Abstract
Summary
Although fractures are associated with short-term reductions in functional status, there is limited information on longer-term burden of fracture. This study documents evidence of an association between fractures and significant declines and functional health and activities that persist but attenuate beyond two years.
Introduction
Although fractures are associated with short-term reductions in functional status and may have other short-term effects on healthcare utilization (hospitalization and follow-up care), there is limited information on long-term burden of fracture beyond 12 to 24 months post-fracture. Analysis of the long-term health burden can inform policymakers, health care practitioners, and payers.
Methods
We acquired a data set containing the 1992–2012 Health and Retirement Survey data linked to the same individuals’ Medicare claims. Fracture cases (n = 745) were matched to non-fracture controls using propensity scores matching. A regression-adjusted difference-in-difference (DD) approach was used to compare the change in functional status measures from baseline to two post-fracture periods for fracture cases relative to the change over the same time periods for matched controls. Self-reported measures of functional status were examined: limitations to activities of daily living (ADLs), limitations to instrumental activities of daily living (IADLs), a mobility index, a gross motor skills index, a fine motor skills index, and self-reported general health status.
Results
Fracture cases reported increases in limitations to ADLs, difficulties with mobility, difficulties with gross motor skills, and difficulties with fine motor skills in each HRS collection period (the survey is administered every 2 years) following the fracture or index date (thus up to two years later) than matched controls (all p values < 0.05). The magnitude of these effects diminished in the second post-fracture wave (two to four years after fracture/index date), but they were still statistically significant.
Conclusions
Results suggest that fractures are associated with significant declines in some measures of functional activities up to two years following the fracture. The effects persist beyond two years but are smaller in magnitude.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the United States, more than 53 million people have osteoporosis or are at risk for developing the disease due to low bone mass [1]. Osteoporosis increases the risk for bone fracture; depending on age and bone density, a 10-year fracture risk can more than double [2, 3]. Osteoporotic fractures are quite frequent; one study estimated that there are more than 2 million osteoporosis-related fractures annually in the USA resulting in almost $17 billion in healthcare spending in 2005 [4]. In a recent study of women over 55, there was an age-adjusted rate of 1124 admissions per 100,000 person-years, compared to myocardial infarction (MI) (668), stroke (687), and breast cancer (151). Costs for these events are also much higher than for other diseases in this age group: annual facility-related hospital costs for osteoporotic fracture were $5.1 billion, higher than stroke ($3.3 billion), MI ($4.3 billion), or breast cancer ($0.5 billion) [5]. The numbers of fractures and associated expenditures are projected to increase due to an aging population and increasing health care costs [4].
In addition to financial costs and specific health outcomes, osteoporosis-related fracture is associated with changes in functional status and quality of life. Functional loss post-fracture has been found to be high; one review focusing on fractures of the hip found that survivors of hip fractures had worse mobility, less functional independence, higher rates of hospitalization, and lower quality of life following the fracture, with the bulk of recovery of walking and activities of daily life occurring within the 6 months following the fracture [6]. Another study found that a large percentage (between 20 and 65%) of individuals who had been independent before their fracture needed assistance with various self-care activities one to 2 years after a hip fracture, while 53% required assistance to get to places out of walking distance [7]. In additional to functional status decreases, mortality also increases after hip fracture [8] Most of the prior research examining functional health has been shorter term, with outcomes measures examined only up to 2 years after the fracture [9,10,11]. In addition, these studies are often more than a decade old, consider a limited range of outcomes, and tend to be based on smaller sample sizes [8, 12]. Less is known about the longer-term effects of fracture on functional status.
Using a dataset combining longitudinal Medicare claim data with self-reported survey data related to labor, wellbeing, and functional status, we aimed to provide an updated, comprehensive assessment of the impacts of osteoporotic fractures on non-economic burden measures with a particular focus on how the associations between fracture and outcomes change over time. Based on the impact of many fractures on the ability to ambulate and otherwise self-care, we hypothesized that Medicare beneficiaries with an osteoporosis-related fracture would have worse overall health and functional status after the fracture event and for a sustained duration (up to 4 years after fracture) than matched comparisons.
Methods
Data source and sample
We used data from the Health and Retirement Study (HRS) linked to Medicare claims. The HRS, sponsored by the National Institutes of Aging (NIA) and the Social Security Administration and fielded by the Institute for Social Research at the University of Michigan, is a biennial panel survey, which collects health, demographic, psychosocial, and economic measures from a nationally representative sample of the US population of individuals age 50 and over. Approximately 80% of respondents who are eligible for Medicare have agreed to have their HRS data linked to their Medicare professional and facility claims [13].
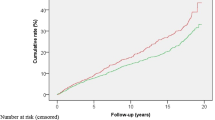
We used the HRS-Medicare linked sample provided by MedRIC (Acumen) with the following restrictions (see Appendix Fig. 1). Individuals must be at least 65 years of age in the pre-period and continuously enrolled in traditional Medicare (i.e., we excluded those covered by Medicare managed care). We used the 1992 to 2012 waves of the data (collected every 2 years), but required that each respondent with a fracture have at least one wave of data prior to the index date (date of the fracture) and another wave after the fracture. We identified osteoporosis-related fracture cases as those with at least one fracture ICD-9 diagnosis during an inpatient stay or at least one fracture ICD-9 diagnosis on a professional claim with at least one fracture repair procedure (see Appendix Table 3) within 90 days of the initial professional claim with a fracture diagnosis. Among fracture cases, were excluded respondents with a cancer diagnosis (ICD-9 codes 140–172, 174–208, or 213) within 6 months before or after fracture diagnosis; respondents with a fracture diagnosis within the first 6 months of Medicare enrollment or within the last 6 months of 2012, and respondents with major trauma E-codes (E800-E848, E881-E884, E908-E909, or E916-E928) concurrent with the index fracture event. Our final analytic sample contained 745 fracture cases, whom we followed across three waves: the pre-fracture wave (baseline), the wave during which the fracture occurred according to Medicare claims (post-period 1),Footnote 1 and one additional follow-up wave (post-period 2). To create the control group, we matched fracture cases to comparison respondents (n = 745) using baseline data (as described below) and then included three additional waves of data (from the index period, based on an index date; follow-up period 1, relative to the index period; and follow-up period 2) for comparison. We refer to these time frames for both fracture cases and comparison respondents as the index period (in which a fracture does or does not occur); post-period 1 (0–2 years after the index period), and post-period 2 (2–4 years after the index period).
Measures
Primary outcomes
We examined a number of self-reported measures of health status and functioning. General health status was measured on a 5-point scale ranging from 1 (excellent) to 5 (poor) based on respondents’ answers to “Would you say your health is excellent, very good, good, fair, or poor?” There is a large body of literature on measuring physical function [14], but here we focus on the key measures consistently available in the HRS that track mobility, large muscle functioning, fine and gross motor skills, limitations in activities “which people perform habitually and universally,” [15] and functioning that reflects “instrumental self-care” [16]. The number of ADLs was summed based on whether a respondent reported difficulty bathing, dressing, eating, getting in/out of bed, and walking across a room. Similarly, respondents’ IADLs were summed based on whether they reported difficulty with using the phone, managing money, and taking medications. We examined three measures of mobility/movement: (1) a mobility index measured as a count of the respondent’s difficulty with the following: walking one block, walking several blocks, walking across a room, climbing one flight of stairs, and climbing several flights of stairs;Footnote 2 (2) a gross motor skills index measured as a count of the respondent’s difficulty with the following: walking one block, walking across a room, climbing one flight of stairs, getting in or out of bed, and bathing;Footnote 3 (3) a fine motor skills index measured as a count of the respondent’s difficulty with the following: picking up a dime, eating, and dressing activities [17].Footnote 4
Covariates
We used the following measures in our analyses as described below: age (continuous), gender (indicator), race/ethnicity (categorical), whether a proxy answered the HRS questionnaire (indicator), respondent’s body mass index (BMI), whether the respondent is a current smoker (indicator), whether the respondent drinks three or more alcoholic drinks per day (indicator), whether the respondent reported vigorous activity three or more times per week (indicator), and total baseline medical costs (based on claims). The proxy status measure is correlated with the respondent’s cognitive function and ability to answer questions and is therefore, an important matching characteristic [18].
Statistical analyses
We used propensity score matching to create an analytic sample of fracture cases matched to comparisons that were statistically similar in the pre-fracture or index period. We estimated a logistic regression where “had fracture” was a function of the following baseline measures: respondent’s gender, age, race/ethnicity, proxy status, body mass index (BMI), and total medical costs as reported in the HRS in the wave prior to the fracture. We calculated the predicted probability of a fracture event using the estimated coefficients from this regression and selected comparison cases with the nearest propensity score without replacement (i.e., comparisons could not serve as comparisons for more than one fracture case) for each fracture case. We excluded cases outside of the common support.Footnote 5 The propensity score matching was performed using SAS 9.3 [19].
Using the matched sample, we estimated regression-adjusted difference-in-differences (DD) models, which allowed us to compare changes in functional health for fracture cases over time relative to statistically similar comparisons. The DD allows us to isolate changes in functional status that are related to the fracture from other secular trends in functional health (e.g., functional health tends to decline in general as a result of aging), but relies on the assumption that trends in the pre-period were similar among fracture and comparison cases. Although we cannot examine trends beyond one pre-period, the propensity score matched comparisons will be similar to fracture cases in the pre-period by construction. We used regression adjustment for the DD analysis in order to obtain doubly robust estimates [20] and to better adjust for baseline costs. Although we used baseline costs in the propensity score matching, they were based on self-reported costs as reported in the HRS in the wave prior to the fracture and thus covered a two-year pre-period. We had to use HRS costs for this purpose because comparison cases would not have had a fracture or index date yet to use for matching. After comparison cases were matched to fracture cases, they were assigned the fracture/index date of their matched case. Then, we were able to create a claims-based measure of costs in the year prior to the fracture/index date, excluding the week prior to that date. In the DD analysis, we included this measure—costs in the year prior to the fracture/index date—as a control variable. We also included age, race, gender, and proxy status using a Poisson regression. DD regressions were estimated using Stata 13 [21]. We used HRS respondent-level sampling weights in all estimations.
Results
Table 1 presents descriptive statistics of the sample population. Even after matching on costs prior to the fracture date, fracture cases tend to report greater out-of-pocket health care costs, but these cases tend to be similar on other observable demographic characteristics. Fracture and comparison cases reported similar functional limitations at baseline, but fracture cases reported slightly worse self-reported general health status at baseline.
Adjusted means and DD estimates for fracture and comparison cases across three HRS periods are provided in Table 2. Overall, fracture cases reported more functional health limitations in both post-periods relative to their counterparts without fracture. The increases in limitations over time were also greater for fracture cases with the DDs from baseline to follow-up period 1 all statistically significant at p < 0.05.
The number of ADL limitations increased from 0.49 to 0.90 (84%) for fracture cases from baseline to the first follow-up period relative to an increase from 0.39 to 0.47 (21%) for matched comparisons. Thus, fracture cases had a 0.33 greater increase in the number of reported limitations with ADLs than matched comparisons experienced, which was about a 63 percentage point difference (84% increase vs. 21% increase). Similarly, fracture cases reported a 0.44 greater increase (31 percentage point increase) in difficulties with mobility, 0.43 greater increase (57 percentage point increase) in difficulties with gross motor skills, 0.11 greater increase (33 percentage point increase) in difficulties with fine motor skills, and 0.10 greater increase (36 percentage point increase) in limitations to IADLs than matched comparisons (all p values < 0.01 except for fine motor skills and count of IADLs, which had p value < 0.05).
The magnitude of these effects diminishes in the second follow-up fracture wave (2 to 4 years after fracture/index date) to 0.19 greater increase (27 percentage point increase, compared to the index period) in limitations to ADLs, 0.41 greater increase (27 percentage point increase) in mobility limitations, 0.32 greater increase (42 percentage point increase) in limitations to gross motor skills (all p values < 0.01), and 0.11 (34 percentage point increase) greater increase in limitations to fine motor skills 2 to 4 years after the fracture relative to matched comparisons (p value < 0.05). The difference in the count of IADLS was no longer statistically significant in the second follow-up wave.
Thus the effects seen after a fracture mostly persisted, though attenuated, with the exception of changes in IADLs, which ceased to be significantly different by the second follow-up period. There was no significant difference in the change in self-reported health status across fracture and comparison cases over time at either follow-up period.
Discussion
Prior research has established the heavy burden of fracture on functional status, particularly for those in long-term care facilities [22,23,24]. However, prior work has typically focused on the first few months after a fracture, does not look at general health, does not have a comparison group which is necessary to remove any aging-related decline in functional status, or has not been updated recently [22, 23, 25, 26].
The HRS-Medicare linked data offer a unique insight into the longer-term impact of fractures on richer measures of physical health. These data allowed us to test whether there are longer-term implications regarding physical functioning for older individuals post-fracture.
Comparing changes in functional status of individuals with an osteoporosis-related fracture to individuals with statistically similar health histories and profiles suggests that the former group experienced greater reductions in functional health relative to their comparisons. This difference persisted over time.
The increase in IADLs at follow-up period 1 becomes statistically insignificant in the second follow-up period but all other comparisons continue to be significant into the 2–4-year time frame. These findings support the hypothesis that fractures impose a burden on older individuals (at least for some measures of functional status) that lasts longer than is typically studied in the literature.
Although the magnitude of the associations between fracture and fine motor skills and IADLs were relatively small at follow-up period 1 and 2, and no longer significant for IADLs at follow-up period 2, these measures encompass movement that is less likely to be affected, especially in the longer term, by a fracture. For example, activities that typically do not require large muscle strength, such as managing money, taking medications, eating, picking up a dime, or using the phone, are less likely be impeded by a broken femur or hip. We also found no evidence of a differential effect of a fracture on self-reported general health. As people switch insurance frequently, insurance companies may focus on shorter-term costs and impact with less focus on longer-term outcomes. Medicare may be less likely to focus on the short-term as its population stays enrolled longer, but may still be influenced by shorter-term measures and costs. We encourage both researchers and insurers to consider the longer-term impact of major health events; even as the impact attenuates, the difference between fracture cases and controls remains after 2 to 4 years. Further research should explore beyond the first year post-fracture, which is the most studied. Only with more information on the longer-term impact of fractures will decision-makers (including payers and policymakers focusing on public health like CDC) be able to best prioritize investments in technologies, treatments, and other interventions to reduce the likelihood of fractures.
Limitations
Although we employed a rigorous empirical approach that is standard in the evaluation literature—DD estimation [27]—it relies on the assumption that the health trajectories of fracture and comparison cases were similar prior to the fracture. We endeavored to ensure this by using the propensity score matching approach matching fracture cases to comparison cases with similar gender, age, race/ethnicity, baseline proxy status, baseline BMI, and baseline total medical costs,Footnote 6 but note that we are only matching using one pre-period. Our approach also addresses issues of selection, whereby we might be concerned that individuals who have fractures are systematically different in both observable (e.g., frailer or sicker as indicated in the HRS and Medicare data) and unobservable ways (e.g., genetic predisposition). Because we are comparing the change in both fracture and comparison cases, any comorbidities or individual characteristics that are time-invariant are effectively removed in the DD model.Footnote 7
Additionally, as noted above, approximately 20% of HRS respondents who are eligible for Medicare opted not to have their claims linked to the HRS. Our findings may not be representative or generalizable if those who did not consent were systematically different from those who did consent (e.g., those who are sicker). Standard concerns of measurement error from self-reported data could result in attenuation bias, which is exacerbated in models with differencing.
Conclusion
The shorter-term impact of fractures has been well described, but until now, researchers have not measured the longer-term implications. Our study is one of the first to explore this issue, identifying a significant impact of these events on functional health. Future studies similarly explore the longer-term impact of fractures on cost and overall health status.
Notes
We include only cases where the Medicare fracture date of service was prior to the HRS interview date.
See http://hrsonline.isr.umich.edu/sitedocs/userg/dr-008.pdf for a detailed list of the questions used from year to year. Generally, the questions are framed as “Because of a health problem, do you have any difficulty…” The specific difficulties for questions used in the mobility index are: (1) “with walking one block,” (2) “with walking several blocks,” (3) “with walking across a room,” (4) “climbing one flight of stairs without resting,” and (5) “climbing several flights of stairs without resting.”
See http://hrsonline.isr.umich.edu/sitedocs/userg/dr-008.pdf for a detailed list of the questions used from year to year. Generally, the questions are framed as “Because of a health problem, do you have any difficulty…” The specific difficulties for questions used in the gross motor skills index are: (1) “with walking one block,” (2) “with walking across a room,” (3) “climbing one flight of stairs without resting,” (4) “getting in or out of bed,” and (5) “bathing or showering.”
See http://hrsonline.isr.umich.edu/sitedocs/userg/dr-008.pdf for a detailed list of the questions used from year to year. Generally, the questions are framed as “Because of a health problem, do you have any difficulty…” The specific difficulties for questions used in the fine motor skills index are: (1) “with picking up a dime from a table,” (2) “with eating, such as cutting up your food,” and (3) “with dressing, including putting on shoes and socks.”
For the 1996 match, we dropped 127 comparison cases that were not within the common support (out of 3737 possible comparison cases). All 91 fracture cases in 1996 were within the common support. For the 1998 match, we dropped 263 comparison cases that were not within the common support (out of 3237 possible comparison cases). We dropped one fracture case in 1998 that was not within the common support (out of 114 fracture cases). For the 2000 match, we dropped 415 comparison cases that were not within the common support (out of 4454 possible comparison cases). All 85 fracture cases in 2000 were within the common support. For the 2002 match, we dropped 305 comparison cases that were not within the common support (out of 4654 possible comparison cases). All 100 fracture cases in 2002 were within the common support. For the 2004 match, we dropped 158 comparison cases that were not within the common support (out of 4568 possible comparison cases). All 82 fracture cases in 2004 were within the common support. For the 2006 match, we dropped 434 comparison cases that were not within the common support (out of 4229 possible comparison cases). All 91 fracture cases in 2006 were within the common support. For the 2008 match, we dropped 363 comparison cases that were not within the common support (out of 4032 possible comparison cases). All 88 fracture cases in 2008 were within the common support. For the 2010 match, we dropped 339 comparison cases that were not within the common support (out of 3910 possible comparison cases). All 97 fracture cases in 2010 were within the common support.
We explored using additional baseline covariates for propensity score matching, including whether individuals smoked (ever smoked), drank alcoholic beverages (measured as counts or whether respondent had 3+ per day), and engaged in 3+ hours of vigorous physical activities per week. These covariates were all statistically insignificant in predicting a fracture and did not affect the matching. Therefore, we chose the more parsimonious model with fewer covariates.
Here is a simplified version of the regression-adjusted DD model:
$$ {Y}_{i t}={\beta}_0+{\beta}_1{{\mathrm{Post}}_t}^{\ast }{\mathrm{Fracture}}_i+{\beta}_2{\mathrm{Post}}_t+{\beta}_3{\mathrm{Fracture}}_i+{\beta}_{4\ }{X}_i+{\varepsilon}_{i t} $$where \( \hat{\beta_1} \) is our estimated difference-in-difference; post = 1 in the period after the fracture and 0 in the pre-period; fracture = 1 for fracture cases and 0 for comparison cases; X is a vector of individual level (time-invariant controls). It does not matter which time-invariant covariates are included in X (or not included), because they are differenced out. To see this, consider what \( \hat{Y_{\mathrm{i}}} \) is for both fracture and comparison cases in the pre- and post-periods; then examine the first differences (last column) where we look at the change in Y for each group.
Pre (post = 0) (column 1)
Post (post = 1) (column 2)
First difference (column 2–column 1)
Fracture (fracture = 1)
β 0 + β 3 + β 4 X i + ε it
β 0 + β 1 + β 2 + β 3 + β 4 X i + ε it
β 1 + β 2
Comparison (fracture = 0)
β 0 + β 4 X i + ε it
β 0 + β 2 + β 4 X i + ε it
β 2
Difference-in-difference
β 1
References
NIH Osteoporosis and Related Bone Diseases NRC (2015) Osteoporosis overview. http://www.niams.nih.gov/Health_Info/Bone/Osteoporosis/overview.pdf
Kanis JA, Oden A, Johansson H, Borgstrom F, Strom O, McCloskey E (2009) FRAX and its applications to clinical practice. Bone 44(5):734–743
Siminoski K, Leslie WD, Frame H et al (2007) Recommendations for bone mineral density reporting in Canada: a shift to absolute fracture risk assessment. J Clin Densitom 10(2):120–123
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 22(3):465–475
Singer A, Exuzides A, Spangler L et al (2015) Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc 90(1):53–62
Dyer SM, Crotty M, Fairhall N et al (2016) A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 16:158
Magaziner J, Hawkes W, Hebel JR et al (2000) Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci 55(9):M498–M507
Bentler SE, Liu L, Obrizan M et al (2009) The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol 170(10):1290–1299
Pasco JA, Sanders KM, Hoekstra FM, Henry MJ, Nicholson GC, Kotowicz MA (2005) The human cost of fracture. Osteoporos Int 16(12):2046–2052
Brenneman SK, Barrett-Connor E, Sajjan S, Markson LE, Siris ES (2006) Impact of recent fracture on health-related quality of life in postmenopausal women. J Bone Miner Res 21(6):809–816
Fukui N, Watanabe Y, Nakano T, Sawaguchi T, Matsushita T (2012) Predictors for ambulatory ability and the change in ADL after hip fracture in patients with different levels of mobility before injury: a 1-year prospective cohort study. J Orthop Trauma 26(3):163–171
Hallberg I, Bachrach-Lindstrom M, Hammerby S, Toss G, Ek AC (2009) Health-related quality of life after vertebral or hip fracture: a seven-year follow-up study. BMC Musculoskelet Disord 10:135
University of Michigan (2016) HRS/CMS research data. http://hrsonline.isr.umich.edu/index.php?p=medicare. Accessed Sept 2016
Nagi SZ (1976) An epidemiology of disability among adults in the United States. The Milbank Memorial Fund Quarterly Health and Society:439–467
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW (1963) Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA 185(12):914–919
Lawton M, Brody EM (1970) Assessment of older people: self-maintaining and instrumental activities of daily living. Nurs Res 19(3):278
Fonda S, Herzog AR (2004) HRS/AHEAD documentation report: documentation of physical functioning measured in the Heath and Retirement Study and the Asset and Health Dynamics among the Oldest Old Study. http://hrsonline.isr.umich.edu/sitedocs/userg/dr-008.pdf
Weir D, Faul J, Langa K (2011) Proxy interviews and bias in the distribution of cognitive abilities due to non-response in longitudinal studies: a comparison of HRS and ELSA. Longit Life Course Stud 2(2):170–184
SAS Institute Inc. (2011) SAS® 9.3 system options: reference. SAS Institute Inc, Cary
Funk MJ, Westreich D, Wiesen C, Stürmer T, Brookhart MA, Davidian M (2011) Doubly robust estimation of causal effects. Am J Epidemiol 173(7):761–767
StataCorp L. (2014) Stata 13. College Station: StataCorp LP
Ekström W, Németh G, Samnegård E, Dalen N, Tidermark J (2009) Quality of life after a subtrochanteric fracture: a prospective cohort study on 87 elderly patients. Injury 40(4):371–376
Beaupre LA, Cinats JG, Jones CA et al (2007) Does functional recovery in elderly hip fracture patients differ between patients admitted from long-term care and the community? J Gerontol Ser A Biol Med Sci 62(10):1127–1133
Lin PC, Chang SY (2004) Functional recovery among elderly people one year after hip fracture surgery. J Nurs Res 12(1):72–82
Visser M, Harris TB, Fox KM et al (2000) Change in muscle mass and muscle strength after a hip fracture relationship to mobility recovery. J Gerontol Ser A Biol Med Sci 55(8):M434–M440
Tang VL, Sudore R, Cenzer IS et al (2016) Rates of recovery to pre-fracture function in older persons with hip fracture: an observational study. J Gen Intern Med
Imbens GW, Wooldridge JM (2009) Recent developments in the econometrics of program evaluation. J Econ Lit 47(1):5–86
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Kandice Kapinos, Shira Fischer, Andrew Mulcahy, and Orla Hayden are employees of the RAND Corporation, which received an unrestricted grant from Amgen for this research. Lionel Pinto and Rich Barron are employees of Amgen.
Sponsor’s role
This project was supported by Amgen Inc. under a contract that provided for independent analysis by the authors. The role of the sponsor in each phase of the research was as follows. Design and conduct of the study: the sponsor requested a proposal for analysis from the authors. The authors and the sponsor designed and proposed the study, which the sponsor accepted. The authors conducted the study. Collection, management, analysis, and interpretation of the data: the authors obtained access to the restricted data used in this study and managed, analyzed, and interpreted the data. The sponsor reviewed the output and provided feedback on results and modeling. Preparation, review, or approval of the manuscript: the authors prepared the manuscript. The manuscript was reviewed by the sponsor for comment, which the authors considered in further revisions. By contract, the authors had the authority to independently revise and submit the manuscript.
Rights and permissions
About this article
Cite this article
Fischer, S., Kapinos, K.A., Mulcahy, A. et al. Estimating the long-term functional burden of osteoporosis-related fractures. Osteoporos Int 28, 2843–2851 (2017). https://doi.org/10.1007/s00198-017-4110-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4110-4