlation with the immunohistochemical characteristic parameters (Ki-67, PCNA, Bcl, and angiogenesis) in malignant lesions. Anticancer Res 17(3B):1639–1644
Neumann DR, Esselstyn CB, Maclntyre WJ, Go RT, Obuchowski NA, Chen EQ, Licata AA (1996) Comparison of FDG-PET and sestamibi-SPECT in primary hyperparathyroidism. J Nucl Med 37(11):1809–1815
Lorberboym M, Minski I, Macadziob S, Nikolov G, Schachter P (2003) Incremental diagnostic value of preoperative 99mTc-MIBI SPECT in patients with a parathyroid adenoma. J Nucl Med 44(6):904–908
Arveschoug AK, Bertelsen H, Vammen B, Brochner-Mortensen J (2007) Preoperative dual-phase parathyroid imaging with tc-99m-sestamibi: accuracy and reproducibility of the pinhole collimator with and without oblique images. Clin Nucl Med 32(1):9–12. https://doi.org/10.1097/01.rlu.0000249401.48030.9c
Krause MW, Hedinger CE (1985) Pathologic study of parathyroid glands in tertiary hyperparathyroidism. Hum Pathol 16(8):772–784
Ritter CS, Haughey BH, Miller B, Brown AJ (2012) Differential gene expression by oxyphil and chief cells of human parathyroid glands. J Clin Endocrinol Metab 97(8):E1499–E1505. https://doi.org/10.1210/jc.2011-3366
Christie AC (1967) The parathyroid oxyphil cells. J Clin Pathol 20(4):591–602
Vijayakumar V, Anderson ME (2005) Detection of ectopic parathyroid adenoma by early Tc-99m sestamibi imaging. Ann Nucl Med 19(2):157–159
Sandrock D, Merino MJ, Norton JA, Neumann RD (1993) Ultrastructural histology correlates with results of thallium-201/technetium-99m parathyroid subtraction scintigraphy. J Nucl Med 34(1):24–29
Benard F, Lefebvre B, Beuvon F, Langlois MF, Bisson G (1995) Rapid washout of technetium-99m-MIBI from a large parathyroid adenoma. J Nucl Med 36(2):241–243
Schachter PP, Issa N, Shimonov M, Czerniak A, Lorberboym M (2004) Early, postinjection MIBI-SPECT as the only preoperative localizing study for minimally invasive parathyroidectomy. Arch Surg 139(4):433–437. https://doi.org/10.1001/archsurg.139.4.433
Pons F, Torregrosa JV, Fuster D (2003) Biological factors influencing parathyroid localization. Nucl Med Commun 24(2):121–124. https://doi.org/10.1097/01.mnm.0000057324.59072.67
Ambrosoni P, Heuguerot C, Olaizola I, Acuna G, Fajardo L, Petraglia A, Caorsi H, Lopez J, Kurdian M, Jorgetti V, Aznarez A (1998) Can we use 99mTc-MIBI in functional studies of the parathyroid gland? Nephrol Dial Transplant 13(Suppl 3):33–36
Torregrosa JV, Palomar MR, Pons F, Sabater L, Gilabert R, Llovera J, Fernandez-Cruz L (1998) Has double-phase MIBI scintigraphy usefulness in the diagnosis of hyperparathyroidism? Nephrol DialTransplant 13(Suppl 3):37–40
Hung GU, Wang SJ, Lin WY (2003) Tc-99m MIBI parathyroid scintigraphy and intact parathyroid hormone levels in hyperparathyroidism. Clin Nucl Med 28(3):180–185. https://doi.org/10.1097/01.RLU.0000053529.71776.37
Dugonjic S, Sisic M, Radulovic M, Ajdinovic B (2017) Positive 99mTc-MIBI and the subtraction parathyroid scan are related to intact parathyroid hormone but not to total plasma calcium in primary hyperparathyroidism. Hell J Nucl Med 20(1):46–50. https://doi.org/10.1967/s002449910506
Staudenherz A, Abela C, Niederle B, Steiner E, Helbich T, Puig S, Kaserer K, Becherer A, Leitha T, Kletter K (1997) Comparison and histopathological correlation of three parathyroid imaging methods in a population with a high prevalence of concomitant thyroid diseases. Eur J Nucl Med 24(2):143–149
Melloul M, Paz A, Koren R, Cytron S, Feinmesser R, Gal R (2001) 99mTc-MIBI scintigraphy of parathyroid adenomas and its relation to tumour size and oxyphil cell abundance. Eur J Nucl Med 28(2):209–213
Carpentier A, Jeannotte S, Verreault J, Lefebvre B, Bisson G, Mongeau CJ, Maheux P (1998) Preoperative localization of parathyroid lesions in hyperparathyroidism: relationship between technetium-99m-MIBI uptake and oxyphil cell content. J Nucl Med 39(8):1441–1444
Lane MJ, Desser TS, Weigel RJ, Jeffrey RB Jr (1998) Use of color and power Doppler sonography to identify feeding arteries associated with parathyroid adenomas. AJR Am J Roentgenol 171(3):819–823. https://doi.org/10.2214/ajr.171.3.9725323
Hassler S, Ben-Sellem D, Hubele F, Constantinesco A, Goetz C (2014) Dual-isotope 99mTc-MIBI/123I parathyroid scintigraphy in primary hyperparathyroidism: comparison of subtraction SPECT/CT and pinhole planar scan. Clin Nucl Med 39(1):32–36. https://doi.org/10.1097/RLU.0000000000000272
Hindie E, Melliere D, Jeanguillaume C, Perlemuter L, Chehade F, Galle P (1998) Parathyroid imaging using simultaneous double-window recording of technetium-99m-sestamibi and iodine-123. J Nucl Med 39(6):1100–1105
Neumann DR, Esselstyn CB Jr, Madera A, Wong CO, Lieber M (1998) Parathyroid detection in secondary hyperparathyroidism with 123I/99mTc-sestamibi subtraction single photon emission computed tomography. J Clin Endocrinol Metab 83(11):3867–3871. https://doi.org/10.1210/jcem.83.11.5241
Jorna FH, Jager PL, Que TH, Lemstra C, Plukker JT (2007) Value of 123I-subtraction and single-photon emission computed tomography in addition to planar 99mTc-MIBI scintigraphy before parathyroid surgery. Surg Today 37(12):1033–1041. https://doi.org/10.1007/s00595-007-3550-4
Acknowledgements
The work was presented as a poster at Endocrine Society’s annual meeting proceedings 2017, Orlando, FL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The corresponding author’s (K.K) institutional review board approved the study.
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kushchayeva, Y., Tella, S., Kushchayev, S. et al. Comparison of hyperparathyroidism types and utility of dual radiopharmaceutical acquisition with Tc99m sestamibi and 123I for localization of rapid washout parathyroid adenomas. Osteoporos Int 30, 1051–1057 (2019). https://doi.org/10.1007/s00198-019-04846-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-04846-6