Abstract
Summary
At present, most hip fracture patients are treated in orthopaedic wards. This study showed that a relatively short hospital intervention based on principles of comprehensive geriatric assessment resulted in safer and more efficient gait as long as 1 year following the fracture as compared to conventional orthopaedic treatment.
Introduction
Hip fracture patients are frail, and the fracture is usually followed by substantial decline in gait function. Few studies have assessed gait characteristics other than gait speed and knowledge about the effect of early intervention on long-term gait outcome is sparse. The purpose of this study was to evaluate the long-term effect of pre- and post-surgery Comprehensive Geriatric Care (CGC) on ability to walk, self-reported mobility and gait characteristics in hip fracture patients.
Methods
Two armed, parallel group randomised controlled trial comparing CGC to conventional Orthopaedic Care (OC) in pre- and early post-surgery phase. Hip fracture patients (n = 397), community-dwelling, age >70 years and able to walk at time of the fracture were included. Spatial and temporal gait characteristics were collected using an instrumented walkway (GAITRite® system) 4 and 12 months post-surgery.
Results
Participants who received CGC had significantly higher gait speed, less asymmetry, better gait control and more efficient gait patterns, more participants were able to walk and participants reported better mobility 4 and 12 months following the fracture as compared to participants receiving OC.
Conclusions
Pre- and post-surgery CGC showed an effect on gait as long as 1 year after hip fracture. These findings underscore the importance of targeting the vulnerability of these patients at an early stage to prevent gait decline in the long run. As presently, most hip fracture patients are treated in orthopaedic wards with larger focus on the fracture than on frailty, these results are important to inform new models for hip fracture care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Safe and efficient gait is crucial for autonomy and quality of life in old age. Hip fractures are associated with a substantial decline in gait and represent a severe threat to health and wellbeing for older people. Hip fracture incidence rises exponentially with increasing age, with a reported residual life time risk in women older than 60 years of 44 % [1, 2]. With advances in surgical techniques, almost full recovery could be expected following a hip fracture. However, less than half of the hip fracture patients return to their prior level of function and the decline in health-related quality of life is considerable and long lasting [3]. Two years after a hip fracture, gait speed is considerably lower than in community-dwelling women at the same age [4]. Furthermore, a previous hip fracture is associated with an increased risk of new falls and injuries [5] and up to 90 % loose independence in daily tasks involving walking [6]. It remains unclear why there should be such a disproportionately large decline in gait function following a hip fracture, and there is also a lack of consensus about content and timing of interventions to maximise recovery of gait [7].
Frailty is defined as a state of vulnerability, an age-related increased risk of functional decline due to global deficiency of physiological reserves and reduced ability to respond adequately to stressors [8]. Hip fractures are closely related to reduced health and function [9–12], and a recent study reported about two thirds of hip fracture patients to be classified with moderate or high levels of frailty [13].
This suggests that older people who sustain hip fractures are especially vulnerable and at high risk of functional decline caused by inability to respond adequately to the strain the injury represents. Comprehensive Geriatric Care is a multidimensional and multidisciplinary approach targeting frailty. The long-term effect on function in geriatric patients is well documented [14], and similar approaches have been shown to improve outcomes also in hip fracture patients [15]. However, the knowledge is sparse concerning the long-term effect of early comprehensive geriatric care on the recovery of gait, and few intervention studies in hip fracture patients have included measures of gait characteristics beyond gait speed.
Gait is not a unitary concept. Relatively independent domains of gait (pace, rhythm, variability, postural control and asymmetry) have been identified [16], and age-related changes in spatial and temporal gait characteristics have been linked to reduced gait control and efficiency in older people [17]. Increased knowledge on the effect of various interventions on specific gait characteristics may contribute to the development of better targeted and more effective treatment and rehabilitation models in the future.
We have recently performed the Trondheim Hip Fracture Trial, a randomised controlled trial primarily designed to test the effect of being treated in an orthogeriatric versus an orthopaedic ward on mobility 4 and 12 months after the fracture. The main paper from the trial has been published [18]. The current paper reports secondary outcomes on gait not reported earlier and have the following aims: to compare long-term effect of pre- and post-surgery Comprehensive Geriatric Care (CGC) vs. conventional Orthopaedic Care (OC) on ability to walk, self-reported mobility and gait characteristics.
Method
Design overview
The Trondheim Hip Fracture Trial is a single centre, prospective, two armed, block randomised, parallel group, controlled trial. The present study on gait was a part of the Trondheim Hip Fracture Trial and included all patients in the main study, including those who lost ability to walk during follow-up.
Setting and participants
The study took place at St. Olav University Hospital from April 2008 to December 2010. St. Olav is the regional hospital for the population of Sør-Trøndelag with 302,000 inhabitants and performs about 400 surgical procedures related to hip fractures each year. The geriatric evaluation and management ward has existed since 1994 and has been shown to be effective in reducing mortality and in increasing number of acutely sick and frail older patients living at home [19–21]. Between 2008 and 2011, five out of 15 beds in the department were dedicated to hip fracture patients, in order to evaluate the effect of the new service delivery model. In Norway length of hospital stay after a hip fracture is restricted to the acute and sub-acute phase, and patients are typically transferred to a rehabilitation institution or a nursing home within a few days after surgery.
This study was powered to detect group difference in the primary outcome of the Trondheim Hip Fracture Trial, the Short Physical Performance Battery. Expecting a drop-out rate of 20 %, with α level of 0.05 and 80 % power, 380 patients were needed to confirm a clinically meaningful difference of 1 point between groups on the Short Physical Performance Battery 4 months after the fracture [22].
Inclusion criteria were confirmed hip fracture (ICD-10 72.0–72.2), age 70 years or older, able to walk 10 m prior to the hip-fracture and being community-dwelling at time of the fracture. Exclusion criteria were life expectancy less than 3 months, pathological fractures and high energy trauma.
Randomisation and interventions
Randomisation was performed using a web-based computerised randomisation service developed by and administrated from the Unit of Applied Clinical Research at the Norwegian University of Science and Technology (NTNU). A computer generated randomisation sequence was prepared by the Unit of Applied Clinical research and kept sealed until inclusion was closed and the data analysis plan finalised.
All patients with a confirmed hip fracture were approached by a nurse in the emergency room. If confirmed eligible, informed written consent was collected from the patient or the next of kin. Once included in the trial, the staff in the emergency room accessed the web-based computer programme. The programme randomly assigned patients to receive pre- and post-surgery CGC or orthopaedic care OC in a ratio of 1:1. Patients were transferred directly to the allocated ward for pre-operative care.
Patients were allocated to either conventional OC in an orthopaedic ward or CGC in a geriatric ward. Both pre- and postoperative care was provided at the allocated ward. Details of the intervention are described elsewhere [23]. In short, CGC is based on multidimensional assessment of somatic and mental health, mobility, ADL and social situation using standardised assessment protocols resulting in an individualised treatment and rehabilitation plan. The intervention was delivered by a multidisciplinary team consisting of geriatricians, physiotherapists, occupational therapists and registered and assistant nurses specialised within geriatric medicine. The care had specific focus on early mobilisation and rehabilitation. Short- and long-term goals were set for each patient in collaboration between the patient, next of kin and the team and were based on prefracture function, home condition, cognitive function and current medical condition. Evaluation of progress and adjustment of goals and treatment plan were performed continuously during formal meetings in the team. Discharge planning was focused from day 1 post-surgery and involved next of kin and primary health care if necessary. Physiotherapy within 2 weeks after discharge or a home-based rehabilitation team following the patient from discharge was arranged for all patients who went directly home. All patients discharged to rehabilitation institutions or nursing homes were followed by a report including the results of the geriatric assessment, description of progress and expected prognosis.
In the geriatric ward, the hip fracture patients were clustered in a separate unit with five single-bed rooms dedicated to older fracture patients and staffed with dedicated personnel. Physical environments were facilitated with regards to delirium prophylaxis. Ward routines were developed to enhance physical activity with a specific focus on splitting up long periods of sitting and lying. Meals were served in the dining room instead of the patient rooms, and patients were encouraged to use the communal areas.
Daily evaluations of need for physiotherapy were part of the routine. Patients that did not progress as expected according to the care plan were given higher priority, as were patients with special challenges like restrictions on weight bearing. Exercises performed during the hospital stay, instructions for a home-based exercise programme and written information provided by the physiotherapist were based on procedures from the orthopaedic department. In addition, goals and plans for mobilisation and training of activities of daily living, including progression, were described as part of the care plan and evaluated continuously. Mobilisation and practicing relevant daily activities were a common responsibility for the team, commonly performed in collaboration between physiotherapists and nurses in the beginning, and then managed by the care personnel as routines and methods were established. Beyond this, there was no additional focus on specific exercises aimed to improve gait control.
Patients in the orthopaedic ward received conventional care according to national and international standards, including mobilisation within 24 h post-surgery [23]. Hip fracture patients stayed in a mixed unit with orthopaedic trauma patients. Geriatricians acted as consultants on request in a few patients. Physiotherapy was routinely requested for all patients and delivered by physiotherapists who were organised in a separate unit serving several departments. There was no structured multidisciplinary collaboration or regular meetings for common goal setting and information about individual patients was passed informally. Physiotherapy included the same exercise programme, instruction in home exercises and written information as in the geriatric ward. The physiotherapists had the main responsibility for practicing walking and adjusting walking aids. Prioritising of patients was based on the individual physiotherapist’s evaluation of the patient’s potential. Discharge planning was mainly the responsibility of the nurse. Patients discharged directly to their homes were provided a requisition for physiotherapy and had to arrange for appointments on their own. Patients discharged to institutions were followed by a short medical report.
Number of staff per patient bed was higher in the geriatric ward as compared to the orthopaedic ward; nurses 1.67 vs. 1.48, doctors 0.13 vs. 0.11, physiotherapists 0.13 vs. 0.09 and occupational therapist 0.13 vs. 0.0 [18].
Outcomes and follow-up
Assessments at 4 and 12 months were performed at the geriatric outpatient clinic at the hospital. Assessments were performed by assessors not involved in the patient care. Blinding was not possible for staff that provided the intervention, study participants or assessors during the hospital stay. Assessments performed after discharge were performed without knowledge of group allocation, but with some assessments performed by the same assessors both in hospital and at follow-ups. A standardised test battery, fixed protocols, procedures and instructions were used to minimise the influence of the assessor. Data processing and the first data analysis were performed blinded for group allocation.
Gait characteristics were measured over an 8 m (4.88 m active area) instrumented walkway, the GAITRite® mat (CIR systems Inc. Havertown, PA). Participants walked back and forth at self-selected preferred speed, starting from a standing position. Walking aids were permitted only when the participants were unable to walk without an aid.
A large number of gait variables can be extracted from the GAITRite system. Gait speed is regarded an indicator of overall health and function, sensitive to change in function and recommended to use as outcome in frail populations [24]. To cover aspects of gait beyond gait speed, the following gait variables were selected; speed and step length to represent pace; cadence, double support time and percentage of single support to represent rhythm; step width and walk ratio (step length/cadence) [25, 26] to represent postural control; standard deviation of step velocity to represent gait variability and single support asymmetry to represent gait asymmetry.
A relatively large proportion of patients was expected to either die, loose their ability to walk or be unable to perform a full gait assessment during the follow-up period. It was deemed important to be able to describe the full range of participants according to gait function, and therefore, participants who were not able or unwilling to attend the outpatient clinic were offered a home visit with a reduced test protocol including a 4-m gait speed test, but not the GAITRite assessment. Accordingly, five participant categories would be present at each follow-up: (1) those performing the GAITRite assessment, (2) those performing a reduced protocol including the 4-m gait speed test, (3) those unable to walk, (4) those deceased within the follow-up period and (5) drop-outs.
Pre-fracture function was assessed through recall from the patient or next of kin using the Barthel Index [27], the Nottingham E-ADL scale [28] and the Clinical Dementia Rating scale [29]. Independence in mobility 4 and 12 months post-surgery was assessed by the mobility subscale of the Nottingham E-ADL scale.
Statistical analysis
Data from the GAITRite mat were processed using the PKmas® (ProtoKinetics, Havertown, PA) software, which is a new programme developed to improve the processing of difficult footstep patterns from electronic gait mats. Outcomes derived from the PKmas and the GAITRite software have been shown to be comparable at group level for most variables [30]. Means, standard deviations and left/right ratio of steps were calculated by the software and exported to Microsoft Excel® for further calculations of walk ratio (step length/cadence) and single support asymmetry: 100x|ln(left/right)| [31]. For the variability measures, standard deviations of the gait variables for left and right sides were calculated separately and then averaged to avoid an effect of asymmetry on the variability outcomes.
The intervention had the potential to affect the number of patients who ended up in each of the five predefined categories, and consequently, it was important to investigate to which extent missing data were informative or not. Our approach was to first characterise the differences in pre-fracture function between the five participant categories. We then conducted two analyses: a primary analysis where we transformed the data into ordinal scaled data and included participants who had lost their ability to walk, and a secondary complete case analysis based on the continuously scaled data. In the primary analysis, continuously scaled data were transformed into a 1–4 point ordinal scale using cut points based on quartiles for the OC-group. Participants unable to walk were provided a value of zero which resulted in a five point scale, with higher scores indicating better function. We then performed a sensitivity analysis where people who died during follow-up were added to the category of zero.
All statistical analyses were performed using SPSS Inc. (SPSS Statistics for Windows, Version 21.0. Chicago: SPSS Inc.). Descriptive statistics are reported as means and standard deviations. Normality of gait variable distributions was checked by inspection of Q-Q plots and by the Kolmogorov-Smirnov test. Most gait variables had a skewed distribution, and the nonparametric Mann–Whitney U test was therefore used to test for group differences. Outcomes are reported as median and interquartile range. Differences in outcomes between participants with complete and missing data were tested with a one-way ANOVA, using the post hoc Gams-Howell test. Group differences for categorical variables were tested by Pearson’s chi-square test.
Ethics
This study complies with the ethical rules for human experimentation as stated in the Declaration of Helsinki and has been approved by the Regional Committee of Ethics in Medical Research (REK 4.2008.335), the Norwegian Social Science Data Service (NSD19109) and the Norwegian Directorate of Health (08/5814).
Funding source
The research was supported by Norwegian Research Council, The Liaison Committee between the Central Norway Regional Health Authority (RHA) and the Norwegian University of Science and Technology (NTNU), the Norwegian Women’s Health Association, the Norwegian Extra Foundation for Health and Rehabilitation through the EXTRA funds and The Norwegian Fund for Post-Graduate Training in Physiotherapy.
Results
A total of 397 participants were randomised between April 18th, 2008 and 30th of December, 2010. Prefracture function and sample characteristics according to allocation are presented in Table 1 and show that treatment arms were comparable. The length of stay was slightly longer in the geriatric ward: 12.6 (SD 0.4) vs. 11.0 (SD 0.5) days in the orthopaedic ward. Preoperative waiting time (29.0 (SD 23.3) h) was similar for the OC and the CGC group. More patients in the CGC group were discharged directly home: 25 % as compared to 11 % in the orthopaedic group [20].
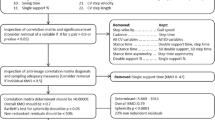
Patient flow through the study is described in Fig. 1. Two hundred and fifty-four participants (64 %) at 4 months and 228 participants (57 %) at 12 months underwent gait assessment with the GAITRite system.
Table 2 shows pre-fracture function according to the five participant categories present at 12 months follow-up and illustrates that participants who performed a reduced protocol, were unable to walk or had deceased, had poorer prefracture function as compared to participants who performed the GAITRite assessment. Prefracture function for those unable to walk at 12 months and prefracture cognitive function among drop-outs tended to be lower in the OC-group as compared to the CGC-group, indicating that data were not missing at random.
Significantly more participants in the CGC group were able to perform either the GAITRite or the 4-m gait speed test both at 4 months (p = 0.049) and at 12 months (p = 0.005). At 12 months, 63 % (124/198) of participants in the CGC group and 52 % (104/199) in the OC group performed the GAITRite assessment (p = 0.037). In the CGC group, 80 % (99/124) were able to walk without walking aids during the test, while 69 % (72/104) walked unsupported in the OC group, (p = 0.065). Among those unable to perform the GAITRite assessment, 10 % (20/198) in the CGC group and 7 % (14/199) in the OC group were still able to perform the 4-m gait speed test (p = 0.275). In the OC group, 8 % (16/199) were unable to walk and in the CGC group 5 % (9/198), (p = 0.152). In the OC group, 19 % (37/199) had deceased within 12 months compared to 15 % (29/198) in the CGC group (p = 0.291). In the OC group, 14 % (28/199) had withdrawn compared to 8 % (16/198) in the CGC group (p = 0.057).
At 4 months, the proportion unable to walk was 4 % (7/198) in the CGC-group and 11 % (21/199) in the OC group, p = 0.006. The proportion able to walk without walking aids during the test was 81 % (107/132) in the CGC group and 66 % (80/122) in the OC group, p = 0.006.
The primary analysis showed better gait characteristics at both 4 and 12 months in the CGC group compared to the OC group, for all gait variables except variability (Table 3). These results did not change when including the deceased in the analysis. A complete case analysis provided similar results as for the primary analysis for the 12 months data, but did not reach significance level at 4 months.
Table 4 shows higher scores on the mobility sub-scale of the Nottingham E-ADL scale at 12 months and a tendency towards more participants reporting walking independently both in- and outdoor in the CGC group as compared to the OC group.
Adverse events
Mortality rates were closely monitored according to predefined criteria [24]. No adverse events were reported.
Discussion
This study aimed to evaluate the long-term effect of CGC on gait 4 and 12 months following hip fracture. To our knowledge, this is the first clinical trial assessing the effects of intervention on other gait characteristics than gait speed in hip fracture patients. We found that more participants in the CGC group preserved their ability to walk, that gait characteristics indicated better gait control and efficiency and that participants reported better mobility as compared to the OC group as long as 1 year following the fracture as a result of a relatively short intervention focusing on interdisciplinary management.
Group differences in pace and rhythm, i.e., lower gait speed, shorter steps and longer double support time, indicate reduced gait control and higher fall risk [32] in the OC group 4 and 12 months following the fracture. Reduced walk ratio and increased step width further suggest that participants in the OC group have reduced postural control and use more compensating strategies to secure gait as compared to the CGC group [33, 34]. These compensating strategies are associated with higher energy costs of walking [35, 36]. High energy costs of walking are related to activity avoidance and reduced function [37] and could be part of the explanation why participants in the CGC group reported better quality of life and more independence in daily life activities [18]. Persistent asymmetry in weight loading and in quadriceps strength has been found in hip fracture patients [38] and has been used as an argument for the relevance of early and high dose progressive strength training in hip fracture patients [39]. Our results suggest that targeting frailty in an early stage has a long-term effect on gait asymmetry.
The mean group difference of 0.08 m/s in gait speed at 12 months is below the 0.1 m/s that is regarded as a clinically meaningful difference in gait speed [40]. However, a higher proportion of participants in the CGC group performed the gait assessment at 12 months. Prefracture function indicate that it was the participants with low prefracture function that were lost to follow-up in the OC group, thereby likely resulting in an attrition bias. In addition, more participants in the OC group were using walking aids as they were not able to walk unassisted. The group difference is therefor most likely underestimated which also may explain the relatively low effect sizes. Clinical relevance of the group differences is supported by the findings of a higher number of participants who preserved ability to walk and better self-reported mobility in the CGC group.
CGC is a complex multicomponent intervention and a combination of factors can possibly explain the effects. Results from activity monitoring on day 4 post-surgery in the Trondheim Hip Fracture Trial have been published earlier and show higher activity level and activity being more spread throughout the day in the geriatric ward [41]. These findings suggest that mobilisation strategies were more successful for the CGC group. The comprehensive assessment and the team approach likely provided more structured and individualised mobilisation and care of the patients and allowed for more well-founded and planned prioritising of patients that needed special attention, especially those with cognitive decline. Lower prefracture cognitive function and ADL function in the OC group among participants who lost ability to walk is an indication that this strategy was successful and that CGC resulted in more of the most vulnerable participants being able to preserve the ability to walk. The organisation of physical therapy as an external service in the orthopaedic ward may not have allowed for the same systematic and coordinated approach and likely resulted in more ad hoc prioritising of patients and less total activity and less walking integrated in daily life activities during the stay as compared to the geriatric ward.
Returning home after a hip fracture is a critical phase associated with lack of confidence and reduced participation [42]. A higher percentage of participants in the CGC-group was able to return directly home. It is likely that patients receiving CGC were more prepared for the home setting due to an explicit focus on progressive ADL training throughout the stay and systematic early discharge planning that involved relatives and primary care.
More staff resources and slightly longer length of stay in the CGC group resulted in higher costs of the index stay. However, cost-effectiveness analysis reported in the main paper showed that despite increased costs of the index stay, CGC is cost effective and has an 88 % probability of being both less costly and more effective than orthopaedic care in the long run [18].
A limitation of this study is the lack of formal blinding. However, the use of standardised tests and instructions should reduce the risk of tester bias and there were indeed no indications of such, the same trends were found for data collected through registers and from more objective data like activity monitoring. Another limitation is the amount of participants not able to perform the GAITRite assessment, which could question the suitability of data from instrumented walkways used as outcome in frail populations with an expected high rate of loss to follow up. Our approach was to carefully register reasons for inability to perform the test and invest effort to obtain a minimum of data on gait by offering a home-based test protocol for those unable to attend the outpatient clinic. These procedures allowed for a relatively comprehensive and detailed description of gait following hip fracture which has not been presented earlier.
The strengths of this trial are the randomised controlled design, the large sample size, few exclusion criteria, high retention rate when taking the population into consideration and a relatively long follow-up period.
Missing data is a general challenge in research on frail populations, but it is important to recognise that patterns of missing data could be informative as demonstrated in this study. Our analysis of patterns of missing data indicated that data were not missing at random and common methods like multiple imputation could not be applied. Our analysis strategy partly solved this problem by including a category of zero for those unable to walk, but we were not able to account for those performing only the reduced gait protocol, the drop-outs or the higher percentage in the OC group who were unable to walk without walking aids. Nevertheless, we believe we have accounted for the most influential causes of bias, and if any should remain, rather underestimated than overestimated the treatment effect.
Conclusion
This randomised controlled trial demonstrates that CGC including a team-based, structured and individualised approach to mobilisation, resulted in better gait control, gait efficiency and self-reported mobility as long as 1 year following the fracture. These results underscore the close association of health and gait functions and raise important issues concerning how to maximise gait recovery after hip fracture. Targeting the frailty of these patients in a very early stage seems to reduce the initial decline in gait function and perhaps make them more susceptible to rehabilitation and exercise at a later stage. Further research is needed to evaluate the added effect of exercises programmes designed to target gait control specifically.
References
Nguyen ND, Ahlborg HG, Center JR, Eisman JA, Nguyen TV (2007) Residual lifetime risk of fractures in women and men. J Bone Miner Res 22(6):781–788. doi:10.1359/jbmr.070315
Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256. doi:10.1007/s00198-012-1964-3
Wehren LE, Magaziner J (2003) Hip fracture: risk factors and outcomes. Curr Osteoporos Rep 1(2):78–85
Fredman L, Magaziner J, Hawkes W, Hebel JR, Fried LP, Kasper J, Guralnik J (2005) Female hip fracture patients had poorer performance-based functioning than community-dwelling peers over 2-year follow-up period. J Clin Epidemiol 58(12):1289–1298. doi:10.1016/j.jclinepi.2004.04.016
Lloyd BD, Williamson DA, Singh NA, Hansen RD, Diamond TH, Finnegan TP, Allen BJ, Grady JN, Stavrinos TM, Smith EU, Diwan AD, Fiatarone Singh MA (2009) Recurrent and injurious falls in the year following hip fracture: a prospective study of incidence and risk factors from the sarcopenia and Hip fracture study. J Gerontol A: Biol Med Sci 64(5):599–609. doi:10.1093/gerona/glp003
Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M, Felsenthal G, Kenzora J (2000) Recovery from hip fracture in eight areas of function. J Gerontol A: Biol Med Sci 55(9):M498–M507
Handoll HH, Sherrington C, Mak JC (2011) Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst Rev 3:CD001704. doi:10.1002/14651858.CD001704.pub4
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381(9868):752–762. doi:10.1016/S0140-6736(12)62167-9
Hannan EL, Magaziner J, Wang JJ, Eastwood EA, Silberzweig SB, Gilbert M, Morrison RS, McLaughlin MA, Orosz GM, Siu AL (2001) Mortality and locomotion 6 months after hospitalization for hip fracture: risk factors and risk-adjusted hospital outcomes. JAMA 285(21):2736–2742
Maggi S, Siviero P, Wetle T, Besdine RW, Saugo M, Crepaldi G, Hip Fracture Study G (2010) A multicenter survey on profile of care for hip fracture: predictors of mortality and disability. Osteoporos Int 21(2):223–231. doi:10.1007/s00198-009-0936-8
Osnes EK, Lofthus CM, Meyer HE, Falch JA, Nordsletten L, Cappelen I, Kristiansen IS (2004) Consequences of hip fracture on activities of daily life and residential needs. Osteoporos Int 15(7):567–574. doi:10.1007/s00198-003-1583-0
Penrod JD, Litke A, Hawkes WG, Magaziner J, Doucette JT, Koval KJ, Silberzweig SB, Egol KA, Siu AL (2008) The association of race, gender, and comorbidity with mortality and function after hip fracture. J Gerontol A: Biol Med Sci 63(8):867–872
Krishnan M, Beck S, Havelock W, Eeles E, Hubbard RE, Johansen A (2014) Predicting outcome after hip fracture: using a frailty index to integrate comprehensive geriatric assessment results. Age Ageing 43(1):122–126. doi:10.1093/ageing/aft084
Bachmann S, Finger C, Huss A, Egger M, Stuck AE, Clough-Gorr KM (2010) Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ 340:c1718. doi:10.1136/bmj.c1718
Stenvall M, Olofsson B, Nyberg L, Lundstrom M, Gustafson Y (2007) Improved performance in activities of daily living and mobility after a multidisciplinary postoperative rehabilitation in older people with femoral neck fracture: a randomized controlled trial with 1-year follow-up. J Rehabil Med 39(3):232–238. doi:10.2340/16501977-0045
Lord S, Galna B, Verghese J, Coleman S, Burn D, Rochester L (2013) Independent domains of gait in older adults and associated motor and nonmotor attributes: validation of a factor analysis approach. J Gerontol A: Biol Med Sci 68(7):820–827. doi:10.1093/gerona/gls255
VanSwearingen JM, Studenski SA (2014) Aging, motor skill, and the energy cost of walking: implications for the prevention and treatment of mobility decline in older persons. J Gerontol A: Biol Med Sci. doi:10.1093/gerona/glu153
Prestmo A, Hagen G, Sletvold O, Helbostad JL, Thingstad P, Taraldsen K, Lydersen S, Halsteinli V, Saltnes T, Lamb SE, Johnsen LG, Saltvedt I (2015) Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet. doi:10.1016/S0140-6736(14)62409-0
Saltvedt I, Jordhoy M, Opdahl Mo ES, Fayers P, Kaasa S, Sletvold O (2006) Randomised trial of in-hospital geriatric intervention: impact on function and morale. Gerontology 52(4):223–230. doi:10.1159/000093654
Saltvedt I, Mo ES, Fayers P, Kaasa S, Sletvold O (2002) Reduced mortality in treating acutely sick, frail older patients in a geriatric evaluation and management unit. A prospective randomized trial. J Am Geriatr Soc 50(5):792–798
Saltvedt I, Saltnes T, Mo ES, Fayers P, Kaasa S, Sletvold O (2004) Acute geriatric intervention increases the number of patients able to live at home. A prospective randomized study. Aging Clin Exp Res 16(4):300–306
Sletvold O, Helbostad JL, Thingstad P, Taraldsen K, Prestmo A, Lamb SE, Aamodt A, Johnsen R, Magnussen J, Saltvedt I (2011) Effect of in-hospital comprehensive geriatric assessment (CGA) in older people with hip fracture. The protocol of the Trondheim Hip fracture trial. BMC Geriatr 11:18. doi:10.1186/1471-2318-11-18
Saltvedt I, Prestmo A, Einarsen E, Johnsen LG, Helbostad JL, Sletvold O (2012) Development and delivery of patient treatment in the Trondheim Hip fracture trial. A new geriatric in-hospital pathway for elderly patients with hip fracture. BMC Res Not 5:355. doi:10.1186/1756-0500-5-355
Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, Cesari M, Donini LM, Gillette Guyonnet S, Inzitari M, Nourhashemi F, Onder G, Ritz P, Salva A, Visser M, Vellas B (2009) Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an international academy on nutrition and aging (IANA) task force. J Nutr Health Aging 13(10):881–889
Callisaya ML, Blizzard L, McGinley JL, Srikanth VK (2012) Risk of falls in older people during fast-walking—the TASCOG study. Gait Posture 36(3):510–515. doi:10.1016/j.gaitpost.2012.05.003
Zijlstra A, de Bruin ED, Bruins N, Zijlstra W (2008) The step length-frequency relationship in physically active community-dwelling older women. Eur J Appl Physiol 104(3):427–434. doi:10.1007/s00421-008-0795-6
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Nouri FM, Lincoln NB (1987) An extended activities of daily living scale for stroke patients. Clin Rehabil 1:301–305
Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL (1982) A new clinical scale for the staging of dementia. Br J Psychiatry 140:566–572
Egerton T, Thingstad P, Helbostad JL (2014) Comparison of programs for determining temporal-spatial gait variables from instrumented walkway data: PKmas versus GAITRite. BMC Res Not 7(1):542. doi:10.1186/1756-0500-7-542
Yogev G, Plotnik M, Peretz C, Giladi N, Hausdorff JM (2007) Gait asymmetry in patients with Parkinson’s disease and elderly fallers: when does the bilateral coordination of gait require attention? Exp Brain Res 177(3):336–346. doi:10.1007/s00221-006-0676-3
Verghese J, Holtzer R, Lipton RB, Wang C (2009) Quantitative gait markers and incident fall risk in older adults. J Gerontol A: Biol Med Sci 64(8):896–901. doi:10.1093/gerona/glp033
Hak L, Houdijk H, Steenbrink F, Mert A, van der Wurff P, Beek PJ, van Dieen JH (2012) Speeding up or slowing down?: gait adaptations to preserve gait stability in response to balance perturbations. Gait Posture 36(2):260–264. doi:10.1016/j.gaitpost.2012.03.005
Hof AL (2008) The’extrapolated center of mass’ concept suggests a simple control of balance in walking. Hum Mov Sci 27(1):112–125. doi:10.1016/j.humov.2007.08.003
Wert DM, Brach J, Perera S, VanSwearingen JM (2010) Gait biomechanics, spatial and temporal characteristics, and the energy cost of walking in older adults with impaired mobility. Phys Ther 90(7):977–985. doi:10.2522/ptj.20090316
Schrack JA, Simonsick EM, Ferrucci L (2010) The energetic pathway to mobility loss: an emerging new framework for longitudinal studies on aging. J Am Geriatr Soc 58(Suppl 2):S329–S336. doi:10.1111/j.1532-5415.2010.02913.x
Wert DM, Brach JS, Perera S, VanSwearingen J (2013) The association between energy cost of walking and physical function in older adults. Arch Gerontol Geriatr 57(2):198–203. doi:10.1016/j.archger.2013.04.007
Nightingale EJ, Sturnieks D, Sherrington C, Moseley AM, Cameron ID, Lord SR (2010) Impaired weight transfer persists at least four months after hip fracture and rehabilitation. Clin Rehabil 24(6):565–573. doi:10.1177/0269215509360753
Kronborg L, Bandholm T, Palm H, Kehlet H, Kristensen MT (2014) Feasibility of progressive strength training implemented in the acute ward after hip fracture surgery. PLoS One 9(4):e93332. doi:10.1371/journal.pone.0093332
Perera S, Mody SH, Woodman RC, Studenski SA (2006) Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 54(5):743–749. doi:10.1111/j.1532-5415.2006.00701.x
Taraldsen K, Sletvold O, Thingstad P, Saltvedt I, Granat MH, Lydersen S, Helbostad JL (2014) Physical behavior and function early after hip fracture surgery in patients receiving comprehensive geriatric care or orthopedic care—a randomized controlled trial. J Gerontol A: Biol Med Sci 69(3):338–345. doi:10.1093/gerona/glt097
Taylor NF, Barelli C, Harding KE (2010) Community ambulation before and after hip fracture: a qualitative analysis. Disabil Rehabil 32(15):1281–1290. doi:10.3109/09638280903483869
Acknowledgments
We thank the patients and their relatives for their participation, the staff at the wards for collaboration, our taxi driver and the GEMS research group for their contribution to the completion of the trial.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thingstad, P., Taraldsen, K., Saltvedt, I. et al. The long-term effect of comprehensive geriatric care on gait after hip fracture: the Trondheim Hip Fracture Trial—a randomised controlled trial. Osteoporos Int 27, 933–942 (2016). https://doi.org/10.1007/s00198-015-3313-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3313-9