Abstract
Introduction and hypothesis
Pelvic organ prolapse (POP) is a benign condition that can adversely affect women’s quality of life. Minimally invasive mesh sacrocolpopexy is an effective surgical treatment for POP. This study aims to assess the perioperative, postoperative, and long term (10 years) outcome of a single institution cohort undergoing minimally invasive sacrocolpopexy.
Methods
This retrospective study included all cases of laparoscopic sacrocolpopexy performed between 2003 and 2016. Patients were contacted by phone in 2022 for long term follow-up. Data on operative time, length of hospital stay, conversion rate, perioperative injuries, early and late postoperative complications and subjective success rates were collected.
Results
Ninety-five patients were included aged 60±12 years. Most patients (72%) presented grade 3 POP. Grade of prolapse (3±0.4 vs 3±0.5, p<0.01) and hospital stay (3±1.1 vs 3.1±1.7; p<0.01) were significantly higher in patients who developed early postoperative complications (1st year). At long term follow-up (12±3 years), 48 patients responded. Nine subjects (19%) presented a subjective recurrence with bulge symptoms. Surgery satisfaction was of 79%. The most frequent de novo reported symptom was urge urinary incontinence followed by stress urinary incontinence. Three cases (3%) of mesh erosion were described, all occurred after the 5th postoperative year.
Conclusions
Laparoscopic mesh sacrocolpopexy is a safe surgical technique that shows satisfying and consistent long-term results despite the occasional onset of new urinary symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP), defined as pressure or bulging sensation in the vaginal area is an increasingly frequent concern. This condition was shown to rise with age, obesity, and increasing parity, as those constitute the principal risk factors of pelvic floor dysfunction [1]. The treatment of POP is usually driven by patient demand. When conservative treatment fail (pelvic floor muscle training and pessary use), surgical treatment is offered either via an abdominal or vaginal route, with or without the use of mesh. Abdominal sacrocolpopexy is a technique that involves the placement of a synthetic mesh from the apex of the vagina to the anterior longitudinal ligament of the sacrum.
With the current rise of minimally invasive approaches, laparoscopic/robotic abdominal sacrocolpopexy is gaining popularity as the standard of care for pelvic organ prolapse. However, concern remain about the complexity of this approach in previously operated patients, in obese patients, in old patients and in patients with severe prolapse [2]. Moreover, data examining long-term complications of laparoscopic mesh sacrocolpopexy are lacking, and delayed side effects are seldom reported (longest reported follow up is 4 years [3]).
In this study, we analyze the perioperative (related to the surgery), early postoperative (1 year), and long term (10 years) outcome of a single institution cohort undergoing minimally invasive sacrocolpopexy.
Methods
Ethic’s board approval was obtained for this retrospective study. All patients undergoing minimally invasive (laparoscopic) mesh sacrocolpopexy (LMS) between 2003 and 2016 were included and contacted by phone in June 2022 for subjective long-term follow-up. The phone call was conducted by the same independent researcher and consisted of the same set of questions related to the presence of symptoms, and satisfaction related to the surgery. At time of surgery, all subjects had signed an informed consent form.
Pre-operatively, all patients underwent a thorough clinical examination. Tension free vaginal tape (TVTO) was simultaneously inserted only in patients complaining of urinary incontinence (SUI) objectified clinically (full bladder cough test after prolapse reduction), or on urodynamic assessment. Therefore, 24% (23 subjects) of patients benefited from simultaneous TVTO insertion.
The same standardized surgical technique was performed alternatively by two different surgeons experienced in urogynecological surgery: an anterior-posterior double arm laparoscopic sacrocolpopexy/hysteropexy using a polypropylene monofilament mesh. The anterior and posterior vaginal walls were fixed to the anterior longitudinal sacral ligament, after creating a retroperitoneal tunnel where the mesh is layed. Peritoneal windows were closed after pulling up the uterus to its normal anatomical position. No additional surgery was performed through the vaginal route other than TVTO when concomitant SUI was present.
All patients received antibiotic prophylaxis and were prescribed low molecular weight heparin for at least three post operative weeks.
The following data was collected:
-
Demographic data and risk factors for prolapse: age, number of normal deliveries, body mass index (BMI) in Kg/m2
-
Operative data: operative time (minutes), length of hospital stay (days), conversion rate, simultaneously performed procedures (adhesiolysis, hysterectomy and TVTO) and peri-operative incidents (urinary/digestive tract or blood vessel injuries).
Short term outcomes
Patients were followed up during the first year systematically at 5 weeks and 6 months, and at any other time if there was a specific complain. Early postoperative complications (at one year) were recorded and combined as a composite outcome: voiding difficulties, delayed mobility, wound complications, febrile morbidity, postoperative ileus, thromboembolic phenomena, mesh erosion, constipation, dyspareunia.
Long term outcomes
All patients were contacted by phone in June 2022 for a subjective long term follow up assessment. An independent medical doctor researcher with sufficient urogynecology knowledge called systematically all patients. The same set of questions was asked for all patients and a discussion was performed if deemed necessary to more clarify the symptoms or complains.
They were asked about the onset of new symptoms preoperatively absent, or recurring post-operatively. The new onset of bulge symptoms at any time follow up was considered a subjective recurrence. The onset of other symptoms: SUI, urge urinary incontinence (UUI), constipation, dyspareunia (if sexually active), were compared between patients considered to have a recurrence and those who did not.
Global satisfaction from the surgery was assessed with a rate going from 0 (not satisfied at all) to 100% (fully satisfied).
Statistical analysis
-
Postoperative complications were recorded in the early postoperative stage up to the first operative year. All analyzed parameters were compared between patients who presented complications and those who did not, using Mann-Whitney test for quantitative non-parametric variables and khi-2 test for qualitative variables. Analyzed parameters were: BMI, age at time of surgery, prolapse grade, number of compartments, operative time and hospital stay duration.
-
At long term follow up, patients were considered to have a subjective recurrence if complaining of new onset of bulge symptoms. Several parameters (SUI, UUI, constipation, sexual activity, dyspareunia) were compared between this recurrent group and those who did not complain of a subjective recurrence, using Mann-Whitney test for quantitative data and khi-2 test for qualitative data.
Results
Demographic and operative data is reported in Table 1. Most patients (72%) presented grade 3 POP, 5% grade 2 and 23% grade 4.
Short term outcomes (Table 2)
Ninety-five patients were included in this group. No hysterectomies were performed at time of LMS, and no cases of conversion were encountered. Blood loss was estimated at less than 200 mL in all cases, and transfusion was not required in any of the patients.
Several parameters were compared between patients who developed complications in the first year and those who did not. Grade of prolapse (3±0.4 vs 3±0.5, p<0.01) and hospital stay (3±1.1 vs 3.1±1.7; p<0.01) were significantly higher in patients with complications. BMI (26±4 vs 26±3; p=0.9), age at time of surgery (60±6 vs 60±12; p=0.6) and operative time (156±40 vs 160±30; p=0.9) did not differ. No difference was found between the rate of complications and the insertion of TVTO (p=0.8), adhesiolysis (p=0.3) and the use of only one mesh (p=0.6).
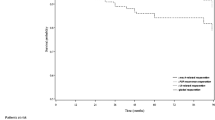
Long term outcomes
Forty-eight patients were included in this group (50% of the initial group). Of the remaining 50%: 33% of patients were lost to FU and 17% were deceased or medically ill (Table 3). Mean time of long follow up was 12±3 years ranging from 7 to 18 years. Mean age at time of follow up was 72±12 years ranging from 42 to 97 years. Most frequent symptoms, of post operative onset, reported at long follow up were: UUI (31%), followed by constipation (21%), then SUI (19%) (Table 3). Amongst sexually active subjects, only 4% complained of dyspareunia at long term follow-up. Surgery satisfaction was of 79±24%. 19% of patients complained of bulge symptoms and were considered to have a subjective recurrence. Bulge symptoms were reported mainly during efforts, and were always more bearable than the preoperative prolapse. Comparison of symptoms between recurrent and non-recurrent patients are reported in Table 4. Recurrent patients were significantly less satisfied than those who did not have a recurrence (61±25 vs 85±17 %, p<0.01). Other parameters did not differ: BMI (26±2 vs 26±4 kg/m2; p=0.5), age at time of surgery (56±14 vs 59±10 years; p=0.6), operative time (168±28 vs 154±33 minutes; p=0.2), length of hospital stay (3.2±0.8 vs 2.8±0.8 days; p=0.1), actual age (67±12 vs 70±10 years; p=0.6) and FU length (11±2 vs 10±3 years; p=0.4).
Patients with subjective recurrence were more likely to present with de novo SUI (p=0.03). It was not the case for UUI (p=0.4), constipation (p=0.3), sexual activity (p=0.8) and dyspareunia (p=0.4).
Symptomatic mesh erosion was diagnosed in three patients at 5, 6 and 10 years postoperatively. All erosions were located at the level of the vagina and cystoscopy did not detect vesical erosion. These patients were excluded from the long term follow up group.
Discussion
Patient’s subjective experience of their pelvic organ prolapse is the main driver to seek treatment. Surgery is indicated when conservative treatments have failed [4]. Therefore, subjective assessment of patient satisfaction is paramount to assess the success of the surgery, especially that anatomical treatment is not necessarily associated with patient relief [3].
In this study, we report the first long term follow-up analysis in the literature, for subjects who had undergone laparoscopic sacrocolpopexy.
Short term outcomes
The two major obstacles to laparoscopic surgery, particularly sacrocolpopexy, were increased weight and age, as these populations were thought to complicate more easily [5]. Our subjects had a mean BMI of 26 and a mean age of 60 at time of surgery. Increased age and BMI did not seem to affect postoperative complications, symptoms, or outcomes.
SUI must be diagnosed prior to POP surgery since correction of the prolapse could unmask stress urinary symptoms [6]. It is recommended to treat both conditions simultaneously when SUI is present. According to the European Association of Urology (EAU) guidelines, preoperative testing detects 30% of SUI in women with POP [7]; in our study 24% had preoperative SUI and benefited from TVTO insertion.
Operative incidents were rare in this series, however, first year complications were reported in 11% mostly related to de novo SUI requiring surgical correction. This was associated with higher prolapse grade, while BMI and age were not. In fact, in the PROSPERE randomized control trial it was shown that LMS causes even less complications than vaginal approaches with similar functional correction [8, 9].
Long term outcomes
Mesh erosions were diagnosed at long term follow up. It is an interesting finding because all were symptomatically diagnosed after 5 years while previous studies report earlier erosions (latest at the 5th postoperative year) [10, 11]. In our cohort all erosions were located in the vagina and successfully repaired with local excision and suturing by a vaginal approach. This is a relatively low rate as the ACOG states that sacrocolpopexy with mesh is associated with 10% of long term (7 years) mesh related complications (erosions, osteitis) most of which require reoperation [12].
At long term follow up, the most frequently reported de novo symptom was UUI followed by SUI. This new onset of urge urinary incontinence could be related to local inflammatory factors related to late mesh retraction or to other factors related to women’s aging and comorbidities [13].
Dyspareunia was reported in only 2 patients of the sexually active subset and is probably related to local dryness following menopause and increased age. Abdominal mesh surgeries are known to cause less dyspareunia than vaginal approaches and this remains true at long follow-up [14].
Nineteen percent of responders complained a subjective recurrence with bulge symptoms. None of the patient required or demanded a redo-surgery since this recurrence was always less bothersome than pre operative prolapse. The only symptom associated with the presence of a recurrence was SUI.
There are some limitations to this study, mainly the small population and the low percentage of responders at long time follow up (50%). Other long-term studies could help in giving more power to the results obtained with this cohort, and better understand the long-term postoperative evolution of operated POP women with mesh.
Conclusion
This is the first study to report long-term follow-up of patients undergoing laparoscopic mesh sacrocolpopexy. Satisfaction rate remains high after 10 years with a low recurrence rate. The most frequently reported urinary symptom of new onset was UUI, while SUI is associated with recurrence of bulge symptoms. Concerning mesh erosion, it must be kept in mind that it can happen as late as 10 years post operatively.
Laparoscopic sarcocolpopexy remains one of the best minimally invasive techniques for surgical treatment of urogenital organ prolapse. It can be offered to young symptomatic patients since the amelioration persists on long follow-up.
Abbreviations
- BMI:
-
body mass index
- LMS:
-
laparoscopic mesh sacrocolpopexy.
- POP:
-
pelvic organ prolapse.
- SUI:
-
stress urinary incontinence.
- TVTO:
-
tension free vaginal tape.
- UUI:
-
urge urinary incontinence.
References
Vergeldt TFM, Weemhoff M, IntHout J, Kluivers KB. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J. 2015;26:1559–73.
Padoa A, Shiber Y, Fligelman T, Tomashev R, Tsviban A, Smorgick N. Advanced Cystocele is a Risk Factor for Surgical Failure after Robotic-assisted Laparoscopic Sacrocolpopexy. J Minim Invasive Gynecol. 2022;29:409–15.
Bojahr B, Tchartchian G, Waldschmidt M, Ohlinger R, De Wilde RL. Laparoscopic Sacropexy: A Retrospective Analysis of the Subjective Outcome in 310 Cases. Obstet Gynecol Int. 2012;2012:1–6.
Pelvic Organ Prolapse: ACOG Practice Bulletin, Number 214. Obstet Gynecol. 2019 134:e126–e142
Boudy AS, Thubert T, Vinchant M, Hermieu JF, Villefranque V, Deffieux X. Outcomes of laparoscopic sacropexy in women over 70: A comparative study. Eur J Obstet Gynecol Reprod Biol. 2016;207:178–83.
Chen A, McIntyre B, De EJB. Management of Postoperative Lower Urinary Tract Symptoms (LUTS) After Pelvic Organ Prolapse (POP) Repair. Curr Urol Rep. 2018;19:74.
Harding CK, Lapitan MC, Arlandis S, et al. EAU Guidelines on non-neurogenic Female LUTS. 2022.
Lucot J, Cosson M, Verdun S, et al. Long-term outcomes of primary cystocele repair by transvaginal mesh surgery versus laparoscopic mesh sacropexy: extended follow up of the PROSPERE multicentre randomised trial. BJOG Int J Obstet Gynaecol. 2022;129:127–37.
Lucot J-P, Fritel X, Debodinance P, et al. Étude randomisée comparant la promontofixation cœlioscopique à la chirurgie prothétique par voie vaginale pour le traitement des cystocèles : PROSPERE (PROSthetic PElvic organ prolapse REpair). J Gynecol Obstet Biol Reprod. 2013;42:334–41.
Costantini E, Zucchi A, Lazzeri M, Del Zingaro M, Vianello A, Porena M. Managing Mesh Erosion after Abdominal Pelvic Organ Prolapse Repair: Ten Years’ Experience in a Single Center. Urol Int. 2011;86:419–23.
Baines G, Price N, Jefferis H, Cartwright R, Jackson SR. Mesh-related complications of laparoscopic sacrocolpopexy. Int Urogynecol J. 2019;30:1475–81.
Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309:2016–24.
Pratt TS, Suskind AM. Management of Overactive Bladder in Older Women. Curr Urol Rep. 2018;19:92.
Zhang C, Sun Z, Yang J, Xu T, Zhu L, Lang J. Sacrocolpopexy compared with transvaginal mesh surgery: a systematic review and meta-analysis. BJOG Int J Obstet Gynaecol. 2021;128:14–23.
Author information
Authors and Affiliations
Contributions
N Khalil: Project development, Data collection, Manuscript writing. M Moubarak: Project development, Data analysis, Manuscript editing.
M Alkassis, N Kassis: Project development, Data collection.
M Moukarzel, D Atallah: Project development, Manuscript editing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khalil, N., Moubarak, M., Alkassis, M. et al. Long term follow-up after minimally invasive sacrocolpopexy. Int Urogynecol J 34, 1279–1283 (2023). https://doi.org/10.1007/s00192-022-05430-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05430-z