Abstract
Summary
We evaluated the correlation between central bone mineral density (BMD) and peripheral bone attenuation using lower extremity computed tomography (CT). A good correlation was found between lower extremity CT and central BMD suggesting that CT is useful for screening osteoporosis, and that peripheral bone attenuation adequately reflects central BMD.
Introduction
This study aimed to evaluate the reliability and validity of CT as a screening tool for osteoporosis and to estimate the correlation between central BMD and peripheral bone attenuation using lower extremity CT.
Methods
In total, 292 patients who underwent a lower extremity, lumbar spine, or abdomen and pelvic CT scan within a 3-month interval of a dual-energy X-ray absorptiometry (DEXA) examination were included. Following reliability testing, bone attenuation of the L1, L2, L3, L4, femoral head, femoral neck, greater trochanter, distal femur, proximal tibia, distal tibia, and talus was measured by placing a circular region of interest on the central part of each bony region on a coronal CT image. Partial correlation was used to assess the correlation between CT and DEXA after adjusting for age and body mass index.
Results
In terms of reliability, all bone attenuation measurements, except the femoral neck, showed good to excellent interobserver reliability (intraclass correlation coefficients, 0.691–0.941). In terms of validity, bone attenuation of the L1 to L4, femoral neck, and greater trochanter on CT showed significant correlations with BMD of each area on DEXA (correlation coefficients, 0.399–0.613). Bone attenuation of the distal tibia and talus on CT showed significant correlations with BMD of all parts on DEXA (correlation coefficients, 0.493–0.581 for distal tibia, 0.396–0.579 for talus).
Conclusion
Lower extremity CT is a useful screening tool for osteoporosis, and peripheral bone attenuation on lower extremity CT adequately reflects central BMD on DEXA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis—often called “the silent disease”—is a serious disease with high morbidity and mortality caused by fragility fracture, especially of the hip and spine [1, 2]. Unfortunately, the prevalence of osteoporosis has increased [3], and the incidence is expected to increase further with the aging of society [4]. Although several diagnostic and screening tools for assessing bone mineral density (BMD) are currently available [5], dual-energy X-ray absorptiometry (DEXA) of the central skeleton is considered the gold standard. The World Health Organization’s international reference standard for diagnosing osteoporosis is assessment at the femoral neck; the lumbar spine also can be assessed in postmenopausal women and in men aged 50 y and older [6].
DEXA for osteoporosis screening is generally performed in older patients. Consequently, younger patients with decreased BMD can be overlooked. In addition, because the measurement area in DEXA is limited to the central skeleton, peripheral BMD is not screened. Recently, assessment of peripheral BMD has grown in importance since peripheral bone fracture can have features of osteoporotic fracture, which is characterized by age- and sex-dependent low bone attenuation [2].
Computed tomography (CT) is performed for a variety of reasons. Previous studies have shown a correlation in BMD between CT and DEXA [7, 8]. These findings demonstrate the potential of CT as a screening tool for osteoporosis. However, the assessment correlation of BMD in those studies was performed in only the spine. Therefore, we performed this study to evaluate the reliability and validity of CT as a screening tool for osteoporosis and to estimate the correlation between central BMD and peripheral bone attenuation using lower extremity CT.
Materials and methods
This retrospective study was approved by the Institutional Review Board of our hospital. Informed consent was waived because of the retrospective nature of this study.
We reviewed the medical records of consecutive patients who underwent BMD assessment by central DEXA at our institution between May 2004 and February 2014. Patients who also underwent a lower extremity, lumbar spine, or abdomen and pelvic CT scan within a 3-month interval of their DEXA examination were included. The exclusion criteria were as follows: (1) patients who suffered a fracture that precluded measurement; (2) inadequate CT scan available for review, including previous surgery or other condition that affected the measurement site; and (3) patients who underwent CT at another institution. Demographic data, including age and sex, and diagnosis, categorized by location of disease or trauma, were collected by medical record and CT image review. BMD studies were performed using Discovery W (Hologic Inc., Bedford, MA, USA) with standard protocols. CT studies were performed using Light-Speed VCT (GE Healthcare, Milwaukee, WI, USA) with 120 kVp, and 1.25-mm-slice thickness for the hip and pelvis, and 0.625-mm-slice thickness for the ankle, tibia, knee, and spine. CT was performed with patients in the supine position. All CT images were digitally acquired using a picture archiving and communication system (STARPACS; Infinitt, Seoul, Korea), and measurements were subsequently carried out using PACS software.
Reliability test and measurement of parameters
Five surgeons with 30, 11, 10, 5, and 4 years of orthopedic experience, respectively, held a consensus-building session before measuring the CT images. Since the literature did not describe the measurement sites or the methods for assessing bone attenuation of the lower extremity, the panel decided that bone attenuation around the hip, knee, and ankle would be measured on CT images. After consensus building, reliability testing was conducted before the main measurements. Interobserver reliability was determined using intraclass correlation coefficients (ICCs) for 3 surgeons (SYL, BCM, and SJM) with 10, 5, and 4 y of orthopedic experience, respectively. These 3 surgeons measured the CT images independently without knowledge of the other surgeons’ measurements. Four weeks after the measurements were taken by all 3 surgeons, 1 surgeon (BCM) repeated the measurements to assess intraobserver reliability. After establishing inter- and intraobserver reliability, the main measurements were performed.
Bone attenuation of the L1, L2, L3, L4, femoral head, femoral neck, greater trochanter, distal femur, proximal tibia, distal tibia, and talus was measured by placing a circular region of interest (ROI) on the central part of each bony region on a coronal CT image. Among a number of coronal images, the image in which the measurement took place was selected by using dynamic scout navigation to choose the central portion of each bony region in the sagittal plane (Fig. 1). A circular ROI with an area ranging from 100 to 120 mm2 was placed manually on the cancellous bone area, avoiding subchondral sclerotic bone and fracture lines. Mean bone attenuation of each desired region was measured using Hounsfield units (HU).
Measurement methods for each specific region with various CT studies were as follows: bone attenuation of the L1, L2, L3, and L4 was measured with L-spine CT and abdomen and pelvic CT. The coronal image was selected in which each measuring vertebral body was largest, meaning the central portion of the vertebra. This could be confirmed by using the dynamic navigation tool of the PACS software. Bone attenuation of the femoral head, femoral neck, and greater trochanter was measured with hip CT that included bilateral femurs. For the purpose of statistical independence, except for CT images showing a fracture or abnormal finding on the right side, only data from the right femur were included for statistical analysis [9]. Measurement of the femoral head, femoral neck, and greater trochanter, similar to the lumbar spine, involved placing the ROI in the center of each bony region on the coronal image in which the head appeared largest, meaning the central portion of the anatomic region. Bone attenuation of the distal femur and proximal tibia was measured with knee and tibia CT. The ROI on the metaphysis was placed as close as possible to the epiphyseal line for reliability. Bone attenuation of the distal tibia and talus was measured with tibia and ankle CT. Using dynamic navigation for a sagittal image of the ankle, the coronal line passing through the center of the articular surface of the distal tibia was identified and selected (Fig. 2). The circular ROI was placed on the center of the metaphysis, as close as possible to the epiphyseal line of the distal tibia and body of the talus.
Statistical analysis
In this study, reliability was assessed using ICCs and a 2-way random effect model, assuming a single measurement and absolute agreement [10, 11]. Using an ICC target value of 0.8, Bonett’s approximation was used in setting 0.2 as the width of 95 % confidence intervals. The minimal sample size was calculated to be 36 [12]. ICC values of >0.8 were considered as excellent reliability.
Partial correlation represents the correlation between CT variables and DEXA variables after common variance with other predictors has been removed from both sets of variables. Partial correlation measures the strength of a linear relationship between 2 variables while controlling for the effect of age.
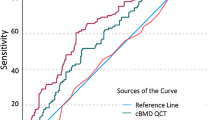
Receiver operating characteristic (ROC) curves were plotted as false-positive rate (i.e., 1 minus specificity) versus sensitivity for all cutoff values for bone attenuation on CT. The area under the ROC curve (AUC) was used to measure performance accuracy of bone attenuation on CT as a predictor of osteoporosis (T-score ≤ −2.5 as measured by DEXA [13]). An AUC of 1.0 represents error-free prediction of osteoporosis in all samples, whereas an AUC of 0.50 represents a 50 % likelihood of a correct prediction of osteoporosis, similar to a coin toss. This ROC curve was useful in finding the optimal cutoff point for correctly identifying osteoporosis or non-osteoporosis. HU thresholds that would yield high sensitivity (about 90 %) and specificity (about 90 %) also were analyzed [14].
Statistical analyses were conducted using R version 2.15.2 software (R Foundation for Statistical Computing, Vienna, Austria; ISBN 3-900051-07-0; http://www.r-project.org) using PPCOR and pROC packages. All statistics were 2-tailed and p values of <0.05 were considered significant.
Results
A total of 555 subjects met the inclusion criteria. After implementation of the exclusion criteria, 292 subjects were finally included in this study (Fig. 3). The mean age of the patients at the time of DEXA examination was 73.2 ± 11.5 y (range, 44.5–97.3 y). Most patients included in this study underwent CT due to trauma (Table 1).
In terms of reliability, all bone attenuation measurements, except the femoral neck in interobserver reliability, showed good to excellent reliability. Intraobserver reliability was highest for the L3 (ICC, 0.941) followed by the talus (ICC, 0.924). Interobserver reliability was highest for the L4 (ICC, 0.923) followed by the distal femur (ICC, 0.919). Intra- and interobserver reliability were lowest for the femoral neck (ICCs, 0.691 and 0.505, respectively) (Table 2). In terms of validity, bone attenuation of the lumbar spine (L3 and L4), femoral neck, and greater trochanter showed significant correlations with each area on DEXA examination (Table 3, Appendix I).
Bone attenuation of the peripheral skeleton on CT adequately reflected BMD of the central skeleton on DEXA. Bone attenuation of the distal tibia and talus on CT showed significant correlations with BMD of all parts on DEXA (correlation coefficients, 0.493–0.581 for the distal tibia, 0.396–0.579 for the talus). Bone attenuation of the femoral head on CT also showed a significant correlation with BMD of all parts on DEXA (correlation coefficients, 0.301–0.425). Bone attenuation of the distal femur and proximal tibia on CT showed significant correlations with BMD of only the femoral region on DEXA (correlation coefficients, 0.360–0.418 for the distal femur, 0.356–0.426 for the proximal tibia) (Table 4).
Cutoff values for bone attenuation on CT between osteoporosis and nonosteoporosis were significant for the L1 (136.15 HU), L2 (101.17 HU), L3 (105.49 HU), L4 (101.92 HU), femoral head (296.15 HU), femoral neck (3.79 HU), greater trochanter (24.74 HU), distal tibia (122.45 HU), and talus (311.37 HU) (Table 5). The ROC curves for these areas showed that bone attenuation on CT was useful in determining cutoff values (Fig. 4). On the contrary, cutoff values for bone attenuation of the distal femur and proximal tibia on CT were not significant between osteoporosis and nonosteoporosis. HU thresholds are shown in Table 5. Distal tibia CT attenuation threshold of 165.41 HU was approximately 90 % sensitive, while a threshold of 17.33 HU was 90 % specific. Talus CT attenuation threshold of 340.29 HU was approximately 90 % sensitive while a threshold of 233.75 HU was 90 % specific.
Discussion
Although previous studies have demonstrated the potential of CT as a screening tool for osteoporosis, the assessment correlation of BMD in those studies was limited to the spine. Therefore, we performed this study to evaluate the reliability and validity of CT as a screening tool for osteoporosis and to estimate the correlation of BMD between central and peripheral skeletons. To our knowledge, this is the first investigation to evaluate the correlation of BMD between lower extremity CT and DEXA. In the present study, bone attenuation on CT was found to be a reliable and valid method for assessing BMD and screening osteoporosis. In addition, peripheral bone attenuation on lower extremity CT correlated well with central BMD on DEXA.
Some limitations of this study should be addressed before discussing the findings in detail. First, this study was retrospective in nature and all subjects were patients who visited our hospital to evaluate a skeletal problem. Thus, there could be differences from the general population. Although we excluded all patients with any condition that could affect bone attenuation of each anatomic region, further research, such as a community-based study, is required. Second, there was a difference in slice thickness between central bone CT (pelvis and hip) and peripheral bone CT. However, we analyzed the “correlation” of bone attenuation between CT scans according to anatomic region. Thus, we believe the difference in examination condition had little influence on the results.
Since most DEXA examinations are performed to assess BMD in elderly patients, osteoporosis screening can overlook decreased BMD in younger patients. A screening tool in medicine should be easy to use and identify an unrecognized disease in all age groups. Therefore, we chose lower extremity CT, which is widely used in patients with various skeletal problems, as a screening tool. Although we focused on trabecular bone on CT, unlike DEXA, which assesses both cortical and trabecular bone, previous studies have shown that bone attenuation of the spine measured on CT was correlated with BMD of the hip and spine measured on DEXA [7, 8]. A previous study used quantitative CT with asynchronous calibration from CT colonography to screen osteoporosis [15]. This approach to CT calibration may provide for greatly expanded osteoporosis screening. However, we believe that screening tools should be easy to use. Therefore, we used conventional CT, which adds no cost and requires no additional equipment or software [14]. In addition, in this study, the age factor was controlled using partial correlation to apply our results in all ages, unlike in previous studies.
Intra- and interobserver reliability of measurements were lowest for the femoral neck. Although a previous study reported that structural changes were not observed in the proximal femur affected by osteoporosis [16], it has been generally accepted that there is a pattern of bone loss in the proximal femur [17]. We believe the value of bone attenuation of the femoral neck on CT was greatly influenced by the area of radiolucency and its heterogeneity. In addition, femoral neck measurement is challenging because the hip joint can rotate, and the degree of rotation differs by case and even by side of the femur. Therefore, examiners can encounter difficulty when selecting the coronal image of the central part of the femoral neck.
Few studies have compared bone attenuation on CT with BMD on DEXA in the same anatomic region. In terms of validity, the present study showed that CT is useful as a screening tool for osteoporosis. In addition, our results are significant considering that peripheral bone attenuation on CT also correlated with BMD on DEXA. Since it is well known that use of bisphosphonates to prevent low-trauma fracture is likely to be effective, BMD measurements are important in identifying patients at risk for fracture [18]. A previous study showed that ankle fracture had features of osteoporotic fracture [2]. In addition, fracture associated with low BMD can be site-specific with BMD of each anatomic region [19]. Although assessment of peripheral BMD has grown in importance, the World Health Organization’s criterion for osteoporosis diagnosis is not applicable to the peripheral skeleton [13]. In this study, bone attenuation of the spine, hip, and ankle on CT, except the distal femur and proximal tibia, had a positive predictive value for osteoporosis. The cutoff values on CT in those anatomic regions could help physicians predict the need for further evaluation.
Sensitivity is a true positive rate and specificity is a 1-false-positive rate of validity when BMD on DEXA reveals osteoporosis. Cutoff value is determined at the point of trade-off between highest sensitivity and specificity [20]. In addition to cutoff value, HU threshold values also were suggested in this study. CT attenuation threshold of 90 % sensitivity may be suitable for high-risk cohorts where the aim is to minimize false-negative results. Alternatively, CT attenuation threshold of 90 % specificity may be used as a reference value for lower-risk cohorts to minimize false-positive results [14].
CT is widely used in patients with various skeletal problems. Although several studies have reported a positive correlation between bone attenuation of the spine on CT and BMD on DEXA, there has been a lack of study regarding the reliability and validity of CT for assessing BMD. Based on our study, CT of the spine and lower extremity is a useful screening tool for osteoporosis. In addition, peripheral bone attenuation on lower extremity CT adequately reflects central BMD on DEXA. We believe that future research regarding the predictive value of bone attenuation on CT for high risk of osteoporotic fracture will be required.
References
Caliri A, De Filippis L, Bagnato GL, Bagnato GF (2007) Osteoporotic fractures: mortality and quality of life. Panminerva Med 49:21–27
Lee KM, Chung CY, Kwon SS, Won SH, Lee SY, Chung MK, Park MS (2013) Ankle fractures have features of an osteoporotic fracture. Osteoporosis International: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 24:2819–2825
Lee YK, Yoon BH, Koo KH (2013) Epidemiology of osteoporosis and osteoporotic fractures in South Korea. Endocrinol Metab 28:90–93
(2004) A public health approach to promote bone health. Bone health and osteoporosis: a report of the surgeon general. Rockville (MD)
Genant HK, Engelke K, Fuerst T et al (1996) Noninvasive assessment of bone mineral and structure: state of the art. J Bone Min Res : J Am Soc Bone Min Res 11:707–730
Lewiecki EM, Gordon CM, Baim S et al (2008) International Society for Clinical Densitometry 2007 Adult and Pediatric Official Positions. Bone 43:1115–1121
Pickhardt PJ, Lee LJ, del Rio AM, Lauder T, Bruce RJ, Summers RM, Pooler BD, Binkley N (2011) Simultaneous screening for osteoporosis at CT colonography: bone mineral density assessment using MDCT attenuation techniques compared with the DXA reference standard. J bone min res :J Am Soc Bone Min Res 26:2194–2203
Romme EA, Murchison JT, Phang KF, Jansen FH, Rutten EP, Wouters EF, Smeenk FW, Van Beek EJ, Macnee W (2012) Bone attenuation on routine chest CT correlates with bone mineral density on DXA in patients with COPD. J Bone Min Res : J Am Soc Bone Min Res 27:2338–2343
Park MS, Kim SJ, Chung CY, Choi IH, Lee SH, Lee KM (2010) Statistical consideration for bilateral cases in orthopaedic research. J bone joint surg Am vol 92:1732–1737
Lee KM, Lee J, Chung CY, Ahn S, Sung KH, Kim TW, Lee HJ, Park MS (2012) Pitfalls and important issues in testing reliability using intraclass correlation coefficients in orthopaedic research. Clinin ortho surg 4:149–155
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Bonett DG (2002) Sample size requirements for estimating intraclass correlations with desired precision. Stat Med 21:1331–1335
(1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organization technical report series 843:1–129
Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N (2013) Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med 158:588–595
Pickhardt P, Bodeen G, Brett A, Brown JK, Binkley N (2014) Comparison of femoral neck BMD evaluation obtained using lunar DXA and QCT with asynchronous calibration from CT colonography. Journal of Clinical Densitometry: the official journal of the International Society for Clinical Densitometry
Saitoh S, Nakatsuchi Y, Latta L, Milne E (1993) An absence of structural changes in the proximal femur with osteoporosis. Skelet Radiol 22:425–431
Kawashima T, Uhthoff HK (1991) Pattern of bone loss of the proximal femur: a radiologic, densitometric, and histomorphometric study. J ortho res : Pub Ortho Res Soc 9:634–640
Blake GM, Chinn DJ, Steel SA, Patel R, Panayiotou E, Thorpe J, Fordham JN, National Osteoporosis Society Bone Densitometry F (2005) A list of device-specific thresholds for the clinical interpretation of peripheral x-ray absorptiometry examinations. Osteoporosis International: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 16:2149–2156
Hongsdusit N, von Muhlen D, Barrett-Connor E (2006) A comparison between peripheral BMD and central BMD measurements in the prediction of spine fractures in men. Osteoporosis International: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 17:872–877
Zweig MH, Campbell G (1993) Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem 39:561–577
Conflicts of interest
None.
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this article.
This study was exempt from the approval of the institutional review board of our institution because it involved no human subjects.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent was not required.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix I
Scatter plot for correlations between bone attenuation on computed tomography and bone mineral density on dual-energy X-ray absorptiometry in the same anatomic region (GIF 68 kb)
High resolution image
(TIFF 3115 kb)
Rights and permissions
About this article
Cite this article
Lee, S.Y., Kwon, SS., Kim, H.S. et al. Reliability and validity of lower extremity computed tomography as a screening tool for osteoporosis. Osteoporos Int 26, 1387–1394 (2015). https://doi.org/10.1007/s00198-014-3013-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-3013-x