Abstract
Summary
In women with osteoporosis treated with alendronate for >12 months and oral bisphosphonates for >3 of the last 4 years, switching to MK-5442, a calcium receptor antagonist, stimulated endogenous parathyroid hormone (PTH) secretion and increased bone turnover marker levels, but produced a decline in bone mineral density (BMD) at all sites.
Introduction
This study assessed the effects of switching from long-term oral bisphosphonate therapy to the calcium-sensing receptor antagonist MK-5442 on BMD and bone turnover markers (BTMs) in post-menopausal women with osteoporosis.
Methods
This randomized, active and placebo-controlled, dose-ranging study enrolled 526 postmenopausal women, who had taken alendronate (ALN) for ≥12 months preceding the trial and any oral bisphosphonate for ≥3 of the preceding 4 years and had spine or hip BMD T-scores ≤−2.5 or ≤−1.5 with ≥1 prior fragility fracture. Women were randomized to continue ALN 70 mg weekly or switch to MK-5442 (5, 7.5, 10, or 15 mg daily) or placebo.
Results
Switching from ALN to MK-5442 produced a dose-dependent parathyroid hormone (PTH) pulse of threefold to sixfold above baseline at 1 h, with PTH levels that remained twofold to threefold above baseline at 4 h and returned to baseline by 24 h. Switching to MK-5442 or placebo increased BTM levels compared to baseline within 3 months and MK-5442 10 mg increased BTM levels compared to placebo by 6 months. With all MK-5442 doses and placebo, spine and hip BMD declined from baseline, and at 12 months, BMD levels were below those who continued ALN (all groups P < 0.05 vs ALN). There was also a dose-dependent increase in the incidence of hypercalcemia with MK-5442.
Conclusion
Switching from ALN to MK-5442 resulted in a pulsatile increase in PTH and increases in BTMs, but a decline in BMD compared with continued ALN. MK-5442 is not a viable option for the treatment of osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alendronate (ALN) has been shown to improve spine and hip bone mineral density (BMD) and reduce fracture risk throughout the skeleton over 3–4 years [1, 2]. Studies that evaluated the efficacy of treatment beyond this time period showed that BMD levels in the hip region generally plateau after 4 years [2, 3], as a result of achievement of a new steady state, with a very low rate of remodeling and a very small remodeling space deficit. Due to the limited evidence of efficacy beyond 5 years, patients who remain at high risk of fracture after a 5-year treatment with oral ALN might benefit from a change in therapy.
Although there are no clinical trials that assess fracture risk in patients who switch from ALN to other therapies, several BMD endpoint studies have been performed. Many of the patients in these trials had only been treated with ALN for a short duration. In women with low BMD after treatment with ALN for at least 1 year, there were no BMD increases in those randomized to zoledronic acid vs. those randomized to remain on ALN [4]. In a similar study of previously treated women switched to denosumab, BMD increases at all skeletal sites were greater in the group that switched to denosumab compared with the group that continued ALN, although in this trial, women were enrolled after ALN treatment periods as short as 6 months [5].
In women on established ALN, the effects of suppressing bone remodeling have plateaued, remodeling cavities have been filled in, the number of stress risers has been minimized, and bone mineralization density has improved [6–8]. At this stage, in order to attain a greater reduction in incidence of fracture, an agent that can stimulate bone formation, increase bone mass, improve bone architecture, and produce newer and perhaps stronger bone might be more fruitful than switching to another antiresorptive agent. To this end, it should be noted that there have been no clinical trials which evaluate the skeletal effects of continuing a bisphosphonate compared with switching to an anabolic agent on bone density, strength, or fracture risk. Several trials have investigated the effects of switching from ALN to teriparatide or PTH1-84 [9–13]. These studies demonstrated that women who switched from ALN to teriparatide or PTH had an increase in spine BMD; however, hip BMD declined consistently during the first year [14]. Furthermore, many patients will not accept a therapy requiring daily injections, and others have concerns about drug safety [15, 16]. Therefore, other therapeutic options for these patients need to be explored.
MK-5442 is an orally active allosteric inhibitor of the calcium-sensing receptor (also called a “calcilytic”) that has been shown to stimulate endogenous PTH secretion in short-term clinical studies. PTH is anabolic to bone when delivered as a brief pulse but is catabolic when administered continuously [17]. An experimental transdermal method of teriparatide administration produced a similar peak PTH concentration, with an even briefer duration compared to the marketed subcutaneous teriparatide formulation. Over 6 months, this transdermal formulation produced a greater hip BMD increase than subcutaneous teriparatide [18]. In contrast, the calcilytic compound ronacaleret produced a prolonged elevation of serum PTH for more than 4 h and did not increase BMD [19].
The current study was designed to determine if administration of MK-5442 to women on prior bisphosphonate treatment could induce a PTH pulse, stimulate bone turnover marker (BTM) increments, and improve BMD compared to continuation of ALN.
Methods
Study design
This was a 1-year, randomized, double-blind, placebo- and active-controlled, dose-ranging trial of the orally administered calcium-sensing receptor antagonist MK-5442 (Fig. 1a). The treatment duration for this study was initially planned for 2 years; however, the study protocol was amended following the availability of data from a parallel study of treatment-naïve women conducted in Japan, which indicated that the effect of MK-5442 on BMD accrual in treatment-naïve patients was marginal [20]. This study was conducted in accordance with the principles of good clinical practice and approved by the appropriate institutional review boards and regulatory agencies. Details of the full protocol can be accessed via the attached file (ESM).
Participants
Women enrolled in this study were 45–85 years old and postmenopausal for ≥5 years. They had taken any oral bisphosphonate for treatment of osteoporosis for at least 3 of the 4 years prior to screening and had to be actively taking ALN for the 12 months preceding the trial, with at least 80 % self-reported adherence. Participants were required to have BMD T-scores ≤−2.5 at one or more sites (lumbar spine, femoral neck, trochanter, or total hip) or T-scores ≤−1.5 with at least one prior osteoporosis-related fracture (no major trauma such as a motor vehicle accident, fractures other than digits and skull). We required at least one hip and at least three of four lumbar spine vertebrae (L1–4) to be evaluable by dual-energy X-ray absorptiometry (DXA). Also required were serum 25 hydroxyvitamin D (25(OH)D) levels ≥15 ng/mL, or ≥9 and <15 ng/mL if alkaline phosphatase and intact PTH levels (as measured by the central laboratory) were normal (9.0–39.0 pg/mL).
Exclusion criteria included BMD T-scores at any of the four sites below −4.0 and use at any time in the past of the following medications: IV bisphosphonates, fluoride >1 mg/day for >2 weeks, strontium, growth hormone, cathepsin K inhibitor, or denosumab. Users of bisphosphonates other than ALN within the past 12 months were excluded, as were users of PTH (1–34 or 1–84) within 24 months, and users of cyclosporine, anabolic steroids, or glucocorticoids for more than 2 weeks in the past 6 months. Users of soy isoflavones, pioglitazone, rosiglitazone, estrogen ± progesterone, or a selective estrogen receptor modulator within 6 months, or heparin, or potent inhibitors or inducers of CYP3A4 (e.g., rifampin or phenytoin) within 2 weeks were excluded. Women with primary parathyroid disease, prior total thyroidectomy, Paget’s disease, HIV infection, malignancy within 5 years, or other major illnesses were also excluded. All participants provided written informed consent to participate in the study.
Treatment
Women were randomized using an interactive voice response system (IVRS), based on a computer-generated algorithm provided by the sponsor, to ALN 70 mg weekly with placebo matching the MK-5442 formulation daily; MK-5442 5, 7.5, 10, or 15 mg daily with placebo matching ALN weekly; or matching placebos for both study drugs. All participants received oral vitamin D3 (2x2800 IU tablets weekly) and supplemental calcium if daily intake at screening was <1200 mg/day. Women were told not to ingest potent inhibitors (e.g., ketoconazole, clarithromycin) or inducers (e.g., dexamethasone, rifampin) of CYP3A4 during the study.
Assessments
Bone mineral density
Areal BMD was measured by DXA using Hologic or GE Lunar densitometers, at the spine, total hip, femoral neck, total body, and one third distal forearm. DXA measurements were performed at the left hip (unless it was not evaluable) at screening or baseline and months 3, 6, and 12. Quality control was performed, and BMD readings were evaluated centrally (Perceptive, Billerica, MA).
Biochemical assessments
Blood and urine samples were collected at screening, baseline, and months 1, 3, 6, and 12 in the morning after at least 8 h of fasting overnight except for water and concomitant medications. Urine was collected as a second morning void specimen. At baseline, serum levels of 25(OH)D and “intact PTH” (containing at least residues 7–84) were measured. For pharmacodynamic analysis, serum “whole PTH” (residues 1–84) levels were assayed. For the latter, serum PTH samples were collected prior to dosing of study medication and at 1, 4, and 24 h after dosing. Total serum calcium was also measured at these time points. Assays for serum 25(OH)D and intact PTH (using Diasorin Liaison chemiluminescence) and serum calcium were performed by PPD (Zaventem, Belgium and Highland Heights, KY). Whole PTH (1–84) levels were assayed by Pacific Biomarkers (Seattle, WA) using an immunoradiometric assay with an inter-assay coefficient of variation <8 %. Biochemical markers of bone formation, serum N-terminal pro-peptide of type I collagen (sPINP) and serum bone-specific alkaline phosphatase (sBSAP), and of bone resorption, urinary N-terminal cross-linked telopeptides of type I collagen/creatinine (uNTx/Cr) and serum C-terminal cross-linked telopeptides of type I collagen (sCTx), were also measured centrally at PPD (Zaventem, Belgium, and Highland Heights, KY) with quality controls stipulating that repeated measurements of standards have a coefficient of variation ≤10 %.
Safety
Safety was assessed by evaluation of adverse experiences (AEs), vital signs, excessive bone loss, and laboratory assessments. Laboratory assessments, including serum calcium and phosphate, were measured at screening, randomization, and months 1, 3, 6, 9, and 12. At any post-randomization visit, patients were discontinued for excessive bone loss (loss of BMD at the spine or total hip of ≥6 % up to 6 months and ≥8 % up to 12 months compared with baseline) or persistent hypercalcemia, defined as a repeat serum calcium concentration greater than the upper limit of normal (normal range 8.5–10.5 mg/dL) within 2 weeks of an initial elevated serum calcium level.
Statistical methods
The primary endpoint of the study was the 12-month percentage change from baseline at the lumbar spine BMD in women switched from ALN to MK-5442, compared to those on continued ALN treatment. BMD was analyzed on the full analysis set population defined as all women who received at least one dose of drug treatment and had a baseline and at least one on-treatment measurement. A longitudinal data analysis model [21] assessed treatment effects, adjusting for treatment, time, interaction of time by treatment, baseline measurements, and region.
BTM endpoints were assessed as percentage change from baseline and were analyzed in the per-protocol population, defined as the population excluding patients with important deviations from the protocol that may have substantially affected the results of the primary efficacy endpoint. Analyses used a constrained longitudinal analysis model, adjusting for treatment, time, and interaction of time by treatment, baseline measurements, and region. Comparison of geometric means by log scale was back transformed for presentation. For multiplicity, comparisons of multiple doses of MK-5442 versus ALN and placebo in BMD and BTM were adjusted using the two-sided step-down Dunnett’s test. Safety results are presented descriptively, including all-patients-as-treated.
Results
A total of 526 postmenopausal women taking ALN 70 mg weekly, with a median of 5.2 years of oral bisphosphonate use, were randomized to treatment (Fig. 1a). The treatment group receiving the highest (15 mg daily) dose of MK-5442 was discontinued from the study by the sponsor after 5–12 months of treatment, due to the high incidence of hypercalcemia (33 %, range 32–44 %) observed with that dose in this and another parallel study [20, 22]. Of the women in the remaining treatment groups, 75 % completed the trial (Fig. 1b). All treatment groups had similar baseline characteristics (Table 1), with overall mean age 67.5 and mean spine BMD T-score −2.5. Similarly, there were no group differences for mean baseline levels of PTH, 25(OH)D, or biochemical indices of bone turnover.
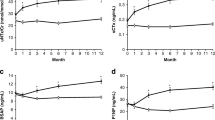
Mean BMD declined in spine, total hip, and femoral neck similarly in the MK-5442 and placebo groups, with no significant group differences, whereas BMD increased or remained stable at all sites in the continued ALN group (Fig. 2a). At 12 months, mean BMD levels for all sites in all MK-5442 groups as well as the placebo group were all significantly lower than mean BMD levels in the continued ALN group.
a BMD endpoints. Graphic representation of the LS mean percentage change from baseline (95 % CI) over 12 months in BMD at the specified site after administration of either MK-5442 (5, 7.5, and 10 mg), alendronate (70 mg), or placebo at lumbar spine, total hip, and femoral neck. b Bone turnover marker endpoints. Graphic representation of the mean absolute concentrations of the BTMs at baseline and 12 months after administration of either MK-5442 (5, 7.5, and 10 mg), alendronate (70 mg), or placebo for PINP (ng/mL), BSAP (ng/mL), sCTx (pg/mL), and uNTx/Cr (nmol/mmol)
BTMs increased significantly after switching to MK-5442 or placebo (Fig. 2b and Table 2). All BTMs rose significantly from baseline levels by 3 months at all MK-5442 doses as well as with placebo, and they continued to increase from 3 through 12 months. Percent increases for all doses of MK-5442 differed significantly from those of ALN at all time points (3, 6, and 12 months) for each of the BTMs (P < 0.001). At 3 months, response to MK-5442 differed significantly from placebo only for sPINP with MK-5442 10 mg. At 6 and 12 months, increases with MK-5442 at all doses were higher than with placebo for sPINP, sBSAP, and sCTx (P < 0.05). The smallest difference between MK-5442 and placebo was seen for uNTx/Cr, where only the highest dose of MK-5442 (10 mg) at 6 and 12 months resulted in a significant difference from placebo.
Increases in serum PTH of approximately threefold to sixfold (70–170 pg/mL) were seen an hour after MK-5442 administration at months 1, 6, and 12, with a dose–response effect (Fig. 3). Within 4 h after MK-5442 administration, PTH concentrations were reduced from the peak by approximately one third, and by 24 h, PTH levels returned to the baseline predose value. PTH increments and profiles were similar after 1, 6, and 12 months of treatment. No changes in PTH levels were seen in patients who remained on ALN or in those who switched to placebo.
There were no differences between treatment groups in overall AEs, serious AEs, or discontinuations due to serious AEs (Table 3). One patient in the MK-5442 15-mg group died on study day 67 due to hypertensive heart disease, unlikely to be related to MK-5442 treatment. Hypercalcemia was the only AE that showed treatment-related increases with MK-5442. The overall incidence of hypercalcemia was 3.4 % in the placebo group and 8.3 % in the ALN group and those with MK5442: 18.4 % in the 5-mg group, 21.6 % in the 10-mg group, 31.0 % in the 10-mg group, and 44.3 % in the 15-mg group. Discontinuations due to persistent hypercalcemia (serum calcium ≥10.6 mg/dL in two measurements over 2 weeks) occurred almost exclusively among MK-5442-treated women and occurred more frequently among women receiving higher doses (Table 4). Most cases of hypercalcemia were apparent by month 3. All cases of hypercalcemia were asymptomatic.
Discussion
Women who were treated with bisphosphonates for at least 3 years and then switched to the calcilytic compound MK-5442 showed dose-dependent, pulsatile increases in serum PTH. Concordant with the PTH increases, BTMs increased with MK-5442 relative to both baseline and to placebo. In contrast, with all MK-5442 groups, BMD declined significantly in all skeletal sites compared to women who remained on ALN. The disappointing BMD findings in this trial are consistent with a short-term trial of MK5442 in a treatment-naïve osteoporotic population, where BMD did not increase significantly over 6 months in any of the dose groups [23]. The negative BMD results are also similar to the BMD decline observed with another calcilytic medication, ronacaleret [19].
Mean increments of 95 % for PINP and 85 % for sCTx above the increases that occurred with placebo treatment were seen in the 10-mg MK-5442 dose group at 12 months. Although we do not know how relative changes in biochemical markers of formation versus resorption relate to effects at the bone level, the proportionate increase in PINP relative to sCTx with MK5442 is smaller than that seen with exogenous PTH administration [10, 19, 24–26]. Furthermore, the adverse outcome of MK-5442 on BMD is distinct from the effect of daily exogenous administration of teriparatide. The absence of an anabolic effect of MK-5442 is likely due to differences in pharmacokinetics when stimulating endogenous PTH secretion (with MK-5442) compared with administering exogenous PTH. Although the maximal concentrations of PTH (1–84) or PTH (1–34) after treatment with MK-5442 or subcutaneous teriparatide, respectively, are similar (fourfold to fivefold above the upper limit of normal for serum PTH [15]), the duration of the PTH elevation is much longer for the endogenous PTH pulse in response to MK-5442. With teriparatide, PTH (1–34) levels are back to baseline within 3 to 4 h [27], whereas with MK5442, PTH levels were still elevated about twofold to threefold from baseline. Data from preclinical studies in animal models and organ cultures suggest that a longer duration of PTH elevation is more likely to be associated with bone resorption that exceeds bone formation [28–30]. Consistently, in the more extreme example of primary hyperparathyroidism, where serum PTH levels are elevated continuously, there is an overall catabolic effect on the skeleton, most prominent in cortical bone [31]. Furthermore, switching from ALN to MK-5442 5 mg or greater produced substantially more hypercalcemia, another indication of a prolonged PTH elevation, compared with exogenously administered teriparatide [27]. Ultimately, the optimal PTH pulse profile (duration and maximal concentration) for greatest potential to improve BMD is unknown.
There may also be differences in the effect of PTH (1–84) pulses produced endogenously compared with exogenous pulses of teriparatide, beyond just the duration of the PTH elevation. For example, a small open-label study comparing the effects of PTH (1–84) and PTH (1–34) on microarchitecture of the radius and tibia suggests that the 1–34 peptide increases cortical thickness whereas the 1–84 fragment does not [32]. Whether the difference was due to dose and duration of PTH exposure or qualitative differences between the effects of PTH (1–84) and (1–34) is uncertain. In addition, the lack of BMD improvement with MK-5442 may have been influenced by actions of the calcium-sensing antagonist outside of the parathyroid gland. The calcium-sensing receptor is expressed in the kidneys [33, 34] and by osteoblasts and osteocytes [35, 36], and antagonism of the receptor at these sites could affect bone turnover rates and/or remodeling balance.
Another consideration is whether adding MK-5442 to ongoing ALN might have produced a superior response, compared with switching to MK-5442. In a randomized trial, when ALN was switched to teriparatide, BMD effects were not as positive as when teriparatide was added to ongoing ALN. After the switch from ALN to teriparatide, hip BMD declined during the first year [10], and there was no increase in bone strength at the hip (estimated by finite element analysis) throughout an 18-month treatment period [11]. In contrast, areal and volumetric BMD as well as bone strength at the hip did increase in women who added teriparatide to ongoing ALN. However, in this trial, spine BMD did increase whether women switched to or added teriparatide. This was not true when switching from ALN to MK5442, where BMD did not increase in either the hip or spine. Nor did MK-5442 increase BMD at either spine or hip in a treatment-naïve population in another study [23].
There is clearly a need to develop anabolic agents for patients with osteoporosis who require a greater increase in bone mass than that produced by an initial course of antiresorptive therapy. This might turn out to be a bigger challenge than anticipated. The only generally available anabolic therapy, teriparatide, may not provide an optimal anabolic effect when given immediately after stopping bisphosphonate therapy, especially during the first year of administration. The calcilytic compound MK-5442 does not improve BMD at any skeletal site in bisphosphonate-treated patients and is clearly not a viable option for the treatment of these patients.
References
Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, Nevitt MC, Suryawanshi S, Cummings SR (2000) Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab 85:4118–24
Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA, Satterfield S, Wallace RB, Bauer DC, Palermo L, Wehren LE, Lombardi A, Santora AC, Cummings SR (2006) Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA 296:2927–38
Bone HG, Hosking D, Devogelaer JP, Tucci JR, Emkey RD, Tonino RP, Rodriguez-Portales JA, Downs RW, Gupta J, Santora AC, Liberman UA (2004) Ten years’ experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med 350:1189–99
McClung M, Recker R, Miller P, Fiske D, Minkoff J, Kriegman A, Zhou W, Adera M, Davis J (2007) Intravenous zoledronic acid 5 mg in the treatment of postmenopausal women with low bone density previously treated with alendronate. Bone 41:122–28
Kendler DL, Roux C, Benhamou CL, Brown JP, Lillestol M, Siddhanti S, Man HS, San Martin J, Bone HG (2010) Effects of denosumab on bone mineral density and bone turnover in postmenopausal women transitioning from alendronate therapy. J Bone Miner Res 25:72–81
Matheny JB, Slyfield CR, Tkachenko EV, Lin I, Ehlert KM, Tomlinson RE, Wilson DL, Hernandez CJ (2013) Anti-resorptive agents reduce the size of resorption cavities: a three-dimensional dynamic bone histomorphometry study. Bone 57(1):277–83
Roschger P, Rinnerthaler S, Yates J, Rodan GA, Fratzl P, Klaushofer K (2001) Alendronate increases degree and uniformity of mineralization in cancellous bone and decreases the porosity in cortical bone of osteoporotic women. Bone 29(2):185–91
Seeman E (2007) Is a change in bone mineral density a sensitive and specific surrogate of anti-fracture efficacy? Bone 41(1):308–17
Boonen S, Marin F, Obermayer-Pietsch B, Simoes ME, Barker C, Glass EV, Hadji P, Lyritis G, Oertel H, Nickelsen T, McCloskey EV (2008) Effects of previous antiresorptive therapy on the bone mineral density response to two years of teriparatide treatment in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 93(1):852–60
Cosman F, Wermers RA, Recknor C, Mauck KF, Xie L, Glass EV, Krege JH (2009) Effects of teriparatide in postmenopausal women with osteoporosis on prior alendronate or raloxifene: differences between stopping and continuing the antiresorptive agent. J Clin Endocrinol Metab 94:3772–80
Cosman F, Keaveny TM, Kopperdahl D, Wermers RA, Wan X, Krohn KD, Krege JH (2013) Hip and spine strength effects of adding versus switching to teriparatide in postmenopausal women with osteoporosis treated with prior alendronate or raloxifene. J Bone Miner Res 28:1328–36
Ettinger B, San Martin J, Crans G, Pavo I (2004) Differential effects of teriparatide on BMD after treatment with raloxifene or alendronate. J Bone Miner Res 19(2):745–51
Miller PD, Delmas PD, Lindsay R, Watts NB, Luckey M, Adachi J, Saag K, Greenspan SL, Seeman E, Boonen S, Meeves S, Lang TF, Bilezikian JP (2008) Early responsiveness of women with osteoporosis to teriparatide after therapy with alendronate or risedronate. J Clin Endocrinol Metab 93(1):3785–93
Cosman F (2014) Anabolic and Antiresorptive Therapy for Osteoporosis: Combination and Sequential Approaches. Curr Osteoporos Rep 12:385–95
Eli Lilly and Co. FORTEO (teriparatide). Prescribing Information. 2012; 1-13. http://www.pi.lilly.com/us/forteo-pi.pdf Accessed 05 November 2015.
Tashjian AH Jr, Gagel RF (2006) Teriparatide [human PTH(1–34)]: 2.5 years of experience on the use and safety of the drug for the treatment of osteoporosis. J Bone Miner Res 21:354–65
Canalis E, Giustina A, Bilezikian JP (2007) Mechanisms of anabolic therapies for osteoporosis. N Engl J Med 357:905–16
Cosman F, Lane NE, Bolognese MA, Zanchetta JR, Garcia-Hernandez PA, Sees K, Matriano JA, Gaumer K, Daddona PE (2010) Effect of transdermal teriparatide administration on bone mineral density in postmenopausal women. J Clin Endocrinol Metab 95:151–58
Fitzpatrick LA, Dabrowski CE, Cicconetti G, Gordon DN, Papapoulos S, Bone HG III, Bilezikian JP (2011) The effects of ronacaleret, a calcium-sensing receptor antagonist, on bone mineral density and biochemical markers of bone turnover in postmenopausal women with low bone mineral density. J Clin Endocrinol Metab 96:2441–49
Fukumoto S, Nakamura T, Nishizawa Y, Hayashi M, Matsumoto T (2009) Randomized, single-blinded placebo-controlled study of a novel calcilytic, JTT-305, in patients with postmenopausal osteoporosis. J Bone Miner Res 24 (Supp1 1)
Liang KY, Zeger SL (2000) Longitudinal data analysis of continuous and discrete responses for pre-post designs. Indian J Stat 62:134–48
Halse J, Greenspan S, Cosman F, Ellis G, Santora A, Leung A, Heyden N, Samanta S, Doleckyj S, Rosenberg E, Denker AE (2014) A phase 2, randomized, placebo-controlled, dose-ranging study of the calcium-sensing receptor antagonist MK-5442 in the treatment of postmenopausal women with osteoporosis. J Clin Endocrinol Metab. 99:E2207-15.
Halse J, Greenspan S, Cosman F, Ellis G, Rosenberg E, Heyden N DS, Samanta S, Weili H, Santora A, Leung A, Denker A (2012) A phase 2b, randomized, placebo-controlled, dose-ranging study of MK-5442 in the treatment of postmenopausal women with osteoporosis. J Bone Miner Res 27 (Suppl 1)
Ryder KM, Tanner SB, Carbone L, Williams JE, Taylor HM, Bush A, Pintea V, Watsky MA (2010) Teriparatide is safe and effectively increases bone biomarkers in institutionalized individuals with osteoporosis. J Bone Miner Metab 28:233–39
Anastasilakis AD, Goulis DG, Polyzos SA, Gerou S, Koukoulis GN, Efstathiadou Z, Kita M, Avramidis A (2008) Head-to-head comparison of risedronate vs. teriparatide on bone turnover markers in women with postmenopausal osteoporosis: a randomised trial. Int J Clin Pract 62:919–24
Tsujimoto M, Chen P, Miyauchi A, Sowa H, Krege JH (2011) PINP as an aid for monitoring patients treated with teriparatide. Bone 48:798–803
Satterwhite J, Heathman M, Miller PD, Marin F, Glass EV, Dobnig H (2010) Pharmacokinetics of teriparatide (rhPTH[1–34]) and calcium pharmacodynamics in postmenopausal women with osteoporosis. Calcif Tissue Int 87:485–92
Tam CS, Heersche JN, Murray TM, Parsons JA (1982) Parathyroid hormone stimulates the bone apposition rate independently of its resorptive action: differential effects of intermittent and continuous administration. Endocrinology 110:506–12
Hock JM, Gera I (1992) Effects of continuous and intermittent administration and inhibition of resorption on the anabolic response of bone to parathyroid hormone. J Bone Miner Res 7:65–72
Iida-Klein A, Lu SS, Kapadia R, Burkhart M, Moreno A, Dempster DW, Lindsay R (2005) Short-term continuous infusion of human parathyroid hormone 1–34 fragment is catabolic with decreased trabecular connectivity density accompanied by hypercalcemia in C57BL/J6 mice. J Endocrinol 186:549–57
Lewiecki EM, Miller PD (2013) Skeletal effects of primary hyperparathyroidism: bone mineral density and fracture risk. J Clin Densitom 16:28–32
Hansen S, Hauge EM, Beck Jensen JE, Brixen K (2013) Differing effects of PTH 1–34, PTH 1–84, and zoledronic acid on bone microarchitecture and estimated strength in postmenopausal women with osteoporosis: an 18-month open-labeled observational study using HR-pQCT. J Bone Miner Res 28:736–45
Brown EM, Pollak M, Hebert SC (1995) Molecular mechanisms underlying the sensing of extracellular Ca2+ by parathyroid and kidney cells. Eur J Endocrinol 132(1):523–31
Brown EM, MacLeod RJ (2001) Extracellular calcium sensing and extracellular calcium signaling. Physiol Rev 81:239–97
Marie PJ (2010) The calcium-sensing receptor in bone cells: a potential therapeutic target in osteoporosis. Bone 46:571–76
Xue Y, Xiao Y, Liu J, Karaplis AC, Pollak MR, Brown EM, Miao D, Goltzman D (2012) The calcium-sensing receptor complements parathyroid hormone-induced bone turnover in discrete skeletal compartments in mice. Am J Physiol Endocrinol Metab 302:E841–E851
Acknowledgments
The authors would like to thank Boyd B Scott, Ph.D., and Jennifer Pawlowski of Merck & Co. Inc. for their assistance in the preparation and submission of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
FC has received consulting, advisory board, and speaker’s bureau fees or honorarium from the study sponsor, Merck & Co. Inc. FC has received consulting, advisory board, and speaker’s bureau fees or honorarium from Amgen, Eli Lilly, Novartis, GSK, Tarsa, Zosano, Pfizer, Unigene, Asahi-Kasei, and Enteris. FC’s Institution has received grants from Merck, Amgen, Eli Lilly, and Novartis.
NG has received consultancy fees and speaker’s bureau fees from GGM.
MM has received consulting, advisory board, and honorarium from the study sponsor, Merck & Co. Inc. MM has received consulting, advisory board, and honorarium from Amgen and Eli Lilly.
JF has received speaker’s bureau fees or honorarium from Merck & Co. Inc. Institution has received grants from the study sponsor, Merck & Co. Inc.
TDV has received advisory board, travel support, and speaker’s bureau fees or honorarium from the study sponsor, Merck & Co. Inc. TDV has received advisory board, travel support, and speaker’s bureau fees or honorarium from Adcock Ingram, Servier, Amgen, and Pfizer.
Authors AD, NH, AL, ER, SS, JM, and AC are all employees of Merck & Co. Inc and may own stock or stock options.
Funding
This study was funded by Merck & Co. Inc. The study protocol was the responsibility of Merck & Co. Inc. and designed in collaboration with the steering committee composed of the academic authors and various health authorities. All analyses were conducted by scientists at Merck & Co. Inc. All authors had full access to the study data and vouch for the completeness of the data set and the performance of the data analyses. This study was registered with clinicaltrials.gov identifier: with registration number NCT00996801.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 1.52 mb)
Rights and permissions
About this article
Cite this article
Cosman, F., Gilchrist, N., McClung, M. et al. A phase 2 study of MK-5442, a calcium-sensing receptor antagonist, in postmenopausal women with osteoporosis after long-term use of oral bisphosphonates. Osteoporos Int 27, 377–386 (2016). https://doi.org/10.1007/s00198-015-3392-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3392-7