Abstract
Introduction and hypothesis
The use of new lightweight meshes in pelvic organ prolapse (POP) surgery may reduce complications related to mesh retraction (chronic pain, dyspareunia, and mesh exposure). The aim of this study was to investigate changes in the area and position of Uphold Lite™ mesh 6 weeks and 12 months after anterior and/or apical prolapse repair.
Methods
This observational prospective multicenter study included patients who had undergone transvaginal surgery for symptomatic POP-Q stage ≥ II anterior and/or apical compartment prolapse with placement of Uphold Lite mesh. The dimensions and position of the mesh were evaluated at 6 weeks and 12 months by ultrasonography. Correlations between ultrasonographic mesh characteristics and POP recurrence were analyzed.
Results
Fifty evaluable women with an average age of 66.8 years were included. No statistically significant difference in mesh area was found between week 6 and month 12 postoperatively, either at rest (1746.92 vs. 1574.48 mm2; p = 0.15) or on Valsalva (1568.81 vs. 1542.98 mm2; p = 0.65). The ROC-AUC of the distance between the mesh and the bladder neck (M-BN) at 6 weeks for predicting cystocele recurrence at 12 months was 0.764 (95% CI 0.573–0.955) at rest and 0.724 (95% CI 0.533–0.916) on Valsalva. An M-BN distance > 12.5 mm could predict cystocele recurrence at month 12 with a sensitivity of 80% and a specificity of 69%.
Conclusions
Ultrasonographic measurements of the Uphold Lite™ mesh appear to remain stable between 6 weeks and 12 months postoperatively. M-BN distance correlates with cystocele recurrence. These results appear to confirm the value of ultrasound in mesh evaluation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Many different surgical techniques are now available for the treatment of pelvic organ prolapse (POP). Anterior vaginal wall prolapse remains difficult to manage and has a high recurrence rate varying between 31 to 69% [1,2,3]. The anatomic success of anterior prolapse repair has been improved by the development of transvaginal mesh surgery [2].
However, various health authorities have questioned the use of transvaginal mesh in recent years, and in 2019 the Food and Drugs Administration banned its use in the US becauase of the risk of graft-specific complications such as mesh exposure and retraction, potentially leading to pain, dyspareunia, and possibly POP recurrence [4, 5]. The improved biocompatibility of lighter weight (≤ 35 g/m2), monofilament, macroporous (pores ≥ 75 μm) polypropylene mesh may prevent these complications [6,7,8].
Ultrasound is a promising method for evaluating meshes after implantation. Polypropylene mesh is hyperechogenic, and various studies have reported the feasibility of mesh analysis using standardized ultrasound [9, 10]. This technique may also help clarify the process behind mesh retraction. Velemir et al. for example found that mesh retraction was associated with a higher risk of prolapse recurrence [11]. One hypothesis for this is that a reduction in mesh surface area reduces the cystocele area covered by the mesh.
The Uphold Lite™ mesh is a new generation of kit used in anterior bilateral sacrospinous fixation. Its lighter weight may help reduce retraction [12, 13] and postoperative complications such as exposure and de novo dyspareunia [14, 15]. However, it is possible that the anchoring system, comprising only two arms, could cause mesh to retract towards the apex and thereby promote POP recurrence.
Few studies have evaluated retraction of these new lightweight meshes. The primary aim of this study was to evaluate changes in mesh area and position between 6 weeks and 12 months after placement.
Materials and methods
This prospective multicenter study, conducted between October 2012 and July 2015, was part of a larger 13-center trial to evaluate the clinical efficacy (anatomic and functional outcomes) and complications of Uphold Lite™ mesh up to 12 months after anterior and/or apical prolapse repair. Informed consent was obtained during the preoperative visit. The trial was approved by the Sud-Méditerranée III ethics committee and registered as NCT01559168 on ClinicalTrial.gov.
All patients older than 50 years and undergoing surgery for POP-Q stage II or more anterior and/or apical prolapse [16] with Uphold Lite™ mesh were included in the original trial. Exclusion criteria included suspected hypersensitivity to polypropylene, concomitant posterior mesh procedure, upper urinary tract obstruction, renal insufficiency, or any pathology that could compromise mesh placement (including autoimmune connective tissue disease or systemic infection). Prolapse staging was performed using the POP-Q classification during a gynecological examination, preoperatively and at 6 months and 12 months postoperatively by the operating surgeon, without blinding. All the women underwent standardized bilateral anterior sacrospinous fixation with transvaginal mesh (Boston Scientific, Montigny-le-Bretonneux, France). The mesh used was the Uphold Lite™ system, which is a lightweight (25 g/m2), monofilament, macroporous polypropylene mesh. All surgeons had participated in pretrial training on the Uphold Lite™ mesh procedure.
The procedure has been described in detail elsewhere [15]. The surgeon performed a vertical anterior colpotomy incision, followed by dissection in the paravesical space and blunt dissection medial to the ischial spine until the sacrospinous ligament was identified and exposed. The mesh arms were inserted using the Capio SLIM suture capturing device (Boston Scientific, Montigny-le-Bretonneux, France) 2 cm medial to the ischial spine. A vaginal pack and urinary catheter were left in place for 24 h. Concomitant surgeries were performed at the surgeon’s discretion where indicated.
Patients were evaluated on day 1, week 6, and months 6 and 12. Anatomic recurrence was defined as stage II or more anterior and/or apical prolapse (points Ba and/or C ≥ 1). Perioperative complications and adverse effects were recorded by the surgeon, and serious adverse events were reported to the health authorities.
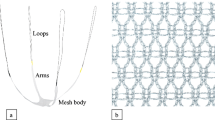
All patients from the original trial who underwent mesh ultrasonography were included in this substudy. Mesh dimensions and topography were evaluated by transvaginal and transperineal ultrasound at 6 weeks and 12 months postoperatively. The surface area of the mesh (in mm2) was calculated from its anteroposterior length measured in the median plane and its width measured in transverse view (Fig. 1), while the distance between the mesh and the bladder neck (M-BN) was measured in the sagittal plane, with the meatus of the urethra visible (Fig. 1). Measurements were taken at rest and on Valsalva.
The primary endpoint was the change in mesh surface area (mesh retraction) between week 6 and month 12. The secondary endpoint was cystocele coverage by the mesh, evaluated by M-BN distance. Other ultrasonographic characteristics reported were mesh folding (defined as a more hyperechoic wavy or thickened appearance of the mesh, suggesting concertina-like folding, with slightly increased acoustic shadowing), mesh detachment (defined as a change in mesh orientation during the Valsalva maneuver), and the presence of a hematoma. Correlations between ultrasonographic characteristics and recurrence were analyzed, including correlation between M-BN distance and cystocele recurrence (point Ba ≥ − 1 or point Ba and point C ≥ -1 when Ba was greater than point C). All mesh ultrasonography was performed by experienced gynecologists using the same measurement protocol, after attending a pretrial workshop.
Statistical analysis
Data on clinical characteristics are presented as frequencies (%, N) for qualitative variables and mean ± standard deviation (SD) for quantitative variables. Continuous variables were compared using Student’s t test or the Mann-Whitney test when normal distribution was not confirmed. Categorical data were compared using the chi-square test.
A stratified recurrence versus non-recurrence analysis was performed using Mann-Whitney tests to evaluate changes in ultrasound measurements between week 6 and month 12, with the threshold of significance set at 5%.
The area under the receiver-operating characteristics curve (ROC-AUC) (DeLong) was used to test correlation between M-BN distance at week 6 and the risk of anatomic recurrence at 12 months and to determine the cutoff M-BN distance predictive of cystocele recurrence.
All data analysis was performed with R 2.9.2 (R Development Core Team (2009), R Foundation for Statistical Computing, Vienna, Austria).
Results
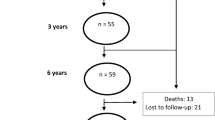
Of the 121 patients included in the main trial from 13 centers, 74 patients from 4 centers underwent ultrasonography at 6 weeks postoperatively, 50 of whom also underwent ultrasonography at 12 months (Fig. 2). The other centers lacked sufficient resources to perform mesh ultrasonography.
Table 1 shows the demographic and preoperative characteristics of the patients included in the main trial and those included in this substudy. These populations appear comparable at baseline, except for differences in the preoperative C-point and rates of prior hysterectomy and prior prolapse surgery, which were lower in the substudy population.
The mean mesh areas at 6 weeks and 12 months, at rest and on Valsalva, are shown in Table 2. No statistically significant reduction in mesh size was found over this period, based on either resting or Valsalva measurements.
The M-BN distance did not change significantly between 6 weeks and 12 months, based on either resting or Valsalva measurements.
During the month 12 ultrasound examination, mesh folding was observed in 10/50 patients (20%), none of whom had pelvic pain or dyspareunia, whereas 2/39 patients (5.1%) without mesh folding reported dyspareunia (p = 1).
Mesh detachment was observed in 4/43 patients (10.7%), with 2 cases of distal detachment (4.7%) and 2 of apical detachment (3.6%). One of the two patients with distal mesh detachment had cystocele recurrence (50%), whereas five patients (13.2%) without distal mesh detachment had cystocele recurrence. Neither of the two patients with apical mesh detachment had apical recurrence, and three patients (8.3%) without apical mesh detachment had apical recurrence.
No hematomas were detected at 12 months, and no mesh exposures were reported in this study.
The anatomic recurrence rate at 12 months was 18% (9/50), comprising 6/50 cases (12%) with recurrence of anterior compartment prolapse only, 1/50 (2%) with apical recurrence only, and 2/50 (4%) with both anterior and apical recurrence. No reinterventions for recurrence were reported.
We observed no significant differences in mesh retraction between the patients with or without anatomic recurrence (Table 3). However, there was a trend towards more retraction at rest in patients with anatomic recurrence (change in mesh area − 228 mm2 [−663; 7] in patients with anatomic recurrence vs. −2.0 mm2 [−254.5; 180.5] in patients without recurrence; p = 0.086).
Focusing on cystocele recurrence alone, we found a trend towards greater M-BN distance at rest at 6 weeks in patients with recurrence (Table 4). This distance was 12 [10; 17] mm in women with cystocele recurrence vs. 10 [9; 13] mm in women without recurrence (p = 0.058).
The ROC-AUC for the use of ultrasonographic M-BN distance at 6 weeks as a test to predict cystocele recurrence at 12 months was 0.764 (95% CI 0.573–0.955) for measurements at rest and 0.724 (95%CI 0.533–0.916) for measurements on Valsalva, making this a good diagnostic tool for predicting recurrence [17]. A cutoff M-BN distance at 6 weeks of 12.5 mm could predict cystocele recurrence at 12 months with a sensitivity of 80% and a specificity of 69%.
Discussion
In this prospective observational study, mesh dimensions remained stable between 6 weeks and 12 months postoperatively. This is consistent with the results of a previous study that reported ultrasonographic data on 40 women seen between 3 and 52 months after surgery [18]. Although other studies have reported significant decreases in mesh dimensions [11, 19], higher weight mesh than the Uphold Lite™ system had been used, and ultrasound measurements were collected at a single time point and compared with in vitro mesh dimensions.
Our results indicate minor mesh retraction; this could suggest that reducing biomaterial load may decrease mesh complications, including retraction. However, further studies with a control group are needed to confirm this hypothesis. Some studies have reported that lighter weight meshes with higher porosity induce a weaker host inflammatory response, thus preventing mesh deformation [12, 20]. This is consistent with clinical results showing low rates of retraction and pelvic pain with Uphold Lite™ mesh [14]. Moreover, some authors have suggested that the contracted appearance of mesh may be the result of physiological healing in the first months after surgery and could be influenced by surgical technique or mesh size [18, 19]. In our study, the distal part of the mesh was fixed laterally to the bladder neck by two absorbable sutures, which may have limited early mesh displacement.
An association between severe retraction and clinical recurrence has been reported [11], with some studies reporting more recurrence in patients with severe retraction. In contrast, we found no significant difference in mesh area between patients with and without recurrence, although we observed a trend towards greater mesh retraction at rest in patients with anatomic recurrence. It is possible that we failed to detect a significant difference because of the small number of patients in our study with recurrence.
According to Velemir et al. ultrasound mesh folding is associated with mesh retraction [11]. Other studies have reported an association between ultrasonographic mesh retraction and vaginal pain [21, 22]. In the present study, we found no correlation between mesh folding and dyspareunia, and indeed none of the ten patients with mesh folding had pelvic pain or dyspareunia. One possible explanation is that lighter weight meshes may undergo less retraction and therefore generate less dyspareunia. It is also possible however that we lacked sufficient affected patients to detect a correlation between retraction and dyspareunia.
We observed few cases of mesh detachment and a low recurrence rate, reducing the possibility of detecting a correlation between apical or distal mesh detachment and recurrence.
The Uphold Lite™ mesh is a two-armed mesh kit anchored to the sacrospinous ligament. We postulated that this anchoring system might cause mesh to contract towards the apex, promoting recurrence of anterior prolapse. In the present study, the M-BN distance remained stable between 6 weeks and 12 months, although there was a trend towards greater M-BN distances in patient with cystocele recurrence. Although our results should be confirmed in a larger sample, they are supported by a study from 2018 in which the distance between Uphold Lite™ mesh and the bladder neck remained stable across measurements at 1, 3, and 12 months at rest. Nevertheless, these authors reported a change in this distance during straining, which could enable cystocele recurrence though the gap [23].
The ROC-AUC for anatomic cystocele recurrence, based on M-BN distance at 6 weeks at rest, showed that this value could help predict cystocele recurrence. We show that a cutoff M-BN distance of 12.5 mm could predict cystocele recurrence at month 12 with a sensitivity of 80% and a specificity of 69%. This could be useful in the follow-up of patients undergoing transvaginal mesh surgery. This finding could be of serious clinical importance because it may also help elucidate the mechanism underlying recurrence after mesh surgery and could help to improve our surgical techniques. This finding is particularly interesting given the ease of access to ultrasound machines and the good feasibility of mesh analysis using standardized ultrasound. The correlation between mesh position and cystocele recurrence has already been reported with laparoscopic sacrocolpopexy, with Wong et al. reporting that for every mm that the mesh was located further from the bladder neck on Valsalva, the likelihood of cystocele recurrence increased by 6–7% [24]. It seems that in prolapse surgery using mesh, mesh location correlates with cystocele recurrence as well in laparoscopic sacrocolpopexy as in transvaginal mesh surgery.
The strengths of this study are its multicenter and prospective design, with prospective evaluation of mesh dimensions in the same patients. It has a number of limitations. First, as it was a substudy, it was not powered on ultrasonographic evaluation, and a large proportion of patients in the index trial did not undergo ultrasonography. Nevertheless, the two populations appear comparable. Second, about one-third of patients who underwent mesh ultrasonography at 6 weeks were subsequently lost to follow-up or were unevaluable for the primary endpoint due to missing data. Third, ultrasound measurements are known to be subject to interobserver variation, although a single operator performed a high volume of ultrasounds (76%), which should limit interobserver variation. Finally, longer-term follow-up is required to confirm our results.
Conclusion
In this multicenter prospective study the dimensions of the Uphold Lite™ mesh appear stable, consistent with minimal retraction of this lightweight mesh. Ultrasonographic measurement of the M-BN distance seems to be useful to predict cystocele recurrence. Ultrasound is a useful tool in the follow-up of mesh-augmented POP surgery with a serious clinical importance.
References
Vollebregt A, Fischer K, Gietelink D, van der Vaart CH. Primary surgical repair of anterior vaginal prolapse: a randomised trial comparing anatomical and functional outcome between anterior colporrhaphy and trocar-guided transobturator anterior mesh. BJOG Int J Obstet Gynaecol. 2011;118:1518–27. https://doi.org/10.1111/j.1471-0528.2011.03082.x.
Maher C, Feiner B, Baessler K, et al. Surgery for women with anterior compartment prolapse. Cochrane Database Syst Rev. 2016;11:CD004014. https://doi.org/10.1002/14651858.CD004014.pub6.
Diez-Itza I, Aizpitarte I, Becerro A. Risk factors for the recurrence of pelvic organ prolapse after vaginal surgery: a review at 5 years after surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1317–24. https://doi.org/10.1007/s00192-007-0321-0.
US FDA: Urogynecologic Surgical Mesh Implants. http://www.fda.gov/medical-devices/implants-and-prosthetics/urogynecologic-surgical-mesh-implants. Published April 16, 2019.
SCENIHR: The safety of surgical meshes used in urogynecological surgery. http://ec.europa.eu/health/scientific_committees/emerging/docs/scenihr_o_049.pdf.
Birch C, Fynes MM. The role of synthetic and biological prostheses in reconstructive pelvic floor surgery. Curr Opin Obstet Gynecol. 2002;14:527–35. https://doi.org/10.1097/00001703-200210000-00015.
Deval B, Haab F. What’s new in prolapse surgery? Curr Opin Urol. 2003;13:315–23. https://doi.org/10.1097/00042307-200307000-00008.
Debodinance P, Berrocal J, Clavé H, et al. Changing attitudes on the surgical treatment of urogenital prolapse: birth of the tension-free vaginal mesh. J Gynecol Obstet Biol Reprod (Paris). 2004;33:577–88. https://doi.org/10.1016/s0368-2315(04)96598-2.
Tunn R, Picot A, Marschke J, Gauruder-Burmester A. Sonomorphological evaluation of polypropylene mesh implants after vaginal mesh repair in women with cystocele or rectocele. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 2007;29:449–52. https://doi.org/10.1002/uog.3962.
Schuettoff S, Beyersdorff D, Gauruder-Burmester A, Tunn R. Visibility of the polypropylene tape after tension-free vaginal tape (TVT) procedure in women with stress urinary incontinence: comparison of introital ultrasound and magnetic resonance imaging in vitro and in vivo. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 2006;27:687–92. https://doi.org/10.1002/uog.2781.
Velemir L, Amblard J, Fatton B, et al. Transvaginal mesh repair of anterior and posterior vaginal wall prolapse: a clinical and ultrasonographic study. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 2010;35:474–80. https://doi.org/10.1002/uog.7485.
Liang R, Knight K, Abramowitch S, Moalli PA. Exploring the basic science of prolapse meshes. Curr Opin Obstet Gynecol. 2016. https://doi.org/10.1097/GCO.0000000000000313.
Patel H, Ostergard DR, Sternschuss G. Polypropylene mesh and the host response. Int Urogynecol J. 2012;23:669–79. https://doi.org/10.1007/s00192-012-1718-y.
Altman D, Mikkola TS, Bek KM, et al. Pelvic organ prolapse repair using the uphold™ vaginal support system: a 1-year multicenter study. Int Urogynecol J. 2016;27:1337–45. https://doi.org/10.1007/s00192-016-2973-0.
Allegre L, Debodinance P, Demattei C, et al. Clinical evaluation of the uphold LITE mesh for the surgical treatment of anterior and apical prolapse: a prospective, multicentre trial. Neurourol Urodyn. 2019;38:2242–9. https://doi.org/10.1002/nau.24125.
Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7.
Šimundić A-M. Measures of diagnostic accuracy: basic definitions. EJIFCC. 2009;19:203–11.
Dietz HP, Erdmann M, Shek KL. Mesh contraction: myth or reality? Am J Obstet Gynecol. 2011;204:173.e1–4. https://doi.org/10.1016/j.ajog.2010.08.058.
Svabík K, Martan A, Masata J, et al. Ultrasound appearances after mesh implantation--evidence of mesh contraction or folding? Int Urogynecol J. 2011;22:529–33. https://doi.org/10.1007/s00192-010-1308-9.
Harsløf S, Zinther N, Harsløf T, et al. Mesh shrinkage depends on mesh properties and anchoring device: an experimental long-term study in sheep. Hernia J Hernias Abdom Wall Surg. 2017;21:107–13. https://doi.org/10.1007/s10029-016-1528-0.
Ostergard DR. Polypropylene vaginal mesh grafts in gynecology. Obstet Gynecol. 2010;116:962–6. https://doi.org/10.1097/AOG.0b013e3181f39b20.
Rogowski A, Bienkowski P, Tosiak A, et al. Mesh retraction correlates with vaginal pain and overactive bladder symptoms after anterior vaginal mesh repair. Int Urogynecol J. 2013;24:2087–92. https://doi.org/10.1007/s00192-013-2131-x.
Lo T-S, Pue LB, Tan YL, et al. Anterior-apical single-incision mesh surgery (uphold): 1-year outcomes on lower urinary tract symptoms, anatomy and ultrasonography. Int Urogynecol J. 2018. https://doi.org/10.1007/s00192-018-3691-6.
Wong V, Guzman Rojas R, Shek KL, et al. Laparoscopic sacrocolpopexy: how low does the mesh go? Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 2017;49:404–8. https://doi.org/10.1002/uog.15882.
Acknowledgments
We thank the BESPIM department of Nîmes University Hospital for statistical analysis and data management.
We thank all the investigators, including those not listed as authors: Philippe Debodinance, Christophe Courtieu, Melanie Cayrac, Xavier Fritel, Maxime Marcelli, Aubert Agostini, and François Monneins.
Funding
This study was partially funded by Boston Scientific, but the company had no influence over the execution of the study, data analysis, or interpretation of the data and was not involved in drafting the manuscript.
Author information
Authors and Affiliations
Contributions
L Allègre: Data collection, Data analysis, Manuscript writing/editing.
G Callewaert: Dataanalysis, Manuscript writing/editing.
C Coudray: Data analysis, Manuscript writing.
C Demattei: Data analysis.
L Panel: Data collection.
C Carlier-Guerin: Data collection.
V Letouzey: Protocol development.
R de Tayrac: Protocol development, Data collection, Manuscript editing.
B Fatton: Protocol development, Data collection, Manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
R. de Tayrac and B. Fatton are consultant for Boston Scientific.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Allègre, L., Callewaert, G., Coudray, C. et al. Prospective ultrasonographic follow-up of transvaginal lightweight meshes: a 1-year multicenter study. Int Urogynecol J 32, 1505–1512 (2021). https://doi.org/10.1007/s00192-020-04483-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04483-2