Abstract
Summary
Among 365 Hertfordshire Cohort Study participants (aged 59–71 years at baseline), higher adiponectin and adiponectin to leptin ratios were associated with lower baseline lumbar spine and femoral neck bone mineral density (BMD). Lower IL-10 was associated with accelerated decline in lumbar spine BMD. This suggests that bone health can be influenced by changes in immune phenotype and alterations in adipokine homeostasis.
Introduction
The aim of this study was to examine the association between indices of inflammation and BMD in a population-based cohort of older adults in the UK.
Methods
Analyses were based on a sample of 194 men and 171 women of the Hertfordshire Cohort Study (community-living, older adults). Dual energy X-ray absorptiometry (DXA) was performed at the lumbar spine and proximal femur at baseline and repeated at a median of 4.5 years (inter-quartile range 3.6 to 5.2). Inflammatory markers (CRP, TNF, IL-1β, IL-6, IL-8, IL-10, adiponectin and leptin) were ascertained at baseline using enzyme-linked immunosorbent assay (ELISA) techniques and Bio-Plex Pro Assays. Gender-adjusted linear regression was used to examine the associations between markers of inflammation and outcomes with and without adjustment for anthropometric and lifestyle factors.
Results
The mean (SD) ages at baseline were 64.4 (2.5) and 66.5 (2.7) years for men and women respectively. Higher levels of adiponectin and adiponectin to leptin ratios were each associated with lower baseline lumbar spine and femoral neck BMD in gender-adjusted (p < 0.01) and fully adjusted (p < 0.05) analyses. Lower levels of IL-10 and TNF were each associated with accelerated decline in lumbar spine BMD in both gender-adjusted (p ≤ 0.05) and fully adjusted (p < 0.05) analyses.
Conclusions
In a cohort of older adults, high levels of adiponectin and adiponectin to leptin ratios were both associated with lower BMD at the lumbar spine and femoral neck at baseline, and lower IL-10 was associated with accelerated decline in BMD at the lumbar spine. This adds weight to the theory that bone health can be influenced by changes in immune phenotype and alterations in adipokine homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a condition characterised by demineralisation of bone with a subsequent increased risk of fracture and is a major global health concern [1]. It is particularly common in women, affecting an estimated 22 million European women over the age of 50 [2]. Risk factors for osteoporosis include older age, family history, low body mass index, smoking, excessive alcohol consumption and corticosteroid usage [3].
Although inconsistent, there is evidence that indolent, low-level inflammation leads to cellular senescence, impaired DNA repair and biological ageing. Studies have even related inflammation to indices of musculoskeletal health. Experimentally, these have demonstrated a role of pro-inflammatory mediators (including TNF, IL-1β and IL-6) in the alteration of bone structure [4], via the inhibition of osteoblasts. With regard to clinical indices, population studies have demonstrated varying relationships between incident fracture and CRP [5,6,7,8,9,10,11], TNF [6, 9, 12], IL-6 [6, 9, 12, 13] and IL-10 [6] and between bone mineral density (BMD) and CRP [6, 7, 10, 14,15,16], TNF [6, 16, 17], IL-6 [6, 16,17,18], IL-10 [6] and adipokines including adiponectin and leptin [19,20,21,22].
Adipokines, in addition to elements of the inflammatory cytokine cascade, have been shown to have marked immune homeostatic effects. Adiponectin manifests an anti-inflammatory state via inhibition of macrophage activation and subsequently lower levels of TNF and interferon-γ and increased levels of IL-10 and IL-1RA [23]. Leptin possesses a more pro-inflammatory profile, leading to higher levels of TNF, IL-6 and IL-12 [24] with these inflammatory mediators having effects on the musculoskeletal system downstream. Previous studies have investigated adipokine relationships with bone turnover markers [25] and bone mineral density (BMD) in pre- and post-menopausal women [21]. However, literature on the longitudinal relationships between inflammatory markers and BMD in older populations is lacking.
The Hertfordshire Cohort Study (HCS) provides an ideal opportunity to address this issue, in consort with examination of the longitudinal relationship between BMD and inflammatory markers, in a population-based cohort of community-dwelling older men and women in the UK (26).
The objective of this current analysis was to examine the associations between baseline markers of inflammation and level and change in total lumbar spine and femoral neck bone mineral density (BMD) among HCS participants.
Methods
The Hertfordshire Cohort Study
The HCS comprises 1579 men and 1418 women born in Hertfordshire between 1931 and 1939 and who still lived there in 1998 to 2004 when they completed a baseline home interview and research clinic for detailed characterisation of their socio-demographic, lifestyle and clinical characteristics; the study has been described in detail previously [26].
Smoking status, weekly alcohol consumption and customary level of physical activity (Dallosso questionnaire [27]) were ascertained by a nurse-administered questionnaire at the home interview. A ‘prudent diet’ score was derived from a food-frequency questionnaire using principal component analysis; higher scores reflect healthier diets [28]. Details of all prescription and over-the-counter medications currently taken were coded according to the British National Formulary; the number of systems medicated was used as a marker of comorbidity.
Investigations conducted at the baseline clinic included measurement of height (using a Harpenden pocket stadiometer, Chasmors Ltd., London, UK) and weight (on a SECA floor scale, Chasmors Ltd., London, UK). Blood samples were taken and serum was aliquoted and stored at − 80 °C. Dual energy X-ray absorptiometry (DXA) at the lumbar spine and proximal femur was performed using a Hologic QDR 4500 instrument (Vertec Scientific, Reading, UK) to ascertain total lumbar spine and total femoral neck BMD. Measurement precision error of this device has been described previously [29]. In 2004–2005, 642 men and women (73% of those invited) agreed to participate in a clinical follow-up study during which medication use was reassessed: DXA measurements were repeated for 568 participants.
Ascertainment of baseline inflammatory markers
Baseline posterity samples were available for 365 of the 568 participants. High sensitivity C-reactive protein (hs-CRP) levels were measured by ELISA using a commercial kit (IBL International, Hamburg, Germany) according to manufacturer’s instructions. A multiplex-based assay for the cytokines IL-1β, IL-6, IL-10, IL-8 and TNF (Bio-Rad Laboratories, Munich, Germany) was performed according to manufacturer’s instructions. Data acquisition and analysis was conducted using Bio-Plex Manager software version 6.0. Intra-assay coefficients of variation (CV %) ranged from 7.15 to 13.89.
Serum adiponectin (serum diluted 1:5000) and leptin (serum diluted 1:2000) were assessed separately by solid phase sandwich ELISA (R&D Systems, Abingdon, UK). Data analysis was performed using GraphPad Prism software (GraphPad Software Ltd., USA).
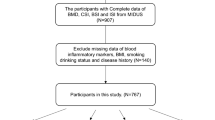
The analysis sample for this paper comprised the 365 participants who had non-missing data for at least one of the inflammatory markers considered and who had complete data for lumbar spine and femoral neck BMD at baseline and follow-up.
The HCS study had ethical approval from the Hertfordshire and Bedfordshire Local Research Ethics Committee and all participants gave written informed consent to participate in the study and for their health records to be accessed in the future. Investigations were conducted in accordance with the principles expressed in the Declaration of Helsinki.
Statistical methods
Height and weight were highly correlated (r = 0.46, p < 0.001 for men; r = 0.38, p < 0.001 for women); to avoid multi-collinearity problems, a sex-specific standardised residual of weight-adjusted-for-height was derived. Smoking status was categorised into ever smokers and never smokers. Conditional change in total lumbar spine and femoral neck BMD was characterised by the residuals obtained after estimating sex-specific linear regression models for measures at follow-up on measures at baseline with adjustment for individual follow-up duration; this measure of residual change is independent of baseline level.
Data were described using summary statistics. Apart from IL-8, all inflammatory markers were highly positively skewed and were log-transformed. Linear regression was used to examine the association between each baseline inflammatory marker and both baseline level and change in femoral neck and lumbar spine BMD. Gender-adjusted and fully adjusted models accounting for gender, baseline age, height, weight-for-height, smoking history, alcohol consumption, prudent diet score, physical activity and use of hormone replacement therapy were implemented. Models for conditional change in BMD were additionally adjusted for bisphosphonate use at follow-up (no participants used bisphosphonates at baseline).
To ensure comparability of effect sizes, sex-specific standard deviation scores were derived for inflammatory markers and outcomes and used in models. Owing to modest sample size, men and women were pooled and analyses were adjusted for gender (interaction effects between gender and the inflammatory markers were non-significant in gender-adjusted models); p < 0.05 was regarded as statistically significant. Analyses were conducted using Stata, release 13.
Results
Participant characteristics
Characteristics of the 365 HCS participants who were included in the analysis sample are presented in Table 1. Mean (SD) age at HCS baseline was 64.4 (2.5) and 66.5 (2.7) years among men and women respectively. Median (inter-quartile range) time between bone scans was 5.2 (4.8, 5.6) years among men and 3.6 (3.1, 4.0) years among women. On average, men had higher BMD than women at the lumbar spine and femoral neck; both sexes gained BMD at the lumbar spine; and women lost BMD at the femoral neck but there was no change at this site for men.
The proportion of participants who were of manual social class did not differ significantly between the analysis sample and the 2632 participants who attended the HCS baseline clinic but were not included in the analysis sample.
Table 3 presents the Pearson correlations between the markers of inflammation. TNF was moderately correlated with IL-1β, IL-6 and IL-10 (0.22 < = r < = 0.32, p < 0.001) and negatively correlated with IL-8 (r = − 0.25, p < 0.001). IL-1β was moderately correlated with IL-10 (r = 0.26, p < 0.001).
Relationships between markers of inflammation and lumbar spine and femoral neck BMD at baseline
The associations between each inflammatory marker and both level and change in lumbar spine and femoral neck BMD are presented in Table 2 and Fig. 1. Lower levels of leptin and higher levels of IL-1β, adiponectin and adiponectin to leptin ratios were each associated with lower baseline lumbar spine and femoral neck BMD; associations for adiponectin and adiponectin to leptin ratios were robust in fully adjusted analyses. For example, an SD increase in adiponectin was associated with a mean reduction in baseline lumbar spine BMD of 0.11 (95% CI 0.01, 0.21) SDs in fully adjusted analyses; reductions regarding femoral neck BMD were similar for this marker. In gender-adjusted analyses, higher levels of TNF and lower levels of hs-CRP were also associated with lower femoral neck BMD but these were attenuated by full adjustment.
SD difference (95% CI) in level and conditional change in total lumbar spine and total femoral neck BMD per SD increase in inflammatory marker. Separate linear regression models for each inflammatory predictor were adjusted for the following baseline predictors: gender, age, height, weight-for-height residual, smoking history (ever vs never), alcohol consumption, diet quality, physical activity and use of hormone replacement therapy. Conditional change models were also adjusted for bisphosphonate use at follow-up. Adjusted p values are presented. Conditional change measures are independent of baseline level; a positive estimate illustrates that the inflammatory marker was associated with reduced loss of BMD over time and a negative estimate reflects accelerated loss. Ad:lep, adiponectin to leptin ratio
Longitudinal relationships between markers of inflammation and conditional change in lumbar spine and femoral neck BMD
Lower levels of TNF and IL-10 and higher levels of IL-8 were each associated with accelerated decline in lumbar spine BMD (Table 2); associations regarding TNF and IL-10 were robust in fully adjusted analysis (Table 2 and Fig. 1). For example, in fully adjusted analyses, an SD decrease in IL-10 was associated with accelerated loss of lumbar spine BMD of 0.10 (95% CI 0.00, 0.20) SD scores. No inflammatory markers were associated with change in femoral neck BMD.
Discussion
Using data from the Hertfordshire Cohort Study, we have examined associations between baseline inflammatory markers and level, and rate of loss, of lumbar spine and femoral neck BMD. Higher adiponectin and adiponectin to leptin ratios (a ratio which purports to assess the inflammatory balance of the adipokine profile [23, 24]) were associated with lower baseline BMD at both the lumbar spine and femoral neck; determinants of accelerated decline in lumbar spine BMD included lower IL-10. Fully adjusted associations were little altered when additionally adjusted for number of systems medicated (a marker of comorbidity). No baseline inflammatory markers were associated with change in femoral neck BMD.
Our study has many strengths. First, the HCS provides a detailed characterisation of community-dwelling older people in England and measurements were carried out according to strict protocols by trained fieldworkers. Moreover, the HCS database is managed by an experienced multi-disciplinary team. Second, we examined the associations between a wide panel of inflammatory markers and components of bone health, relationships which have not been previously investigated in an elderly, UK population.
Our study has some limitations. First, a healthy responder bias has, unsurprisingly, been identified in HCS [26]. However, HCS participant characteristics are nonetheless broadly comparable with those of participants in the nationally representative Health Survey for England [26]. Furthermore, our analyses were internal so unless the associations of interest differed systematically among subgroups of the population, no major bias should have been introduced. Second, the inflammatory markers and outcomes contained missing values and to maximise statistical power, participants were included in the analysis sample if they had non-missing values for at least one inflammatory marker and bone outcome. Third, the measurement of serum measures of inflammation at a single time-point may be vulnerable to the influence of concurrent illness. However, due to the organisation of the research clinics, it is unlikely that participants would have attended if they were unwell. This is supported by the fact that the majority of inflammatory markers were within the normal range. Additionally, baseline inflammatory marker measurements have been successfully used to predict cardiovascular risk [30]. Fourthly, the sample size used for analysis was reasonably small and due to the number of statistical tests performed, we cannot exclude the possibility of chance findings. However, the results reported in this study are broadly consistent with the wider literature [6, 16, 20, 31].
The immune system and inflammatory response changes across the life course. This alteration is suspected to occur secondary to overloading of the immune system with activated, primed macrophages, lymphocytes and dendritic cells in response to continuous stress and inflammation. This results in a chronic, low-grade inflammatory state [32] with changes in the pro- and anti-inflammatory cytokine, chemokine landscape [33, 34]. Ageing can also effect bone with an increasingly prevalent pro-osteoclastic environment leading to increased bone resorption and a subsequent propensity to fracture [35].
Our current analysis has identified associations between adiponectin to leptin ratio and baseline bone mineral density at both femora and vertebrae. Adipocytes and osteoblasts share a common progenitor, and thus, adipokine cross-talk between the two resultant tissues is not surprising. Previous studies have demonstrated an increased risk of incident fracture with increasing adiponectin level in women [31] and in an elderly US population of men [20].The influence of adipokines on BMD has been investigated in a younger, female, Korean population by Haam and colleagues [21] who found a negative association between leptin concentration with non-vertebral BMD and a positive association between high-molecular weight (HMW) adiponectin and total hip BMD in pre-menopausal women but a negative association of HMW adiponectin with BMD at both femoral and vertebral sites in post-menopausal women. In addition, an association between higher adiponectin and accelerated loss of hip areal BMD has been reported previously [22]; in our study, higher adiponectin was only associated with lower baseline lumbar spine and lower femoral neck BMD. Our study therefore contributes significantly to the adipokinetic literature as an investigation of a mixed-sex population of older adults, which uses BMD as the outcome measure and highlights the relevance of the adiponectin to leptin ratio, rather than considering the levels of each mediator in isolation. Our current study adds to previous work that we have published on the effect of adipose tissue on the bone [36].
Our study also suggested associations between inflammatory cytokines and baseline BMD, including associations between higher levels of IL-1β and TNF and lower levels of hs-CRP, in relation to lower BMD, although these results were not robust to adjustment. Interleukin-1β is a profligate pro-inflammatory cytokine. Although short-term release of IL-1β is necessary for fracture healing, long-term exposure can lead to bone loss and has been associated with osteoporosis [37]. In vitro studies have shown that IL-1β causes osteoclastogenesis via induction of receptor activator of nuclear kappa-Β ligand (RANKL) and inhibition of osteoprotegerin [38] and reduces osteoblast migration [39]. Our finding is therefore in keeping with the literature and supports evidence for the influence of the inflammatory cascade on bone minerality and structure.
The associations that we identified between hs-CRP and TNF and baseline DXA outcomes may reflect the heterogeneous relationships between both mediators and bone mineral density in previous investigations [6, 7, 14,15,16,17, 19]. The ubiquity of these inflammatory markers, and their common release (and thus presence in sera) in response to inflammatory stimuli of any aetiology, is likely the cause. Further tissue-specific work in vivo is required to delineate associations with bone density.
In this current study, we identified relationships between the inflammatory markers IL-10, IL-8 and TNF and change in BMD but only at the lumbar spine and not the femoral neck. This may be explained by the greater degree of trabeculation in the lumbar spine, increased metabolic activity and, thus, increased vulnerability to manipulation by inflammatory mediators. Interleukin-10 is primarily an anti-inflammatory cytokine which dampens T helper 1 cell activity and lipopolysaccharide-stimulated immune activation. Work in animal models has demonstrated that IL-10 deficiency results in adverse bone outcomes including the development of osteopenia, attenuated bone formation and phenotypically long, fragile bones [40]. This is likely through the inhibition of osteoclastogenesis and promotion of osteoblastic differentiation [41]. These cellular effects are supported by findings in human studies relating IL-10 haplotypes with reduced BMD in post-menopausal females [42].
Interleukin-8 plays a primary role in neutrophil chemotaxis as well as correlating positively with RANKL. Our study suggested some association between higher levels of IL-8 and accelerated decline at the lumbar spine. This is in keeping with an adverse effect of inflammation on BMD, though this finding was not robust in the fully adjusted model. It was surprising that lower levels of TNF were associated with accelerated decline in lumbar spine BMD in our study; indeed, this is at odds with a previous finding in a smaller study of older adults in Australia which showed that higher levels of TNF predicted greater decline in BMD [16]. Therefore, we cannot rule out the possibility that this result is a chance finding in our study. However, another study in a group of elderly males in Sweden found no association between TNF level and BMD [6]. Further studies are required to clarify this relationship, though it may be explained by increased spinal degeneration and osteoarthritis; associations between higher TNF and accelerated loss of knee cartilage have been reported previously [43]. Osteoarthritis (OA) is associated with raised intra-articular TNF; thus, a serum increase in TNF may be representative of an increased burden of OA.
In conclusion, we have demonstrated an association between higher levels of adiponectin and adiponectin to leptin ratios and lower baseline bone mineral density. Lower levels of the anti-inflammatory cytokine IL-10 were associated with loss of BMD in longitudinal follow-up. Further work, particularly tissue-specific, in vivo experimentation, is required to elucidate the role of inflammatory mediators at the bone-inflammation interface.
References
Harvey N, Dennison E, Cooper C (2010) Osteoporosis: impact on health and economics. Nat Rev Rheumatol 6(2):99–105. https://doi.org/10.1038/nrrheum.2009.260
Dawson A, Dennison E (2016) Measuring the musculoskeletal aging phenotype. Maturitas 93:13–17. https://doi.org/10.1016/j.maturitas.2016.04.014
Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N, Cauley JA, Compston JE, Dawson-Hughes B, El-Hajj Fuleihan G, Johansson H, Leslie WD, Lewiecki EM, Luckey M, Oden A, Papapoulos SE, Poiana C, Rizzoli R, Wahl DA, McCloskey EV (2011) Interpretation and use of FRAX in clinical practice. Osteoporos Int 22(9):2395–2411. https://doi.org/10.1007/s00198-011-1713-z
Boyle WJ, Simonet WS, Lacey DL (2003) Osteoclast differentiation and activation. Nature 423(6937):337–342. https://doi.org/10.1038/nature01658
Nakamura K, Saito T, Kobayashi R, Oshiki R, Oyama M, Nishiwaki T, Nashimoto M, Tsuchiya Y (2011) C-reactive protein predicts incident fracture in community-dwelling elderly Japanese women: the Muramatsu study. Osteoporos Int 22(7):2145–2150. https://doi.org/10.1007/s00198-010-1425-9
Cauley JA, Barbour KE, Harrison SL, Cloonan YK, Danielson ME, Ensrud KE, Fink HA, Orwoll ES, Boudreau R (2016) Inflammatory markers and the risk of hip and vertebral fractures in men: the osteoporotic fractures in men (MrOS). J Bone Miner Res 31(12):2129–2138. https://doi.org/10.1002/jbmr.2905
Schett G, Kiechl S, Weger S, Pederiva A, Mayr A, Petrangeli M, Oberhollenzer F, Lorenzini R, Redlich K, Axmann R, Zwerina J, Willeit J (2006) High-sensitivity C-reactive protein and risk of nontraumatic fractures in the Bruneck study. Arch Intern Med 166(22):2495–2501. https://doi.org/10.1001/archinte.166.22.2495
Pasco JA, Kotowicz MA, Henry MJ, Nicholson GC, Spilsbury HJ, Box JD, Schneider HG (2006) High-sensitivity C-reactive protein and fracture risk in elderly women. JAMA 296(11):1353–1355. https://doi.org/10.1001/jama.296.11.1353
Cauley JA, Danielson ME, Boudreau RM, Forrest KY, Zmuda JM, Pahor M, Tylavsky FA, Cummings SR, Harris TB, Newman AB (2007) Inflammatory markers and incident fracture risk in older men and women: the Health Aging and Body Composition Study. J Bone Miner Res 22(7):1088–1095. https://doi.org/10.1359/jbmr.070409
Ishii S, Cauley JA, Greendale GA, Crandall CJ, Danielson ME, Ouchi Y, Karlamangla AS (2013) C-reactive protein, bone strength, and nine-year fracture risk: data from the Study of Women’s Health Across the Nation (SWAN). J Bone Miner Res 28(7):1688–1698. https://doi.org/10.1002/jbmr.1915
Dahl K, Ahmed LA, Joakimsen RM, Jorgensen L, Eggen AE, Eriksen EF, Bjornerem A (2015) High-sensitivity C-reactive protein is an independent risk factor for non-vertebral fractures in women and men: the Tromso Study. Bone 72:65–70. https://doi.org/10.1016/j.bone.2014.11.012
Barbour KE, Boudreau R, Danielson ME, Youk AO, Wactawski-Wende J, Greep NC, LaCroix AZ, Jackson RD, Wallace RB, Bauer DC, Allison MA, Cauley JA (2012) Inflammatory markers and the risk of hip fracture: the Women’s Health Initiative. J Bone Miner Res 27(5):1167–1176. https://doi.org/10.1002/jbmr.1559
Barbour KE, Lui LY, Ensrud KE, Hillier TA, LeBlanc ES, Ing SW, Hochberg MC, Cauley JA (2014) Inflammatory markers and risk of hip fracture in older white women: the study of osteoporotic fractures. J Bone Miner Res 29(9):2057–2064. https://doi.org/10.1002/jbmr.2245
Ganesan K, Teklehaimanot S, Tran TH, Asuncion M, Norris K (2005) Relationship of C-reactive protein and bone mineral density in community-dwelling elderly females. J Natl Med Assoc 97(3):329–333
Koh JM, Khang YH, Jung CH, Bae S, Kim DJ, Chung YE, Kim GS (2005) Higher circulating hsCRP levels are associated with lower bone mineral density in healthy pre- and postmenopausal women: evidence for a link between systemic inflammation and osteoporosis. Osteoporos Int 16(10):1263–1271. https://doi.org/10.1007/s00198-005-1840-5
Ding C, Parameswaran V, Udayan R, Burgess J, Jones G (2008) Circulating levels of inflammatory markers predict change in bone mineral density and resorption in older adults: a longitudinal study. J Clin Endocrinol Metab 93(5):1952–1958. https://doi.org/10.1210/jc.2007-2325
Lin CC, Li TC, Liu CS, Yang CW, Lin CH, Hsiao JH, Meng NH, Lin WY, Liao LN, Li CI, Wu FY (2016) Associations of TNF-alpha and IL-6 polymorphisms with osteoporosis through joint effects and interactions with LEPR gene in Taiwan: Taichung Community Health Study for Elders (TCHS-E). Mol Biol Rep 43(10):1179–1191. https://doi.org/10.1007/s11033-016-4037-4
Scheidt-Nave C, Bismar H, Leidig-Bruckner G, Woitge H, Seibel MJ, Ziegler R, Pfeilschifter J (2001) Serum interleukin 6 is a major predictor of bone loss in women specific to the first decade past menopause. J Clin Endocrinol Metab 86(5):2032–2042. https://doi.org/10.1210/jcem.86.5.7445
Lim HS, Park YH, Kim SK (2016) Relationship between serum inflammatory marker and bone mineral density in healthy adults. J Bone Metab 23(1):27–33. https://doi.org/10.11005/jbm.2016.23.1.27
Barbour KE, Zmuda JM, Boudreau R, Strotmeyer ES, Horwitz MJ, Evans RW, Kanaya AM, Harris TB, Bauer DC, Cauley JA (2011) Adipokines and the risk of fracture in older adults. J Bone Miner Res 26(7):1568–1576. https://doi.org/10.1002/jbmr.361
Haam JH, Kim YS, Kim MJ, Koo HS, Kim HY, Kim HJ, Park KH, Joo NS, Park KC (2016) A cross-sectional study of the association between adipokine levels and bone mineral density according to obesity and menopausal status in Korean women. J Bone Miner Metab 35:642–648. https://doi.org/10.1007/s00774-016-0801-8
Barbour KE, Zmuda JM, Boudreau R, Strotmeyer ES, Horwitz MJ, Evans RW, Kanaya AM, Harris TB, Cauley JA (2012) The effects of adiponectin and leptin on changes in bone mineral density. Osteoporos Int 23(6):1699–1710. https://doi.org/10.1007/s00198-011-1768-x
Tilg H, Moschen AR (2006) Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol 6(10):772–783. https://doi.org/10.1038/nri1937
Procaccini C, De Rosa V, Galgani M, Carbone F, La Rocca C, Formisano L, Matarese G (2013) Role of adipokines signaling in the modulation of T cells function. Front Immunol 4:332. https://doi.org/10.3389/fimmu.2013.00332
Labouesse MA, Gertz ER, Piccolo BD, Souza EC, Schuster GU, Witbracht MG, Woodhouse LR, Adams SH, Keim NL, Van Loan MD (2014) Associations among endocrine, inflammatory, and bone markers, body composition and weight loss induced bone loss. Bone 64:138–146. https://doi.org/10.1016/j.bone.2014.03.047
Syddall H, Sayer AA, Dennison E, Martin H, Barker D, Cooper C (2005) Cohort profile: the Hertfordshire cohort study. Int J Epidemiol 34(6):1234–1242
Dallosso HM, Morgan K, Bassey EJ, Ebrahim SB, Fentem PH, Arie TH (1988) Levels of customary physical activity among the old and the very old living at home. J Epidemiol Community Health 42(2):121–127
Robinson S, Syddall H, Jameson K, Batelaan S, Martin H, Dennison EM, Cooper C, Sayer AA, Group HS (2009) Current patterns of diet in community-dwelling older men and women: results from the Hertfordshire Cohort Study. Age Ageing 38:594–599
Gale CR, Dennison EM, Edwards M, Sayer AA, Cooper C (2012) Symptoms of anxiety or depression and risk of fracture in older people: the Hertfordshire Cohort Study. Arch Osteoporos 7:59–65. https://doi.org/10.1007/s11657-012-0080-5
Emberson JR, Whincup PH, Morris RW, Walker M, Lowe GD, Rumley A (2004) Extent of regression dilution for established and novel coronary risk factors: results from the British Regional Heart Study. Eur J Cardiovasc Prev Rehabil 11(2):125–134
Johansson H, Oden A, Lerner UH, Jutberger H, Lorentzon M, Barrett-Connor E, Karlsson MK, Ljunggren O, Smith U, McCloskey E, Kanis JA, Ohlsson C, Mellstrom D (2012) High serum adiponectin predicts incident fractures in elderly men: osteoporotic fractures in men (MrOS) Sweden. J Bone Miner Res 27(6):1390–1396. https://doi.org/10.1002/jbmr.1591
Franceschi C, Garagnani P, Vitale G, Capri M, Salvioli S (2016) Inflammaging and ‘Garb-aging’. Trends Endocrinol Metab 28:199–212. https://doi.org/10.1016/j.tem.2016.09.005
Franceschi C, Bonafe M, Valensin S, Olivieri F, De Luca M, Ottaviani E, De Benedictis G (2000) Inflamm-aging. An evolutionary perspective on immunosenescence. Ann N Y Acad Sci 908:244–254
Gerli R, Monti D, Bistoni O, Mazzone AM, Peri G, Cossarizza A, Di Gioacchino M, Cesarotti ME, Doni A, Mantovani A, Franceschi C, Paganelli R (2000) Chemokines, sTNF-Rs and sCD30 serum levels in healthy aged people and centenarians. Mech Ageing Dev 121(1–3):37–46
Demontiero O, Gunawardene P, Duque G (2014) Postoperative prevention of falls in older adults with fragility fractures. Clin Geriatr Med 30(2):333–347. https://doi.org/10.1016/j.cger.2014.01.018
Cole ZA, Harvey NC, Kim M, Ntani G, Robinson SM, Inskip HM, Godfrey KM, Cooper C, Dennison EM (2012) Increased fat mass is associated with increased bone size but reduced volumetric density in pre pubertal children. Bone 50(2):562–567. https://doi.org/10.1016/j.bone.2011.05.005
Pacifici R, Rifas L, Teitelbaum S, Slatopolsky E, McCracken R, Bergfeld M, Lee W, Avioli LV, Peck WA (1987) Spontaneous release of interleukin 1 from human blood monocytes reflects bone formation in idiopathic osteoporosis. Proc Natl Acad Sci U S A 84(13):4616–4620
Nakashima T, Kobayashi Y, Yamasaki S, Kawakami A, Eguchi K, Sasaki H, Sakai H (2000) Protein expression and functional difference of membrane-bound and soluble receptor activator of NF-kappaB ligand: modulation of the expression by osteotropic factors and cytokines. Biochem Biophys Res Commun 275(3):768–775. https://doi.org/10.1006/bbrc.2000.3379
Hengartner NE, Fiedler J, Ignatius A, Brenner RE (2013) IL-1beta inhibits human osteoblast migration. Mol Med 19:36–42. https://doi.org/10.2119/molmed.2012.00058
Dresner-Pollak R, Gelb N, Rachmilewitz D, Karmeli F, Weinreb M (2004) Interleukin 10-deficient mice develop osteopenia, decreased bone formation, and mechanical fragility of long bones. Gastroenterology 127(3):792–801
Zhang Q, Chen B (2014) Interleukin-10 inhibits bone resorption: a potential therapeutic strategy in periodontitis and other bone loss diseases. 2014:284836. https://doi.org/10.1155/2014/284836
Park BL, Han IK, Lee HS, Kim LH, Kim SJ, Shin JS, Kim SY, Shin HD (2004) Association of interleukin 10 haplotype with low bone mineral density in Korean postmenopausal women. J Biochem Mol Biol 37(6):691–699
Stannus O, Jones G, Cicuttini F, Parameswaran V, Quinn S, Burgess J, Ding C (2010) Circulating levels of IL-6 and TNF-alpha are associated with knee radiographic osteoarthritis and knee cartilage loss in older adults. Osteoarthr Cartil 18(11):1441–1447. https://doi.org/10.1016/j.joca.2010.08.016
Funding
This research was funded by the Medical Research Council and the University of Southampton, UK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Fuggle, N.R., Westbury, L.D., Syddall, H.E. et al. Relationships between markers of inflammation and bone density: findings from the Hertfordshire Cohort Study. Osteoporos Int 29, 1581–1589 (2018). https://doi.org/10.1007/s00198-018-4503-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4503-z