Abstract
Introduction and hypothesis
The primary objective was to compare high- and low-frequency pelvic floor muscle training (PFMT) with the impact on urinary incontinence episode frequency over 1 week (IEF/week). The secondary objective was to compare the two groups with regard to pelvic floor muscle function, morphometry, incontinence quality of life, and patient global impression.
Methods
This was a randomised parallel controlled study. The setting was regional gynaecological and urological outpatient clinics. The subjects consisted of a sample of 86 women with stress urinary incontinence (SUI). Group A underwent high-frequency PFMT and group B underwent low-frequency PFMT for 12 weeks. We recorded the IEF/week. The International Consultation on Incontinence Questionnaire Urinary Incontinence Short Form (ICIQ-UI SF) was used. Pelvic floor muscle function was evaluated using a perineometer. Pelvic floor muscle morphometry was evaluated with 3D/4D ultrasound. The Urinary Incontinence Quality of Life Scale (I-QoL) was used.
Results
Significant differences between group A and B after treatment (p<0.001) were noted in favour of group A in IEF/week (group A 10.2±7.0/2.3±3.0 vs group B 9.3±4.7/6.3±4.9), in the ICIQ-UI SF (group A 9.7±3.0/3.7 ± 3.6 vs group B 9.9±3.2/9.4±3.4). Significant differences between groups A and B after treatment were noted in favour of group A for pelvic floor muscle function in terms of maximal voluntary contraction and its duration, and also for pelvic floor muscle morphometry in terms of a reduction of the hiatal area during rest, contraction, and the Valsalva manoeuvre.
Conclusions
High-frequency PFMT for 12 weeks significantly decreased IEF/week in comparison with low-frequency PFMT. In the high-frequency exercise group, women had significantly better pelvic floor muscle function, morphometry and quality of life than the low-frequency exercise group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) is defined as a complaint of involuntary leakage of urine during physical activity or sports, sneezing or coughing due to increased intra-abdominal pressure [1,2,3,4]. Regardless of age, 15–30% of women are negatively affected by urinary incontinence in all areas of their lives (i.e. physical, mental and social), with a consequent deterioration in their quality of life [4].
According to the International Continence Society (ICS), pelvic floor muscle training (PFMT) is the first-line method for the treatment of SUI [2]. PFMT is a method based on scientific evidence, defined by the International Incontinence Society as repeated selective voluntary contraction and relaxation of specific pelvic floor muscles. It is important to train the strength and endurance of the pelvic floor muscles and to perform PFMT in the correct way [2, 3]. Based on scientific knowledge, it is recommended to perform stabilisation exercises with simultaneous activation of the pelvic floor muscles [5].
The dosage of pelvic floor exercises can be divided into mode of exercises, frequency, intensity, volume and duration of training. Mode of exercises are different positions during exercises. Frequency of exercises is number of training sessions per week. Intensity of strength training is defined as the percentage of the repetition maximum. The training volume is the number of repetitions performed in a specific time period. Periodisation is planned variation in the training volume and intensity by altering muscle actions–isometric, concentric and excentric. The American College of Sport Medicine recommends evaluating the efficacy of various intensities, frequencies and durations of exercise [3]. There are a limited number of studies that have evaluated the different frequencies of PFMT in women with stress urinary incontinence. Maintaining the frequency of the exercises is very important for its effect. High frequency is a major barrier to training adherence and compliance [6, 7].
Currently, there are a limited number of studies assessing the effect of PFMT with pelvic floor muscle morphometry using 3D/4D ultrasound [8, 9].
The 2D/3D ultrasound perineal approach is a non-invasive examination, but the probe is attached to the perineum. The standard midsagittal field of vision includes the symphysis pubis anteriorly, the urethra and bladder neck, the vagina, the cervix, the rectum and the anal canal. We can measure the bladder neck position, levator plate angle and anorectal angle. We can also measure the distance of the bladder neck from the symphysis and the distance between the symphysis and the anorectal angle. Translabial ultrasound may be used to quantify ureterovaginal prolapse during the Valsalva manoeuvre. The inferior margin of the symphysis pubis is used as a reference line [10,11,12].
The 3D/4D ultrasound perineal approach can show the levator hiatus area both at rest and in motion. It is examined at rest, at maximal voluntary contraction (MvC) and during the Valsalva manoeuvre. Subsequently, we can measure the anteroposterior dimension of the hiatus and the latero-lateral dimension of the hiatus in centimetres. We can measure muscle thickness and objectively record avulsions or muscle thinning. It is possible to objectively measure the activation of the hiatus muscles during coughing. We can also observe the hiatal area during pelvic floor muscle function examination. Volume contrast imaging software allows us to work with images of the hiatal area, even after the examination is finished [8, 9, 13, 14].
The primary objective was to compare high- and low-frequency PFMT with the impact on urinary incontinence episode frequency over 1 week (IEF/week). The secondary objective was to compare the two groups with regard to pelvic floor muscle function, morphometry, incontinence quality of life and patient global impression.
Materials and methods
The PELSTAB study was a randomised parallel controlled study with a 1:1 allocation that compared the effect of high-frequency PFMT in group A and low-frequency PFMT in group B in a population of women with SUI. It was conducted between May 2020 and January 2022 in Urogynaecology and Physiotherapy in Gynaecology and Urology, Clinic Centrum. The protocol was approved by the Ethics Committee of the self-governing region with the number 3545/2020/ODDZ-06621 on 28 February 2020.
Participants
Patients with urinary incontinence (UI) from regional gynaecological clinics were recommended for PFMT. The diagnosis of UI was made by a gynaecologist based on a standard examination [1]. Patients signed an informed consent form and were enrolled in the randomised, parallel, intervention study of an independent researcher. All patients had a medical history obtained through a structured interview to obtain urological and gynaecological data. The pelvic floor was then examined by an experienced physiotherapist who was blinded to the SUI condition.
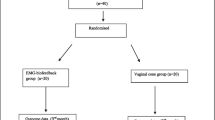
A total of 86 patients were enrolled in the study. Based on the inclusion and exclusion criteria, 71 patients were randomised 1:1 into groups A and B. The first patient serial numbers were assigned to the high-intensity exercise group A and the second patient serial numbers were assigned to low-intensity exercise group B. We used simple software randomisation according to the serial numbers of the patients. The generated numbers were placed in sealed envelopes. Each envelope contained a group A or B code. The final sample consisted of 71 women, with 35 women in group A and 36 women in group B. Investigators were blinded to which groups the patients were assigned to. Three women did not complete the study owing to low adherence (Fig. 1).
Sample size calculation
We used an estimate based on a sample of women based on a test power of 0.80 and an alpha of 0.05 (type I error). According to the sample selection, we expected a decreased incidence in SUI after PFMT from 25% to 10% according to incontinence episode frequencies per week. Success of the treatment was defined as a reduction of IEF of more than 50%. The estimated number of women in group A was 34, and the estimated number of women in group B was 34, for a total of 68. We expected a 20% loss, so we enrolled a total of 86 women.
Inclusion criteria
The inclusion criteria were as follows:
-
1.
Women willing to provide written informed consent
-
2.
Women over 18 years of age experiencing uncomplicated SUI
-
3.
Score on the International Consultation on Urinary Incontinence Questionnaire ≥6 points
-
4.
Symptoms of urinary incontinence for at least 3 consecutive months
-
5.
Degree of pelvic organ prolapse, stage ≤ 2
-
6.
Willingness to accept the randomisation process and fully participate in tests
Exclusion criteria
Exclusion criteria were as follows:
-
1.
History of anti-incontinence surgery in the past 12 months
-
2.
History of pelvic prolapse repair or urethral surgery in the past 12 months
-
3.
History of PFMT in the past 12 months
-
4.
History of interstitial cystitis or bladder-related pain
-
5.
Chronic severe constipation
-
6.
Clinically significant renal or hepatic impairment
-
7.
Clinically significant heart impairment
-
8.
Pregnant, lactating or actively trying to become pregnant
-
9.
Presence of urinary tract infection
-
10.
Use of rehabilitation aids (pessary, urethral plugs, vaginal beads etc.)
-
11.
Not able to perform pelvic floor exercises and/or omitting exercises
-
12.
Incomplete questionnaire
-
13.
Refusal to participate in the study
-
14.
Urinary incontinence medication
Stress urinary incontinence was confirmed by a positive score on the International Consultation on Incontinence Questionnaire Urinary Incontinence Short Form (ICIQ-UI SF) and a negative symptom score on the Overactive Bladder Questionnaire Symptom Score (OAB-q SS).
Interventions
Both groups
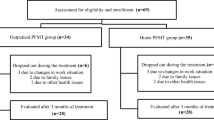
Figure 2 shows a detailed description of the exercises.
-
1.
Educational instruction with a model of the pelvis of the women and on the anatomy, physiology and function of the pelvic floor muscles; the exercises were explained.
-
2.
Mode of exercises are different positions during exercises: training of the pelvic floor muscles in various positions, such as lying on the back, abdomen, side, kneeling, sitting, standing and walking.
-
3.
Training of the pelvic floor muscles with static and dynamic stabilisation. Respiratory stereotype correction, exercises to activate the diaphragm and training of the transverse abdominis muscles, multifidus muscles and other deep muscles of the spine and upper and lower limbs with simultaneous activation of the PFMs. The PFMs were contracted during exhalation. Patients held the stabilisation exercises during exhalation (Fig. 2) [5].
Group A
Frequency of exercises: high-frequency exercise group, i.e. 12 weeks, five times a week for 30 min a day, with five sessions of training with a physiotherapist, followed by continuation in the home environment [3]. The number of PFM contractions per week was 900. This means that the number of contractions was 5 times greater than in group B.
Group B
Frequency of exercises: low-frequency exercise group, i.e. 12 weeks, twice a week for 15 min a day, with five sessions of training with a physiotherapist, followed by continuation in the home environment [3]. The number of PFM contractions per week was 180. During the 15-min training unit, group B did half the number of stabilisation exercises and contractions of PFMs compared with group A.
Description of sessions with a physiotherapist
-
First session with physiotherapist—comprehensive kinesiological examination of posture and the pelvis, examination of breathing patterns, examination of pelvic floor muscles with ultrasound, perineometer, vaginal palpation and education regarding proper exercise.
-
Second session—explanation of the principle of exercise lying on the back, on the abdomen, on the side and kneeling.
-
Third session—explanation of the principle of exercise when sitting, standing and walking and during changes of positions.
-
Fourth session—correction of breathing patterns (rhythm, speed, length of exhalation and other aspects and stereotypes) when lying on the back and when sitting—diaphragmatic breathing and activation of the musculus transversus abdominis.
-
Fifth session—practicing stabilisation exercises—stabilisation during the bridge, diagonal stabilisation, stabilisation in the push-up, stabilisation during squats and stabilisation during side bridges. With the accompanying strength and endurance activation of the pelvic floor muscles during exhalation.
Patients had a notebook where they kept a detailed record of the frequency of exercises.
Measurements
All measurements were taken before treatment and after 12 weeks of treatment.
Stress urinary incontinence was confirmed by a positive score on the ICIQ-UI SF and a negative symptom score on the Overactive Bladder Questionnaire Symptom Score (OAB-q SS). Both overactive bladder and urge urinary incontinence were excluded by the OAB-q.
SUI evaluation questionnaire
The ICIQ-UI SF was developed by the ICS. The first two questions monitor the frequency and quantity of leaked urine and the third question considers how urine loss affects daily life. The ICIQ-UI SF score is the sum of the score of all questions (0 = no leak; 1–5 = slight; 6–12 = moderate; 13–18 = severe; and 19–21 = very serious). The Cronbach’s alpha reliability for this questionnaire is 0.95 [15, 16].
OAB evaluation questionnaire
The Overactive Bladder Questionnaire Symptom Score (OAB-q SS) on the symptoms of an overactive bladder in the past 4 weeks. It contains six questions on symptoms, giving a symptom score (0, without symptoms; 100, most symptoms). The Cronbach’s alpha of this questionnaire is 0.90 [17, 18].
Primary measurements
The primary objective of our study was to evaluate change in urinary incontinence episode frequency over 1 week in the two groups.
Secondary measurements
The secondary objective was to compare the two groups with regard to pelvic floor muscle function, morphometry, incontinence quality of life and patient global impression.
Pelvic floor muscle function
Pelvic floor examination by perineometer
Perineometric pressure during a maximum voluntary contraction (MvC, cmH2O), MvC endurance in seconds, and pelvic floor muscle relaxation in units of water column height (cmH2O) were measured. An 11-cm pressure probe was used, covered by a latex condom to which a lubricant was applied. Examination was carried out with an empty bladder in the lithotomy position. Each manoeuvre was performed twice. The probe was inserted vaginally. Up to 10 cmH2O there was a slight contraction, 10–30 cmH2O a moderate contraction and 40–60 cmH2O a strong contraction. It is important to set the resting tone correctly after saturation introduction to 100 cmH2O [19].
The PERFECT scheme: P – Power. A five-point scale was used (0, no contraction; 1, weak contraction; 2, normal contraction; 3, strong contraction; and 4, very strong contraction). E – Endurance. The patient was asked to perform an MvC of the pelvic floor, and the contraction-weakening time was measured. Time was given in seconds, for a maximum of 10 s. R – Repetitions of contractions. The patient was requested to perform repeated MvCs for 3 s. The number of contractions to fatigue or a decrease in quality (up to 10 contractions) was recorded. F – Fast contractions. The patient was requested to perform rapidly repeated MvCs lasting a maximum of 1 s each. The number of contractions to fatigue or quality decline (up to ten contractions) was recorded. We examined this scheme using vaginal palpation and a perineometer (Peritron, Laborie, Mississauga, ON, Canada) [20].
Pelvic floor muscle morphometry with 3D/4D transperineal ultrasound
We used a Voluson-i BT11 ultrasound console, volume contrast imaging (VCI) software (GE Healthcare Austria, Zipf, Austria) and a RAB4-8-RS 3D/4D 4–8 MHz probe in the midsagittal plane. Examination took place with an empty bladder in the lithotomy position. The probe was placed longitudinally on the perineum. 3D/4D images of the hiatal area were taken at rest, at MvC and during the Valsalva manoeuvre (in centimetres squared). Subsequently, we measured the anteroposterior dimension of the hiatus and the latero-lateral dimension of the hiatus (in centimetres). Each manoeuvre was performed twice. This method has been tested for reliability and shown to be very good [10,11,12]. The examinations were performed by a trained urogynaecologist and physiotherapist (Fig. 3).
Pelvic floor muscle morphometry measures muscle tone and thickness and provides an objective measurement of avulsions. It is possible to measure the activation of the hiatus muscles during coughing. We can also examine the hiatal area during the PFM function examination. VCI software allows us to work with images of the hiatal area, even after the examination is finished. Translabial ultrasound may be used to quantify ureterovaginal prolapse during the Valsalva manoeuvre.
Pelvic floor muscle morphometry is a unique way for physiotherapists to visualise the PFMs after PFMT in women with SUI. In future research, three-dimensional tomographic ultrasound imaging software and vaginal pressure profiles may be used in order to measure the effect of different types of PFMT.
Incontinence-related quality of life
Urinary Incontinence Quality of Life scale
The Incontinence Quality of Life (I-QoL) scale is composed of three subscales (avoidance and limiting behaviour, psychosocial impact and social embarrassment) and comprises 22 questions, with a total score within the range 0 (worst quality of life) to 100 (best quality of life). The Cronbach’s alpha reliability of the I-QoL is 0.91–0.96 [21].
Patient Global Impression of Improvement scale
The Patient Global Impression of Improvement (PGI-I) scale evaluates the status of urination problems compared with the patient’s condition before treatment. Patient impressions are evaluated according to the following scores: 1, much better; 2, moderately better; 3, a little better; 4, no change; 5, a little worse; 6, a lot worse; and 7, definitely worse [22].
All measurements were taken before treatment and after 12 weeks of treatment.
Statistical analysis
Descriptive and analytical statistics were used for data analysis. An unpaired t test was used to compare the experimental and control groups before training. Differences between the control and experimental groups pre- and post-intervention were assessed using a generalised linear model and repeated-measures mixed-design analysis of variance (ANOVA; significance level, t<0.05); partial eta-squared (η2) effect sizes were calculated. According to Cohen’s specification for ANOVA analysis, effect sizes were classified as follows: η2=0.00–0.003, no effect size; η2=0.010–0.039, small effect size; η2=0.060–0.110, medium effect size; and η2=0.140–0.200, large effect size. We used an intention-to-treat analysis. The calculations were performed in IBM SPSS Statistics for Macintosh, Version 28.0 (IBM, Armonk, NY, USA).
Results
The final sample consisted of 71 women, with 35 women in group A and 36 women in group B. The cohort consisted of women with SUI, with an average age of 41.7 years in group A and 39.1 years in group B. No significant differences were observed in demographics between the two groups in terms of age, education, menstrual cycle, BMI, duration of difficulties with SUI, average number and type of childbirth, foetal weight, number of incontinence episodes per week, average number of sanitary pads used per day, ICIQ-UI SF score or OAB-q SS. PFM prolapse was not present. None of the women had undergone anti-incontinent or prolapse surgery (Table 1).
All measurements were taken before treatment and after 12 weeks of treatment.
No significant differences between groups A and B were observed in the pre-treatment parameters. After treatment, significant differences between groups A and B were noted in favour of group A (p<0.001) in the number of incontinence episodes per week. In group A, there was a reduction in IEF by 7.9 per week and in group B there was a reduction in IEF by 2.9 per week. In group A, there was a reduction in ICIQ-UI SF score of 6.0 points and in group B there was a reduction of 0.5 points (Table 2).
After treatment, significant differences (p<0.001) between groups A and B were noted in favour of group A in pelvic floor muscle function assessed by perineometer, in terms of MvC (in cmH2O) and its duration in seconds, as well as by the parameters of the PERFECT scheme (power of MvC, endurance of MvC, number of repetitions of MvCs for 3 s, number of fast MvCs for 1 s assessed by perineometer; Table 3).
After treatment, significant differences (p<0.001) between groups A and B in favour of group A were also recorded by pelvic floor muscle morphometry assessed using 3D/4D ultrasound, i.e. a reduction in the levator hiatus area during rest, contraction and the Valsalva manoeuvre (in centimetres squared), and a reduction in the levator hiatus (antero-posterior, AP) and (left-right, LR) diameters in centimetres (Table 4). The hiatus size was 16–18 cm2 at rest and 18–21 cm2 during the Valsalva manoeuvre.
After treatment, significant differences between group A and B were noted in favour of group A (p<0.001) in the PGI-I subjective improvement scale, quality of life assessed by the I-QoL total score, avoidance and limiting behaviour score, psychosocial impact score and social embarrassment score (p<0.001). The PGI-I scale of subjective improvement indicated that group A felt that their condition was “much better”, and group B felt “a little better” (Table 5).
Discussion
A regimen of daily PFM exercises along with stabilisation is more likely to significantly reduce IEF/week than twice-weekly exercises. After treatment, significant differences were noted in favour of high-frequency PFMT (group A) regarding the number of incontinence episodes per week and the symptoms of SUI.
A regimen of daily PFM exercises along with stabilisation was more likely to significantly improve PFM function and morphometry than twice-weekly exercises. Significant differences were noted in favour of group A regarding pelvic floor muscle function assessed using a perineometer in terms of MvC and its duration, endurance and fast contractions. Significant differences in favour of group A were also recorded in PFM morphometry by 3D/4D ultrasound regarding a reduction in the levator hiatus area during rest, contraction and the Valsalva manoeuvre, and a reduction in the levator hiatus antero-posterior and latero-lateral diameters. If the condition of the patient improves after high-intensity PFMT, they may subsequently be able to reduce the exercise dose and continue with low-intensity PFMT for a long time.
The stated results confirmed that the mentioned improvements also had a positive impact on the quality of life and subjective improvement.
Bø et al. [24] examined the correlation between vaginal resting pressure, pelvic floor muscle strength, endurance and levator hiatus area in 300 pregnant nulliparas. Strong pelvic floor muscle contraction correlated slightly with lower levator hiatus area. Increased resting tone correlated with decreased levator hiatus area. After high-frequency PFMT in group A, a significant reduction in levator hiatus area during rest, contraction and the Valsalva manoeuvre was noted.
Albrich et al. [25] assessed the correlation between 2D/3D ultrasound examination and pelvic floor muscle contractility in 114 women. Here, positive correlations were found between bladder neck elongation and reduction of the symphysis–levator distance, and reduction of the levator hiatus area and palpable vaginal examination of muscle strength. Our diagnostic procedure included vaginal palpation, palpation of the muscles in three layers to detect painful points and diagnose avulsions (neither of which was present), and the Valsalva manoeuvre to detect prolapses.
Cacciari et al. [8] evaluated PFM morphometry and function after 12 weeks of PFMT in 362 elderly women with urinary incontinence. The women trained 5 times a week, followed by 3 times a week for 9 months. Immediately after 12 weeks, significant improvements in pelvic floor muscle morphometry were observed when coughing and during contraction. These improvements persisted after a year of exercise.
Strengths and limitations
The strengths of the study are the objective measurement of the PFM function using a perineometer and utilisation of pelvic floor muscle morphometry by 3D/4D ultrasound, and the use of standardised measuring tools, including ICIQ-UI SF. A limitation is the impossibility of using other measurement devices, such as a dynamometer or vaginal pressure profile. These tools are still in development and in preparation for use in clinical practice. It is unknown whether these changes persist in the long term.
Another limitation is that this was not a multicentre study.
Conclusions
High-frequency PFMT with stabilisation for 12 weeks significantly decreases IEF/week in comparison with low-frequency PFMT.
In the high-frequency exercise group, women had significantly better PFM function and morphometry and life quality compared with the low-frequency exercise group.
Pelvic floor muscle morphometry by 3D/4D transperineal ultrasound is a unique way of visualising PFM function.
References
Abrams P, Andersson KE, Apostolidis A, et al. 6th International Consultation on Incontinence. Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Neurourol Urodyn. 2018;37(7):2271–2.
Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Neurourol Urodyn. 2017;36(2):221–44.
Bo K, Berghmans B, Morkved S, Van Kampen M. Evidence–based physical therapy for the pelvic floor, 2nd Edition. London: Churchill Livingstone, 2015. p. 446.
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
Kim EY, Kim SY, Oh DW. Pelvic floor muscle exercises utilizing trunk stabilization for treating postpartum urinary incontinence: randomized controlled pilot trial of supervised versus unsupervised training. Clin Rehabil. 2012;26(2):132–41.
Szumilewicz A, Dornowski M, Piernicka M, et al. High-low impact exercise program including pelvic floor muscle exercises improves pelvic floor muscle function in healthy pregnant women—a randomized control trial. Front Physiol. 2019;9:1867.
Szumilewicz A, Kuchta A, Kranich M, Dornowski M, Jastrzębski Z. Prenatal high-low impact exercise program supported by pelvic floor muscle education and training decreases the life impact of postnatal urinary incontinence: a quasiexperimental trial. Medicine (Baltimore). 2020;99(6):e18874.
Cacciari LP, Morin M, Mayrand MH, Tousignant M, Abrahamowicz M, Dumoulin C. Pelvic floor morphometrical and functional changes immediately after pelvic floor muscle training and at 1-year follow-up, in older incontinent women. Neurourol Urodyn. 2021;40(1):245–55.
Cyr MP, Dumoulin C, Bessette P, et al. Characterizing pelvic floor muscle function and morphometry in survivors of gynecological cancer who have dyspareunia: a comparative cross-sectional study. Phys Ther. 2021;101(4):pzab042.
Dietz HP, Shek C, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by 3D pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25:580–5.
Dietz HP, Wong V, Shek KL. Simplified method for determining hiatal biometry. Aust NZ J Obstet Gynecol. 2011;51:540–3.
Dietz HP. Ultrasound imaging of the pelvic floor. I. Two-dimensional aspects. Ultrasound Obstet Gynecol. 2004;23:80–92.
Cyr MP, Kruger J, Wong V, Dumoulin C, Girard I, Morin M. Pelvic floor morphometry and function in women with and without puborectalis avulsion in the early postpartum period. Am J Obstet Gynecol. 2017;216(3):274.e1–8.
Fontaine F, Dumoulin C, Bergeron S, et al. Pelvic floor muscle morphometry and function in women with primary and secondary provoked vestibulodynia. J Sex Med. 2018;15(8):1149–57.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23:322–30.
Klovning A, Avery K, Sandvik H, Hunskaar S. Comparison of two questionnaires for assessing the severity of urinary incontinence: the ICIQ-UI SF versus the incontinence severity index. Neurourol Urodyn. 2009;28(5):411–5.
Coyne K, Revicki D, Hunt T, et al. Psychometric validation of an overactive bladder symptom and health-related quality of life questionnaire: the OAB-q. Qual Life Res. 2002;11(6):563–74.
Coyne KS, Payne C, Bhattacharyya SK, Revicki DA, Thompson C, Corey R, et al. The impact of urinary urgency and frequency on health related quality of life in overactive bladder: results from a national community survey. Value Health. 2004;7:455–63.
Rahmani N, Mohseni-Bandpei MA. Application of perineometer in the assessment of pelvic floor muscle strength and endurance: a reliability study. J Bodyw Mov Ther. 2011;15:209–14.
Laycock J, Jerwood D. Pelvic floor assessment: the P.E.R.F.E.C.T. scheme. Physiotherapy. 2001;87(1):631.
Bushnell DM, Martin ML, Summers KH, Svihra J, Lionis C, Patrick DL. Quality of life of women with urinary incontinence: cross-cultural performance of 15 language versions of the I-QOL. Qual Life Res. 2005;14:1901–13.
Yalcin I, Bump RC. Validation of two global impression questionnaires for incontinence. Am J Obstet Gynecol. 2003;189(1):98–101.
Cohen J. Statistical power analysis for the behavioural sciences. Hillsdale: Lawrence Erlbaum Associates. 1998
Bø K, Hilde G, Tennfjord MK, Stær-Jensen J, Siafarikas F, Ellstrøm EM. Pelvic floor muscle variables and levator hiatus dimensions: a 3/4D transperineal ultrasound cross-sectional study on 300 nulliparous pregnant women. Int Urogynecol J. 2014;25:1357–61.
Albrich S, Steetskamp J, Knoechel SL, Porta S, Hoffmann G, Skala C. Assessment of pelvic floor muscle contractility: digital palpation versus 2D and 3D perineal ultrasound. Arch Gynecol Obstet. 2016;293:4.
Acknowledgements
The authors are grateful to all patients who participated in this study.
Author information
Authors and Affiliations
Contributions
P.U. is responsible for the provision and selection of suitable probands; J.S. and M.H. are responsible for study design and methodology; M.H. is responsible for data collection and intervention; E.V. is responsible for preparing educational materials for exercise; P.U., J.S. and M.H. have access to the final trial dataset. M.H. paid for English corrections. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The protocol was approved by the Ethics Committee of the self-governing region with the number 3545/2020/ODDZ-06621 on 28 February 2020.
All participants gave written informed consent before data collection began.
Conflicts of interest
The authors have no conflicts of interest to declare.
Source(s) of support: VEGA 1/0540/21
Correlation of a combination of biochemical and clinical markers in the diagnosis and prognosis of the clinical outcome of cancer.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Registration: NCT04340323
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hagovská, M., Švihra, J., Urdzík, P. et al. A randomised interventional parallel study to evaluate the effect of different frequencies of pelvic floor muscle exercises with core stabilisation using three-dimensional ultrasound: the PELSTAB study. Int Urogynecol J 34, 2049–2060 (2023). https://doi.org/10.1007/s00192-023-05473-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05473-w