Abstract
Introduction and hypothesis
The objective was to compare the clinical efficacy and safety of pharmacological interventions for interstitial cystitis and bladder pain syndrome (IC/BPS) with direct and indirect evidence from randomized trials.
Methods
We searched PubMed, the Cochrane library, and EMBASE for randomized controlled trials (RCTs) that assessed the pharmacological therapies for IC/BPS. Primary efficacy outcomes included ICSI (O’Leary Sant Interstitial Cystitis Symptom Index), ICPI (O’Leary Sant Interstitial Cystitis Problem Index), 24-h micturition frequency, visual analog scale (VAS), and Likert score for pain. Safety outcomes are total adverse events (AEs, intravesical instillation, and others), gastrointestinal symptoms, headache, pain, and urinary symptoms. A systematic review and Bayesian network meta-analysis were performed.
Results
A total of 23 RCTs with 1,871 participants were identified. The ICSI was significantly reduced in the amitriptyline group (MD = −4.9, 95% CI: −9.0 to −0.76), the cyclosporine A group (MD = -7.9, 95% CI: −13.0 to −3.0) and the certolizumab pegol group (MD = −3.6, 95% CI:−6.5 to −0.63) compared with placebo group. Moreover, for ICPI, cyclosporine A showed superior benefit compared to placebo (MD = −7.6, 95% CI: −13 to −2.3). VAS score improved significantly in cyclosporine A group than pentosan polysulfate sodium (MD = 3.09, 95% CI: 0.13 to 6.07). None of the agents revealed a significant alleviation of 24-h micturition frequency. In terms of safety outcomes, the incidence rate on urinary symptoms for botulinum toxin A was the only variate higher than chondroitin sulfate (MD = −2.02, 95% CI: −4.99 to 0.66) and placebo (MD = −1.60, 95% CI:−3.83 to 0.17). No significant difference was found among the other treatments.
Conclusions
Cyclosporine A might be superior to other pharmacological treatments in efficacy. Amitriptyline and certolizumab pegol were capable of lowering the ICSI as well.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interstitial cystitis/bladder pain syndrome (IC/BPS) is a urinary bladder disease characterized as lower urinary tract symptoms over 6 weeks with an unpleasant sensation such as discomfort, pain, and pressure [1]. The prevalence of IC/BPS is around 45 out of 10,000 in women and 8 out of 100,000 in men [2]. Pain is a vital symptom of IC/BPS, which is not only suprapubic pain associated with bladder filling but also pelvic pain (urethra, vagina, rectum, etc.) [3]. However, the unitary of definition and management, the optimal treatment, and treatment duration are still absent worldwide [4].
Moreover, various pharmacological therapies with IC/BPS as the target have been discussed, such as intravesical instillation including chondroitin sulfate [5], alkalinized lidocaine [6, 7] and bacillus Calmette–Guerin (BCG) [8]; intravesical injection including onabotulinum toxin A [9,10,11]; oral medication including tricyclic antidepressants, hydroxyzine, cimetidine, and pentosan polysulfate (PPS) sodium [12, 13]; subcutaneous medication including certolizumab pegol, adalimumab, fulranumab; and intravenous medication including tanezumab. However, the highest curative rate is only about 60% [10]. It has been found that IC/BPS is a multi-factorial disease, as along with autoimmunological responses [14], there is damage of the glycosaminoglycan (GAG) layer of the urothelium [15], neurological pain, and inflammatory activities [16]. PPS reduces urothelial permeability by reinforcing the GAG layer. Lidocaine has shown an obvious improvement in IC/BPS symptoms because of its anti-inflammatory function. Heparin-related drugs function as part of GAG family, which promotes the growth of urothelium. Intravesical injection of botulinum toxin A (BoNTA) has shown an improvement in IC/BPS symptoms through detrusor paralysis [17]. Therefore, more effective methods are necessary for patients who do not respond to current therapies.
Although several pairwise meta-analyses and a network meta-analysis have been published [18,19,20], only the outcome of intravesical pharmacotherapies with a limited information supply was provided. Many other drugs have different application methods, and there are no ranking recommendations at present [21]. Hence, we performed this systematic review and Bayesian network meta-analysis to investigate all available pharmacological therapies for more evidence on efficacy and safety for patients with IC/BPS.
Materials and methods
Methodology
We conducted a network meta-analysis based on a Bayesian model of randomized controlled trials (RCTs), comparing pharmacotherapies for IC/BPS. Our network meta-analysis was carried out under the guidance of the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement for network meta-analysis of health care interventions. In addition, the current meta-analysis was registered on PROSPERO (no. CRD42020176627). Commentaries, review articles, editorials, and letters were excluded. All duplicates were excluded, following the literature research.
Search strategy
A search of PubMed, the Cochrane library, EMBASE, and other sources covering English-language articles with full text from August 2003 to June 2020 was carried out. Both text word terms and subject headings (“Interstitial Cystitis” *or* “Bladder Pain Syndrome” *and* “RCT”) were used including MeSH terms in combination with keyword searching (see Supplementary Table 1). All results were restricted to RCTs.
Eligibility and exclusion criteria
Participants of our network meta-analysis were all diagnosed with IC/BPS or refractory IC/BPS. The diagnostic criteria decided by the study authors were based on urinary symptom scores such as an ICSI (O’Leary Sant Interstitial Cystitis Symptom Index) of at least 5, an ICPI (O’Leary Sant Interstitial Cystitis Problem Index) of at least 4, and chronic bladder pain over 6 months, accompanied by urinary urgency, urinary frequency (≥8 voids daily) [22, 23]. In addition, patients with urinary tract infection, bladder outlet obstruction, overactive bladder, or other urological diseases were excluded.
Studies were included if they were prospective RCTs, assessing pharmacotherapy of IC/BPS with a duration of no less than 4 weeks. The intervention arms of our network meta-analysis were all pharmacological therapies. Accordingly, we searched mainly regarding several pharmacological therapies including antidepressants, tumor necrosis factor, anesthetics, toxins, etc. All the interventions were listed in Supplementary Table 1. For studies concerning multiple publications, the most intact or recent version in our analysis was included.
Unavailable data, observational studies, commentaries, and review articles were excluded. Bibliographies of the studies included were hand-searched to ensure completeness. Conference abstracts were not included because of absent or insufficient data. All duplicates were excluded. The comparators were placebo or other related pharmacological treatments eligible in our network meta-analysis.
Outcome measures
The primary outcome was efficacy (ICSI, ICPI, 24-h micturition frequency, visual analog scale [VAS] for pain, Likert score for pain). Secondary outcomes were total adverse events (AEs, intravesical instillation, and others), gastrointestinal symptoms, headache, pain, and urinary symptoms.
Study selection and data extraction
According to the criteria above, two authors (XP Di and DY Luo) performed the study selection independently and strictly. Disagreements were resolved by discussion. Moreover, all baseline information was analyzed thoroughly to avoid bias; such information included age, design, sample size, drugs, as well as efficacy, safety, and adverse events.
Risk of bias assessment
The risk of bias was assessed via the Cochrane Collaboration tool [24] in RevMan version 5.3. Then, selection bias (allocation concealment, random sequence generation), performance bias, attrition bias, reporting bias, and other susceptible sources of bias were analyzed by XP Di and DY Luo separately.
Data analysis
Before the meta-analysis, we summarized the base-line information and outcomes of the studies included. Mean differences (MDs) for continuous variables and risk ratios (RRs) for dichotomous variables with 95% confidence intervals (CIs) were used to present the integrated data.
Both traditional meta-analysis and network meta-analysis were performed. First, a pairwise meta-analysis was performed on a random-effects model. Any outcome covering more than 10 studies was analyzed using Begg’s test to detect publication bias in STATA version 15.1. Once publication bias was detected, Egger’s test or the trim-and-fill method was used for further detection. p ≤ 0.05 indicates significant heterogeneity. Then, a network meta-analysis based on Bayesian frameworks was conducted for direct and indirect treatment comparisons. Considering the heterogeneities among groups, the most recommended random-effects model for analysis was applied. The Markov chain Monte Carlo method was used with four chains in ‘GeMTC’ packages of R version 3.6.1 (https://www.r-progect.org/) [25]. Moreover, we ran models for 150,000 iterations to ensure convergence of the model, which was ensured by density and convergence plots, after discarding the first 20,000 iterations and thinning of 1. We estimated relative probability rankings of each treatment and assessed the hierarchy of competing interventions using the Surface Under the Cumulative Ranking (SUCRA) curve.
As the inclusion criteria were different between studies, a sensitivity analysis was conducted by comparing the Deviance Information Criterion (DIC) between the consistent and inconsistent models for each outcome (https://mtm.uoi.gr/index.php/tutorial/15-tutorial-articles/mtmmetaanalysis/31-generalstatisticalconsiderations).
Results
Search and selection
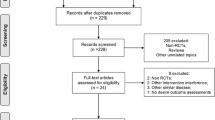
The literature search yielded a total of 2,582 articles, as shown in the PRISMA flowchart. One thousand three hundred and thirty-two titles and abstracts were reviewed after deletion of 1,250 duplicates. Fourty-five articles were eligible for fulltext review. Twenty-two of 45 articles were excluded according to the inclusion and exclusion criteria. Twenty-three RCTs with 1,881 participants were identified after careful revision (Table 1). A summary of the literature review was shown in Fig. 1. A weighted network plot was shown in Fig. 2.
Network plot of pharmacological therapies included in the network meta-analysis. The width of the lines is proportional to the number of trials comparing each pair of treatments, and the size of each circle represents the amount of randomized assigned participants (sample size). ADA adalimumab, AMI amitriptyline, AQX1125 SH2-containing inositol-50-phosphatase1ctivator, BCG bacillus Calmette–Guérin, BoNTA botulinum toxin A, CER certolizumab pegol, CS chondroitin sulfate, CyA cyclosporine A, DMSO dimethyl sulfoxide, FUL fulranumab, HA hyaluronic acid, HA/CS hyaluronic acid plus chondroitin sulfate, LPX lipotoxin, PLA placebo, PPS pentosan polysulfate, PSD597 alkalinized lidocaine, SIL sildenafil, TAN tanezumab
Study and patient characteristics
Publication dates ranged from August 2003 to September 2019 from different regions or nations. The number of patients in each arm ranged from 14 to 134. The follow-up duration ranged from 29 days to 24 months. Most patients were women.
All studies were RCTs, with three triple-arm studies (n = 530) and 20 double-arm (n = 1,351) studies. Placebo was regarded as the most frequent comparator. Nineteen of 23 studies were double-blind trials. The application methods in most studies were intravesical instillation or injection, whereas 5 were orally administered [26, 27, 32, 36, 37], 3 were subcutaneously injected [28,29,30], and 1 was intravenously infused [31]. For intravesical injection, patients received injection of specific drugs about 1 mm into the urothelium at the posterior and lateral wall of the bladder. For subcutaneous injection, drugs or placebo were injected into the thigh (or abdominal wall).
For the primary outcome, 17 out of 23 studies provided the ICSI score. Meanwhile, 15 out of 23 studies provided an ICPI score. For secondary outcomes, 17 out of 23 covered 24-h micturition frequency, and 15 out of 23 reported the pain scores (VAS or Linkert). Fifteen studies depicted the AEs. Further details are shown in Table 1.
Quality of evidence and risk bias
According to the Cochrane risk of bias tool, the quality and risk of bias were carefully assessed. The results showed the high quality and low risk of eligible studies (Fig. 3). The allocation concealment was difficult to figure out, with the possibility of selection bias. Besides, no publication bias was detected in Begg’s test (Fig. S1).
Meta-analysis results
Efficacy
Owing to the differences in application methods and drug dosages, network meta-analysis was performed based on both consistent and inconsistent models to ensure a satisfying convergence among studies.
ICSI
For the ICSI, a network meta-analysis of 17 trials was performed to compare 15 different treatments (n = 1,266, Fig. 4a). Compared with treatment with placebo, the ICSI changed significantly in the amitriptyline group (MD = −4.9, 95% CI:−9.0 to −0.76), the cyclosporine A group (MD = −7.9, 95% CI:−13.0 to −3.0), and the certolizumab pegol group (MD = −3.6,95% CI: −6.5 to −0.63) (Fig. 4b). Data from SUCRA revealed a possible rank as cyclosporine A > amitriptyline > certolizumab pegol > pentosan polysulfate sodium > hyaluronic acid plus chondroitin sulfate > botulinum toxin A > placebo > chondroitin sulfate > hyaluronic acid (Fig. 4c). More indirect comparisons were shown in Fig. 4d.
Analysis of the O’Leary Sant Interstitial Cystitis Symptom Index (ICSI). a Network diagram. b Forest plot. c Surface Under the Cumulative Ranking (SUCRA) plot: with the placebo as the comparator. d League table. Forest plot of the ICSI shows the relative effect of interventions against placebo on the ICSI. The SUCRA curve plot demonstrates the possible hierarchy of pharmacological therapies on the ICSI, and the rankings from 1 to 15 represent the worst to the best. In the league table, when the mean difference with 95% CI displayed above the orange grid is positive, the efficacy of the column-defining treatment is identified as being better than that of the row-defining treatment, and vice versa
ICPI
Fifteen studies were included for the ICPI (n = 1,185, Fig. 5a). The ICPI improved significantly in the cyclosporine A group (MD = −7.6, 95% CI: −13 to −2.3; Fig. 5b). The derived hierarchy was cyclosporine A > certolizumab pegol > hyaluronic acid plus chondroitin sulfate > botulinum toxin A > chondroitin sulfate > placebo > adalimumab (Fig. 5c). More indirect comparisons were shown in Fig. 5d.
Analysis of the O’Leary Sant Interstitial Cystitis Problem Index (ICPI). a Network diagram. b Forest plot: with the placebo as the comparator. c The Surface Under the Cumulative Ranking (SUCRA) plot. d League table. The SUCRA plot demonstrates the possible hierarchy of pharmacological therapies on the ICPI, and the rankings from 1 to 13 represent the worst to the best. In the league table, when the mean difference with 95% CI displayed above the orange grid is positive, the efficacy of the column-defining treatment is identified as being better than that of the row-defining treatment, and vice versa
24-h micturition frequency
Based on available data from 17 studies (n = 1,596, Fig. 6a). None of the treatments was significantly superior to placebo or any other (Fig. 6b, d). The derived hierarchy in micturition frequency alleviation was cyclosporine A > botulinum toxin A > bacillus Calmette–Guérin (BCG) > placebo > chondroitin sulfate > pentosan polysulfate sodium > tanezumab (Fig. 6c). Cyclosporine A might show the greatest improvement in 24-h micturition frequency.
Analysis of 24-h micturition frequency. a Network diagram. b Forest plot: with placebo as the comparator. c Surface Under the Cumulative Ranking (SUCRA) plot. d League table. The SUCRA plot demonstrates the possible hierarchy of pharmacological therapies on 24-h micturition frequency, and the rankings from 1 to 13 represent the worst to the best. In the league table, when the mean difference with 95% CI displayed above the orange grid is positive, the efficacy of the column-defining treatment is identified as being better than that of the row-defining treatment, and vice versa.
Pain scale (VAS and Likert)
As the VAS and the Likert scale are both pain scaling systems with different ceiling scores, the data were analyzed separately.
Seven studies covering 706 patients were included for VAS assessment (Fig. 7a). None of the treatments was significantly superior to placebo (Fig. 7b). The derived hierarchy was cyclosporine A > amitriptyline > certolizumab pegol > botulinum toxin A > lipotoxin > placebo > fulranumab (Fig. 7c). The VAS score improved significantly in the cyclosporine A group compared with the pentosan polysulfate sodium group (MD = 3.09, 95% CI: 0.13 to 6.07; Fig. 7d). Cyclosporine A might show the greatest improvement in VAS score.
Analysis of the visual analog scale (VAS) pain score. a Network diagram. b Forest plot: with placebo as the comparator. c The Surface Under the Cumulative Ranking (SUCRA) plot. d League table. The SUCRA plot demonstrates the possible hierarchy of pharmacological therapies on the VAS, and the rankings from 1 to 8 represent the worst to the best. In the league table, when the mean difference with the 95% CI displayed above the orange grid is positive, the efficacy of the column-defining treatment is identified as being better than that of the row-defining treatment, and vice versa
Seven studies were included for the Likert score (n = 611; Fig. 8a). None of the treatments was significantly superior to placebo or any other groups (Fig. 8b). The derived hierarchy was tanezumab > botulinum toxinA > PSD597 > BCG > placebo > chondroitin sulfate (Fig. 8c). Tanezumab might show the greatest improvement in Likert score. More indirect comparisons are shown in Fig. 8d.
Analysis of the Likert pain score. a Network diagram. b Forest plot: with the placebo as the comparator. c The Surface Under the Cumulative Ranking (SUCRA) plot. d League table. The SUCRA plot demonstrates the possible hierarchy of pharmacological therapies on the Likert score, and the rankings from 1 to 7 represent the worst to the best. In the league table, when the mean difference with 95% CI displayed above the orange grid is positive, the efficacy of the column-defining treatment is identified as being better than that of the row-defining treatment, and vice versa
Safety
The network meta-analysis converged well. Unlike efficacy, the incidence of total AEs might be influenced by doctor-related factors such as catheter insertion-related infection of the urinary system. In order to avoid the bias, the analysis of total adverse events was divided into the intravesical group and the other treatments group. Four typical AEs with high incidence rates were taken into consideration.
Total AEs (intravesical instillation and others)
Fifteen studies were included for AEs (Fig. 9a, b). No significant difference was found in both the intravesical intervention group and the other treatments group (Fig. S2). The derived hierarchy of the risk of total AEs of intravesical instillation was botulinum toxin A > BCG > placebo > PSD597 (Fig. 9c). The derived hierarchy of the risk of total AEs of other treatments was sildenafil > cyclosporine A > tanezumab > placebo > AQX1125 (Fig. 9d).
Analysis of adverse events (AEs). a Network diagram of intravesical instillation. b Network diagram of the other treatments. c The Surface Under the Cumulative Ranking (SUCRA) plot of intravesical instillation. d The SUCRA plot of the other treatments. The SUCRA plot demonstrates the possible hierarchy of pharmacological therapies on AEs, and the rankings from 1 to 4 or 8 represent the highest incidence rate to the lowest
Gastrointestinal symptoms
The network meta-analysis on gastrointestinal symptoms included six studies of seven treatments (n = 859; Fig. S3A). We found no significant difference between any of the treatments (Fig. S3B, C). The probability of gastrointestinal symptoms ranked as pentosan polysulfate sodium > placebo > chondroitin sulfate (Fig. S3D).
Headache
The network meta-analysis on headache included four studies of five treatments (n = 750, Fig. S4A). We found no significant difference between any of the treatments (Fig. S4B, C). Prevalence of headache ranked as sildenafil > placebo > BCG > AQX1125 (Fig. S4D).
Pain
The network meta-analysis on gastrointestinal symptoms included 6 studies on five treatments (n = 733, Fig. S5A). No significant difference was found between any treatments (Fig. S5B, C). The probability of pain incidence was ranked from high to low as BCG > pentosan polysulfate sodium > placebo > AQX1125 > fulranumab (Fig. S5D).
Urinary symptoms
The network meta-analysis on gastrointestinal symptoms included 6 studies on seven treatments (n = 635, Fig. S6A). Botulinum toxin A was superior to chondroitin sulfate (MD = −2.02, 95% CI: −4.99 to 0.66) and placebo (MD = −1.60, 95% CI: −3.83 to 0.17) respectively (Figure S6B, C). The probability of urinary symptoms events incidence rate was ranked from high to low as botulinum toxin A > pentosan polysulfate sodium > placebo > chondroitin sulfate (Fig. S6D).
Sensitivity analysis
As the inclusion criteria of the studies were different, we compared the parameters between a consistent and an inconsistent model of outcomes based on the methodology. It was found that the data were well matched and stable for network meta-analysis (Supplementary Table 2).
Discussion
To our knowledge, this is the first network meta-analysis to investigate the efficacy and safety of eligible pharmacotherapies in clinical use. Using a Bayesian framework, both direct and indirect evidence for pharmacological therapies for IC/BPS were acquired. Although some therapies, such as BCG, are no longer recommended in the guidelines because of unimpressive outcomes and severe adverse effects [14], all the studies were included in order to keep the analysis intact. It was found that besides current mainstream pharmacotherapies such as intravesical instillation or injection [46,47,48], immunoregulators such as cyclosporine A demonstrated a vital role, with relatively higher efficiency and fewer AEs. Cyclosporine A and certolizumab pegol showed a significantly improved ICSI and ICPI compared with other pharmacological therapies. Cyclosporine A and botulinum toxin A were more likely to reduce 24-h micturition frequency. Botulinum toxin A, sildenafil, and cyclosporine A improved the AEs from the hierarchy as well. Moreover, our findings revealed that drugs such as TNFα inhibitors and antidepressants performed better than others as well.
The purpose of our network meta-analysis was a drug-based comparison of the efficacy and safety of 18 pharmacological therapies for IC/BPS. At this time, the etiology of IC was still unclear, some evidence revealed that an abnormal immune response takes place in IC/BPS, which means that immunological regulation in the bladder might be a treatment option for IC/BPS. Tirumuru et al. [49] demonstrated that BoNTA was probably a therapy with a short-term benefit. Crescenze et al. [50] suggested that cyclosporine A might be effective for refractory IC/BPS. Wang and Zhang [51] performed a meta-analysis suggesting that cyclosporine A might be an effective method with a long-term benefit. Giannantoni et al. [33] performed a systematic review of all the possible treatments for IB/BPS, but failed to reach a reliable conclusion because of great heterogeneity in their methodology, among other things. Their results only showed the potential efficiency of cyclosporine A with low-quality evidence. The absence of a comparison between intravesical therapy and other types of drug application methods restricted the utilization of drugs. Regarding safety, AEs of all therapies were evaluated. These adverse events, mostly mild and similar to those in previous studies, constituted the major drawback of these therapies for IC/BPS. There was no significant difference in almost all treatments that might be attributed to application method, drug metabolism, drug dose, etc.
In line with previous studies [36, 52], the results favored cyclosporine A as a potential option for IC/BPS over other treatments. Cyclosporine A is a calcineurin inhibitor that enables suppression of T cell activity and cytokine release [53]. Cyclosporine A has been successfully applied to the management of autoimmune diseases such as Crohn’s disease and rheumatoid arthritis and psoriasis [54, 55]. Generally, cyclosporine A shares not only safety and high efficiency but also long-term therapeutic effect [56]. In addition, cyclosporine A was also considered as a novel choice for refractory IC/BPS [52, 57]. Although cyclosporine A is more likely to cause side effects such as increases in blood pressure and serum creatinine, abdominal pain, flushing, hyperplasia, hair growth, muscle pain, and shaking, there was no significant differences in mean systolic and diastolic blood pressure or serum creatinine during the half-year treatment with cyclosporine A [36]. The importance of drugs such as immunoregulators, antidepressants, or anesthetics for systematic treatment are highlighted.
The most outstanding point of our study is that we compared and ranked the efficacy and safety outcomes of eligible pharmacological interventions with direct and indirect evidence in patients with IC/BPS under a Bayesian network meta-analysis framework. Previous meta-analyses [18, 58,59,60] only focused on intravesical treatments with a relatively higher incidence of side effects.
Furthermore, one crucial aspect that we cannot neglect is the health care cost. Cervigni et al. [34] demonstrated that the incremental cost-effectiveness ratio (ICER) of HA/CS versus DMSO falls between 3,735€/quality-adjusted life years (QALY; an optimistic assumption) and 8,003€/QALY (a pessimistic assumption). One recent study [5] revealed similar efficacy–cost rates on HA and CS. Unfortunately, a cost-effectiveness analysis was not performed in our study as only two eligible studies analyzed health care cost. Further studies should include the direct and indirect analysis of the medical costs in order to acquire a better assessment of pharmacological treatments.
This network meta-analysis had some limitations. First, because most available data showed the comparison between drug and placebo, the lack of comparisons among drugs caused a lack of direct comparisons and looplessness. We tried fixed and random models under consistent and inconsistent models, and the outcomes showed high consistency and low heterogeneity. However, more high-quality RCTs on the direct comparison of drugs are still needed. Second, because of some unavailability of patient data, we were not able to carry out a subgroup analysis of age, gender, etc. Third, no consistent post-treatment follow-up duration for pharmacological therapies of IC/BPS resulted in the failure to compare the efficiency of drugs at different post-treatment times. The selection of outcomes (ICSI, ICPI, 24-h micturition frequency, AEs) is applicable for the purposes of the investigation, whereas other factors may strongly affect outcomes in patients with IC/BPS and have not been included in this systematic review. Given the various outcomes and recommendations of pharmacological therapies, it was found that the preferred intervention may be different because of the endpoints prioritized by patient and physician. Finally, owing to the small patient numbers in some studies, the results may be biased to some extent. For this reason, the efficacy of some therapies, such as cyclosporine A, must be validated in future studies with more patients for a reasonable conclusion. Despite the limitations described above, our network meta-analysis shows the best eligible evidence of the efficacy and safety outcomes of pharmacological interventions and enables us to provide a novel recommendation with less impairment of clinical use in patients with IC/BPS. Researchers have found that IC/BPS is no longer simply an inflammatory disease. In the future, we should concentrate more on multi-factorial treatments instead of monotherapy. More high-quality drug-based, dose-based, and duration-based head-to-head RCTs are needed.
Conclusion
In this systematic review and Bayesian network meta-analysis of pharmacological therapies for patients with IC/BPS, cyclosporine A may be identified as being highlighted to provide more effective benefit. Amitriptyline and certolizumab pegol were capable of lowering the ICSI as well. Alkalinized lidocaine and AQX1125 were more likely to be tolerated than other treatments. These findings may provide novel options for clinicians when making clinical decisions.
References
Hanno P, Dmochowski R. Status of international consensus on interstitial cystitis/bladder pain syndrome/painful bladder syndrome: 2008 snapshot. Neurourol Urodyn. 2009;28(4):274–86. https://doi.org/10.1002/nau.20687.
Patnaik SS, Laganà AS, Vitale SG, Butticè S, Noventa M, Gizzo S, et al. Etiology, pathophysiology and biomarkers of interstitial cystitis/painful bladder syndrome. Arch Gynecol Obstet. 2017;295(6):1341–59. https://doi.org/10.1007/s00404-017-4364-2.
Hanno PM, Erickson D, Moldwin R, Faraday MM. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193(5):1545–53. https://doi.org/10.1016/j.juro.2015.01.086.
Malde S, Palmisani S, Al-Kaisy A, Sahai A. Guideline of guidelines: bladder pain syndrome. BJU Int. 2018;122(5):729–43. https://doi.org/10.1111/bju.14399.
Gülpınar Ö, Esen B, Kayış A, Gökçe Mİ, Süer E. Clinical comparison of intravesical hyaluronic acid and chondroitin sulfate therapies in the treatment of bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. 2018;37(1):257–62. https://doi.org/10.1002/nau.23284.
Parsons CL, Zupkas P, Proctor J, Koziol J, Franklin A, Giesing D, et al. Alkalinized lidocaine and heparin provide immediate relief of pain and urgency in patients with interstitial cystitis. J Sex Med. 2012;9(1):207–12. https://doi.org/10.1111/j.1743-6109.2011.02542.x.
Henry RA, Morales A, Cahill CM. Beyond a simple anesthetic effect: lidocaine in the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. Urology. 2015;85(5):1025–33. https://doi.org/10.1016/j.urology.2015.01.021.
Mayer R, Propert KJ, Peters KM, Payne CK, Zhang Y, Burks D, et al. A randomized controlled trial of intravesical bacillus Calmette–Guerin for treatment refractory interstitial cystitis. J Urol. 2005;173(4):1186–91. https://doi.org/10.1097/01.ju.0000152337.82806.e8.
Chuang Y-C, Kuo H-C. A prospective, multicenter, double-blind, randomized trial of bladder instillation of liposome formulation onabotulinumtoxinA for interstitial cystitis/bladder pain syndrome. J Urol. 2017;198(2):376–82. https://doi.org/10.1016/j.juro.2017.02.021.
Pinto RA, Costa D, Morgado A, Pereira P, Charrua A, Silva J, et al. Intratrigonal OnabotulinumtoxinA improves bladder symptoms and quality of life in patients with bladder pain syndrome/interstitial cystitis: a pilot, single center, randomized, double-blind, placebo controlled trial. J Urol. 2018;199(4):998-1003. https://doi.org/10.1016/j.juro.2017.10.018.
Kuo Y-C, Kuo H-C. O'Leary–Sant symptom index predicts the treatment outcome for OnabotulinumtoxinA injections for refractory interstitial cystitis/bladder pain syndrome. Toxins (Basel). 2015;7(8):2860–71. https://doi.org/10.3390/toxins7082860.
Foster HE Jr, Hanno PM, Nickel JC, Payne CK, Mayer RD, Burks DA, et al. Effect of amitriptyline on symptoms in treatment naïve patients with interstitial cystitis/painful bladder syndrome. J Urol. 2010;183(5):1853–8. https://doi.org/10.1016/j.juro.2009.12.106.
Al-Zahrani AA, Gajewski JB. Long-term efficacy and tolerability of pentosan polysulphate sodium in the treatment of bladder pain syndrome. Can Urol Assoc J. 2011;5(2):113–8. https://doi.org/10.5489/cuaj.10095.
Ogawa T, Ishizuka O, Ueda T, Tyagi P, Chancellor MB, Yoshimura N. Pharmacological management of interstitial cystitis/bladder pain syndrome and the role cyclosporine and other immunomodulating drugs play. Expert Rev Clin Pharmacol. 2018;11(5):495–505. https://doi.org/10.1080/17512433.2018.1457435.
Wyndaele JJJ, Riedl C, Taneja R, Lovász S, Ueda T, Cervigni M. GAG replenishment therapy for bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. 2019;38(2):535–44. https://doi.org/10.1002/nau.23900.
Wammack R, Remzi M, Seitz C, Djavan B, Marberger M. Efficacy of oral doxepin and piroxicam treatment for interstitial cystitis. Eur Urol. 2002;41(6):596–600; discussion 601. https://doi.org/10.1016/s0302-2838(02)00174-4.
Lam KH, Yao G, Jin R. Diverse binding modes, same goal: the receptor recognition mechanism of botulinum neurotoxin. Prog Biophys Mol Biol. 2015;117(2–3):225–31. https://doi.org/10.1016/j.pbiomolbio.2015.02.004.
Zhang W, Deng X, Liu C, Wang X. Intravesical treatment for interstitial cystitis/painful bladder syndrome: a network meta-analysis. Int Urogynecol J. 2017;28(4):515–25. https://doi.org/10.1007/s00192-016-3079-4.
Matsuoka PK, Haddad JM, Pacetta AM, Baracat EC. Intravesical treatment of painful bladder syndrome: a systematic review and meta-analysis. Int Urogynecol J. 2012;23(9):1147–53. https://doi.org/10.1007/s00192-012-1686-2.
Guo C, Yang B, Gu W, Peng B, Xia S, Yang F, et al. Intravesical resiniferatoxin for the treatment of storage lower urinary tract symptoms in patients with either interstitial cystitis or detrusor overactivity: a meta-analysis. PLoS One. 2013;8(12):e82591. https://doi.org/10.1371/journal.pone.0082591.
Davis NF, Brady CM, Creagh T. Interstitial cystitis/painful bladder syndrome: epidemiology, pathophysiology and evidence-based treatment options. Eur J Obstet Gynecol Reprod Biol. 2014;175:30–7. https://doi.org/10.1016/j.ejogrb.2013.12.041.
Hanno PM, Landis JR, Matthews-Cook Y, Kusek J, Nyberg L Jr. The diagnosis of interstitial cystitis revisited: lessons learned from the National Institutes of Health interstitial cystitis database study. J Urol. 1999;161(2):553–7. https://doi.org/10.1016/s0022-5347(01)61948-7.
O'Leary MP, Sant GR, Fowler FJ Jr, Whitmore KE, Spolarich-Kroll J. The interstitial cystitis symptom index and problem index. Urology. 1997;49(5A Suppl):58–63. https://doi.org/10.1016/s0090-4295(99)80333-1.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Neupane B, Richer D, Bonner AJ, Kibret T, Beyene J. Network meta-analysis using R: a review of currently available automated packages. PLoS One. 2014;9(12):e115065. https://doi.org/10.1371/journal.pone.0115065.
van Ophoven A, Pokupic S, Heinecke A, Hertle L. A prospective, randomized, placebo controlled, double-blind study of amitriptyline for the treatment of interstitial cystitis. J Urol. 2004;172(2):533–6. https://doi.org/10.1097/01.ju.0000132388.54703.4d.
Chen H, Wang F, Chen W, Ye X, Zhou Q, Shao F, et al. Efficacy of daily low-dose sildenafil for treating interstitial cystitis: results of a randomized, double-blind, placebo-controlled trial—treatment of interstitial cystitis/painful bladder syndrome with low-dose sildenafil. Urology. 2014;84(1):51–6. https://doi.org/10.1016/j.urology.2014.02.050.
Bosch PC. A randomized, double-blind, placebo-controlled trial of Certolizumab Pegol in women with refractory interstitial cystitis/bladder pain syndrome. Eur Urol. 2018;74(5):623–30. https://doi.org/10.1016/j.eururo.2018.07.026.
Bosch PC. A randomized, double-blind, placebo controlled trial of adalimumab for interstitial cystitis/bladder pain syndrome. J Urol. 2014;191(1):77–82. https://doi.org/10.1016/j.juro.2013.06.038.
Wang H, Russell LJ, Kelly KM, Wang S, Thipphawong J. Fulranumab in patients with interstitial cystitis/bladder pain syndrome: observations from a randomized, double-blind, placebo-controlled study. BMC Urol. 2017;17(1):2. https://doi.org/10.1186/s12894-016-0193-z.
Evans RJ, Moldwin RM, Cossons N, Darekar A, Mills IW, Scholfield D. Proof of concept trial of tanezumab for the treatment of symptoms associated with interstitial cystitis. J Urol. 2011;185(5):1716–21. https://doi.org/10.1016/j.juro.2010.12.088.
Nickel JC, Egerdie B, Davis E, Evans R, Mackenzie L, Shrewsbury SB. A phase II study of the efficacy and safety of the novel Oral SHIP1 activator AQX-1125 in subjects with moderate to severe interstitial cystitis/bladder pain syndrome. J Urol. 2016;196(3):747–54. https://doi.org/10.1016/j.juro.2016.03.003.
Giannantoni A, Bini V, Dmochowski R, Hanno P, Nickel JC, Proietti S, et al. Contemporary management of the painful bladder: a systematic review. Eur Urol. 2012;61(1):29–53. https://doi.org/10.1016/j.eururo.2011.07.069.
Cervigni M, Sommariva M, Tenaglia R, Porru D, Ostardo E, Giammo A, et al. A randomized, open-label, multicenter study of the efficacy and safety of intravesical hyaluronic acid and chondroitin sulfate versus dimethyl sulfoxide in women with bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. 2017;36(4):1178–86. https://doi.org/10.1002/nau.23091.
Davis EL, El Khoudary SR, Talbott EO, Davis J, Regan LJ. Safety and efficacy of the use of intravesical and oral pentosan polysulfate sodium for interstitial cystitis: A randomized double-blind clinical trial. J Urol. 2008;179(1):177–85.
Sairanen J, Tammela TL, Leppilahti M, Multanen M, Paananen I, Lehtoranta K, et al. Cyclosporine A and pentosan polysulfate sodium for the treatment of interstitial cystitis: a randomized comparative study. J Urol. 2005;174(6):2235–8. https://doi.org/10.1097/01.ju.0000181808.45786.84.
Nickel JC, Herschorn S, Whitmore KE, Forrest JB, Hu P, Friedman AJ, et al. Pentosan polysulfate sodium for treatment of interstitial cystitis/bladder pain syndrome: insights from a randomized, double-blind, placebo controlled study. J Urol. 2015;193(3):857–62. https://doi.org/10.1016/j.juro.2014.09.036.
Gülpınar Ö, Esen B, Kayış A, Gökçe Mİ, Süer E. Clinical comparison of intravesical hyaluronic acid and chondroitin sulfate therapies in the treatment of bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. 2017;37(1):257–62.
El-Bahnasy AE, Farahat YA, El-Bendary M, et al. A randomized controlled trail of bacillus calmette-guerin and botulinum toxin-A for the treatment of refractory interstitial cystitis[J]. Urotoday Int J. 2008;02(1).
Nickel JC, Moldwin R, Lee S, Davis EL, Henry RA, Wyllie MJ. Intravesical alkalinized lidocaine (PSD597) offers sustained relief from symptoms of interstitial cystitis and painful bladder syndrome. BJU Int. 2009;103(7):910–8.
Manning J, Dwyer P, Rosamilia A, Colyvas K, Murray C, Fitzgerald E. A multicentre, prospective, randomised, double-blind study to measure the treatment effectiveness of abobotulinum A (AboBTXA) among women with refractory interstitial cystitis/bladder pain syndrome. Int Urogynecol J. 2014;25(5):593–9.
Nickel JC, Egerdie RB, Steinhoff G, Palmer B, Hanno P. A multicenter, randomized, double-blind, parallel group pilot evaluation of the efficacy and safety of intravesical sodium chondroitin sulfate versus vehicle control in patients with interstitial cystitis/painful bladder syndrome. Urology. 2010;76(4):804–9.
Irani D, Heidari M, Khezri AA. The efficacy and safety of intravesical Bacillus-Calmette-Guerin in the treatment of female patients with interstitial cystitis: a double-blinded prospective placebo controlled study. Urol J. 2004 Spring;1(2):90–3.
Propert KJ, Mayer R, Nickel JC, Payne CK, Peters KM, Teal V, et al. Followup of patients with interstitial cystitis responsive to treatment with intravesical bacillus calmette-guerin or placebo. J Urol. 2008;179(2):552–5.
Özkıdık M. Assessment of long-term intravesical hyaluronic acid, chondroitin sulfate and combination therapy for patients with bladder pain syndrome. Cent European J Urol. 2019;72:270–5. https://doi.org/10.5173/ceju.2019.0007.
Lin YH, Chiang BJ, Liao CH (2020) Mechanism of action of botulinum toxin a in treatment of functional urological disorders. Toxins (Basel) 12 (2):129. https://doi.org/10.3390/toxins12020129.
Kocatürk H, Atasoy N, Bedir F, Altay MS, Demirdöğen ŞO, Koç E, et al. Questionnaire-guided evaluation of the effectiveness of long-term intravesical 0.2% chondroitin sulfate therapy in interstitial cystitis. Int Urogynecol J. 2020. https://doi.org/10.1007/s00192-020-04245-0.
Scarneciu I, Bungau S, Lupu AM, Scarneciu CC, Bratu OG, Martha O, et al. Efficacy of instillation treatment with hyaluronic acid in relieving symptoms in patients with BPS/IC and uncomplicated recurrent urinary tract infections—long-term results of a multicenter study. Eur J Pharm Sci. 2019;139:105067. https://doi.org/10.1016/j.ejps.2019.105067.
Tirumuru S, Al-Kurdi D, Latthe P. Intravesical botulinum toxin a injections in the treatment of painful bladder syndrome/interstitial cystitis: a systematic review. Int Urogynecol J. 2010;21(10):1285–300. https://doi.org/10.1007/s00192-010-1162-9.
Crescenze IM, Tucky B, Li J, Moore C, Shoskes DA. Efficacy, side effects, and monitoring of Oral cyclosporine in interstitial cystitis-bladder pain syndrome. Urology. 2017;107:49–54. https://doi.org/10.1016/j.urology.2017.05.016.
Wang Z, Zhang L. Treatment effect of cyclosporine a in patients with painful bladder syndrome/interstitial cystitis: a systematic review. Exp Ther Med. 2016;12(1):445–50. https://doi.org/10.3892/etm.2016.3301.
Forrest JB, Payne CK, Erickson DR. Cyclosporine a for refractory interstitial cystitis/bladder pain syndrome: experience of 3 tertiary centers. J Urol. 2012;188(4):1186–91. https://doi.org/10.1016/j.juro.2012.06.023.
Giusto LL, Zahner PM, Shoskes DA. An evaluation of the pharmacotherapy for interstitial cystitis. Expert Opin Pharmacother. 2018;19(10):1097–108. https://doi.org/10.1080/14656566.2018.1491968.
Dijkmans B, Gerards A. Cyclosporin in rheumatoid arthritis: monitoring for adverse effects and clinically significant drug interactions. BioDrugs. 1998;10(6):437–45. https://doi.org/10.2165/00063030-199810060-00002.
Maza A, Montaudié H, Sbidian E, Gallini A, Aractingi S, Aubin F, et al. Oral cyclosporin in psoriasis: a systematic review on treatment modalities, risk of kidney toxicity and evidence for use in non-plaque psoriasis. J Eur Acad Dermatol Venereol. 2011;25(Suppl 2):19–27. https://doi.org/10.1111/j.1468-3083.2011.03992.x.
Sairanen J, Forsell T, Ruutu M. Long-term outcome of patients with interstitial cystitis treated with low dose cyclosporine A. J Urol. 2004;171(6 Pt 1):2138–41. https://doi.org/10.1097/01.ju.0000125139.91203.7a.
Ehrén I, Hallén Grufman K, Vrba M, Sundelin R, Lafolie P. Nitric oxide as a marker for evaluation of treatment effect of cyclosporine a in patients with bladder pain syndrome/interstitial cystitis type 3C. Scand J Urol. 2013;47(6):503–8. https://doi.org/10.3109/21681805.2013.788552.
Wang J, Wang Q, Wu Q, Chen Y, Wu P. Intravesical botulinum toxin a injections for bladder pain syndrome/interstitial cystitis: a systematic review and meta-analysis of controlled studies. Med Sci Monit. 2016;22:3257–67. https://doi.org/10.12659/msm.897350.
Barua JM, Arance I, Angulo JC, Riedl CR. A systematic review and meta-analysis on the efficacy of intravesical therapy for bladder pain syndrome/interstitial cystitis. Int Urogynecol J. 2016;27(8):1137–47. https://doi.org/10.1007/s00192-015-2890-7.
Dawson TE, Jamison J (2007) Intravesical treatments for painful bladder syndrome/interstitial cystitis. Cochrane Database Syst Rev (4):CD006113. https://doi.org/10.1002/14651858.CD006113.pub2.
Acknowledgements
This study was funded by 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (Grant Nos. ZY2016104) and 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (Grant Nos. ZYGD18011), and 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (Grant Nos. ZYGC18015). Project of Science and Technology Department of Sichuan Province (2018SZ0177, 2018SZ0055).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Table 1
(DOC 20 kb)
Supplementary Table 2
(DOC 21 kb)
Figure S1
(PNG 17 kb)
Figure S2
(PNG 1699 kb)
Figure S3
(PNG 2336 kb)
Figure S4
(PNG 1179 kb)
Figure S5
(PNG 1185 kb)
Figure S6
(PNG 1668 kb)
Rights and permissions
About this article
Cite this article
Di, Xp., Luo, Dy., Jin, X. et al. Efficacy and safety comparison of pharmacotherapies for interstitial cystitis and bladder pain syndrome: a systematic review and Bayesian network meta-analysis. Int Urogynecol J 32, 1129–1141 (2021). https://doi.org/10.1007/s00192-020-04659-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04659-w