Abstract
Background
Pelvic floor disorders (PFDs), include urinary incontinence, overactive bladder, anal incontinence, and pelvic organ prolapse negatively affect physical, psychosocial, and economic wellbeing of women. In developing countries, less than a quarter of women with PFDs seek health care for their problem. Health care seeking for PFDs, and its associated factors, is little known in Ethiopia. This study aimed to assess health care seeking for PFDs, associated factors, and deterrents for seeking care.
Methods
From a community based cross sectional study conducted form August 10 to September 4, 2016 to assess pelvic floor disorders, seven hundred four participants with PFDs drawn for health care seeking behavior analysis. Data were collected through interviewed administered questionnaire. Poisson regression model with robust variance was used to investigate the association of the independent variable with health care seeking behaviors. The results are reported in crude and adjusted prevalence ratio with 95% confidence intervals.
Result
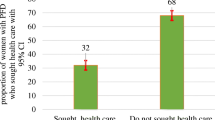
Two hundred twenty five (32%; CI: 26.8–35.5) women sought care for their PFDs. Majority 160 (71%) of them seek care from government health facilities. Middle wealth index Adjusted Prevalence Ratio (APR) = 1.4, CI: 1.1, 1.8), autonomous decision making on own health (APR = 1.3, CI: 1.1, 1.7), and sever impact of PFDs on quality of life (APR = 1.4, CI:1.1, 1.9) were identified as associated factors for health care seeking.
Conclusion
A large number of women with pelvic floor disorder did not seek health care: this calls for urgent and tailored intervention to enhance health care seeking behaviors of women with PFD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic floor disorder (PFD) is a term used to describe conditions related to changes in anatomy or functioning of the pelvic organs, include urinary incontinence, overactive bladder, anal incontinence, and pelvic organ prolapse [1, 2]. The PFDs can occur in isolation or more commonly co-exist together [3]. It has a profound influence on women’s physical, psychological and social lives, and health care costs. It seriously affects physical health by contributing to perineal rash, pressure ulcer, and urinary tract and uterine infection. It also imposes a burden on psychosocial health through creating embarrassment, negative self-perception, depression, and social stigma. Moreover, the global cost of PFDs to the health care system and society is enormous. The average annual cost (direct cost and lost productivity) related to PFDs per person is estimated to be $4110 [4,5,6,7].
Although women with PFDs experiences numerous unfavorable outcomes, a large number of them do not seek health care. Less than one fourth of women with PFDs sought health care in developing countries [4, 8,9,10]. Misconceptions about cause of PFDs and its treatability, sociocultural taboos that prevent disclosing ones’ private conditions to others, economic constraints, and health care workers behaviors negatively influence women’s health care seeking behavior. Women in developing countries silently wait to heal from their problem without seeking care until the disease progressively worsens [11,12,13]. On the other hand, older age, literacy, severe distress of PFDs, and longer duration of PFDs symptoms are reported as facilitating factors to seeking health care for PFDs [14] .
Women develop adaptive behavior and strategies that minimize PFDs’ impact on quality of life (QOL). They only start to search for help when PFDs’ impact worsens and adaptive behaviors fail to maintain expected QOL. Treating PFDs after it reaches the advanced stage has little impact, and the treatment outcome is not satisfactory to revert back to normal as the disease state progresses. Timely and effective treatment of early symptoms may contribute to better recovery, higher QOL, and lower economic burden [5, 13, 14].
In Ethiopia, where only one third of women seek maternal health care, and have limited decision making power [15], health care seeking behaviors for PFDs, deterrents and factors associated to health care seeking is unknown [11, 12]. Therefore, this study aimed to assess health care seeking among women with pelvic floor disorder, identify factors associated with seeking care and explore the barriers against seeking care.
Methods and material
Study area period
This is a part of large scale community based cross sectional study on PFDs and associated factors conducted in Kersa Demographic and Health Surveillance System site (HDSS) in Kersa district. The study was conducted from August 10 to September 4, 2016. The district has 6 health centers and 20 health posts. The site constitutes 26,061 household and 127,000 inhabitants of which 23% are women of reproductive age [16].
Population and sampling technique
The population of this study were drawn from the study population set for investigation of PFDs. Ever-married women who had PFDs (over active bladder, stress urinary incontinence, pelvic organ prolapse and anal incontinence) were included in this study. A multi stage stratified random sampling procedure was used to enroll the study population. The sample was proportionally allocated to each kebele and village per size of house hold. The sample frame is extracted from Kersa HDSS database. Details of methods are described elsewhere [17].
Data collection tools
The questionnaire used to assess the outcome variable (Health seeking behaviors among women with PFDs) was adapted from different literature [4, 18, 19]. To assess PFDs, a standardized data collection tool was customized and adapted from An International Urogynecologic Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female PFD [20], Swedish Pregnancy, Obesity and Pelvic floor [21], and Epidemiology of Incontinence and prolapse Questionnaire [19]. Other explanatory variables including socio-demography and obstetrics condition of study participants were also collected using a structured questionnaire adapted from a health related national survey [22].
The English version of the original questionnaire was translated into local languages (Afan Oromo and Amharic) for data collection. We pretested the questionnaire in a similar setting and refined the tool to fit to the social and cultural norms. Experienced female data collectors and field supervisors fluent in the local languages were recruited and trained for four days in preparation for fieldwork. The data collectors conducted the interviews in a private setting at the interviewee’s house.
Measurement
Health care seeking behavior for PFDs (the outcome variable for this study) was assessed by the following questions: “Have you ever sought care/help for urinary symptoms (this include over active bladder and/or stress urinary incontinence)?” “Have you ever sought care/help for pelvic organ prolapse?” “Have you ever sought care/help for anal incontinence?” The response set was “yes” or “no.” Participants who responded “yes” were considered to be ‘sought care for disorder’ and those who responded “no” were considered to be ‘not sought care for disorder’ for each PFD. The findings from each pelvic floor disorder were combined together to create care seeking behavior for overall PFDs. Those who sought care for at least one of the PFDs is considered to be ‘sought care for overall PFDs’ and those who did not seek health care for any of PFD were considered to be ‘not sought health care for overall PFDs.’
Those who responded “yes” to the question of seek health care, were further interviewed as to where they sought care: “Where/ did you seek care?” The response sets were “government health facilities (government hospital, government health center, and government health post),” “private health facilities (private hospital, private clinic, and private pharmacy),” and “traditional medicine (herbalist, faith healer, and homemade remedy).”
Participants who reported that they never sought help were asked the following question: “What was the reason that you did not seek any care?” The response sets were “Ashamed (shy to disclose their problem to someone or embarrassed),” “do not believe it had treatment options,” “inaccessibility (lack of qualified health care worker, too far from health facilities, lack of transportation services),” “affordability problem (unable to pay for diagnosis and treatment),” and “health care workers bad behavior and /or lack of female health care workers”.
The independent variables included age of respondent, marital status, wealth status, women decision making autonomy, impact of pelvic floor disorder on quality of life, and duration of pelvic floor disorder. Age of respondents were categorized by 10 year intervals (15–24 years, 25–34 year, 35–44 year, 45–54 year, 55+ years); marital status (currently married, widowed/divorced); the wealth index of each household was constructed using principal component analysis and is expressed as wealth quintiles grouped in to three (first tercile ‘poor’, second tercile ‘middle’, and third tercile ‘ better off’); for women’s decision making autonomy, information was collected on three issues that respondents could make decision autonomously: respondent’s own health care, making major household purchases, and visits to family or relatives. Women were considered to participate in a decision if they usually made that decision alone or jointly with their husbands. Options for the questionnaire included “mainly wife”, “mainly husband”, “wife and husband jointly,” and “someone else.” These four categories of response were reduced into two responses; if the response of participants was “mainly wife” and “wife and husband jointly” the responses categorized as ‘women can decide autonomously;’ and if participants’ response was “mainly husband” and “someone else” the responses were categorized in to ‘women cannot decided autonomously.’ Thus, the response is categorized in to “can decide and cannot decide” for the three components [23].
Impact of PFD on quality of life was measured by Pelvic Floor Impact Questionnaire (PFIQ-7). All of the items use the following response scale: 0, not at all; 1, somewhat; 2, moderately; 3, quite a bit. PFIQ-7 Score Scales includes: Urinary Impact Questionnaire (UIQ-7): 7 items under bladder or urine” Colorectal-Anal Impact Questionnaire (CRAIIQ-7): 7 items under Bowel / rectum, Pelvic Organ Prolapse Impact Questionnaire (POPIQ-7): 7 items under “Pelvis / Vagina. To calculate scale scores, the mean value for all of the answered items within the corresponding scale (possible value 0–3) was multiply by (100/3) to obtain the scale score (range 0–100). Scores from the 3 domain (UIQ-7, CRAIIQ-7, and POPIQ-7) scales were added together to obtain the summary score (range 0–300). The severity of impact on quality of life categorized as mild impact 0–33, moderate 34–66, and severe 67–100 for each sub category. For all the three it was categorized as mild impact score 0–100, moderate 101–199 and severe symptoms 200–300 [24]. Impact of pelvic floor disorder was categorized as ‘mild 0–100′, ‘moderate 101–199′, and ‘severe 200–300.’ Duration of the symptoms of PFDs was asked by the following question: “how long did you suffer with PFDs?” the option set was ‘< 1 year’, ‘1–5 year’ and ‘> 5 year’.
Data analysis
Data were double entered into Epi-Data 3.1 and validated for consistency. Data were then exported to STATA version 14 (StataCorp. 2015, Texas) for analysis. Prevalence of care seeking for PFD, where sought health care, and reason for not seeking health care were reported with 95% confidence interval (CI). When the outcome of interest was common (larger than 10%), the odds ratio (OR) overestimates the prevalence ratio (PR) and logistic regression model produces poor estimates. Thus, we used Poisson regression analysis model with robust variance estimation to investigate the association of the independent variables with care seeking for PFDs. Bivariate analysis was first made and the variable with a p value less than 0.2 were consider for the multivariable analysis. These were reported in adjusted prevalence ratio (APR) with 95% CI. P values <0.05 were taken as indicating statistical significance. Multi-collinearity was assessed by variance inflation factors (VIF) and interaction were also checked among the independent variables.
Results
This study encompassed 704 ever-married women reported symptoms of PFDs (over active bladder, stress urinary incontinence, pelvic organ prolapse, and anal incontinence). The mean age and standard deviation of study participants were (39.5 + 13.6 years). One hundred and thirty nine (19.8%) study participants autonomously decided upon their own health care. Two hundred and twenty (31%) women suffered with PFDs for more than five years.
Among 704 women with PFDs, 225(32%; CI: 26.8–35.5) study participants sought health care for their problem. Women with pelvic organ prolapse were most likely to seek care, with 40.3%(95% CI: 35.0–45.7) reporting seeking care. Women who were affected by urinary symptoms(stress urinary incontinence and Over active bladder) were slightly less likely, with 25.9% (95% CI: 22.4–29.7) seeking care. Among 225 women who sought health care, the majority of them 160 (71%) sought help from government health facilities, and the least proportion (15.5%) sought help from traditional medicine (home remedy, herbalist, and religious services) (Table 1).
Among 225 study participants seeking health care, 123 (54.5%) of them sought health care only from one source; 29.7% sought health care form government health facilities only, 16% from private health facilities only, and 8.8% form traditional medicine only. Among those who sought health care from more than one source, 32% of the women visited government health facilities as the first option. The proportion of women who visited a private health facility as the second option was 14.2%, whereas 11.5% visited private health facilities as a first option. About 2 % of women sought care from traditional medicine as the last or third option, and 1.3% as the second option (Fig. 1).
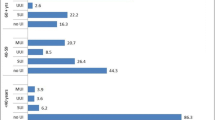
Among 479 participants who did not seek health care, 209 (43.6%) of respondents avoided seeking health care because of they thought PFDs have no treatment, 35% avoided care seeking because of affordability of the treatment and diagnosis, and 16.2% did not seek health care in order not to disclose their condition to health care providers (Fig. 2).
In bivariate analysis, a significant association was observed between care seeking for PFDs and independent variables including older age, currently married, middle wealth status, severely affected quality of life, longer duration of PFDs, and women who can decide autonomously about their own health (Table 2). In multiple Poisson regression analysis care seeking was higher by 40% among middle wealth status individual compare to poor wealth status (APR = 1.4, CI: 1.1, 1.8). Moreover, the prevalence of care seeking was 1.3 times higher among women who can decide autonomously on their own health than those who cannot decide (APR = 1.3, CI: 1.1, 1.7). Those who suffer longer than five years with PFDs were 1.5 times higher in seeking health care than those who suffer with PFDs less than 1 year (APR = 1.5, CI: 1.1, 2.2). Those whose quality of life affected severely were 1.4 times higher in seeking care as compared to those whose quality of life was mildly affected (APR = 1.4, CI:1.1,1.9) (Table 2).
Discussion
In this study, one third of participants sought health care for overall PFDs. A fourth of women with urinary symptoms, two fifth of women with pelvic organ prolapse, and a tenth of women with anal incontinence sought health care for their problem. Two thirds, two fifths, and one sixth of women with pelvic floor disorder visited government health facilities, private health facilities, and traditional medicine for their problems respectively. Women’s economic status, decision-making power, duration of PFDs, and PFD’s impact on quality of life were independently associated with health care seeking behaviors.
In Ethiopia where a fifth of women suffer from PFDs [17], a few of them sought health care. Although sexual function, marital harmony, and social and gender role of women are impacted by PFDs [11, 12, 25, 26], two thirds of them did not seek care. Our finding is consistent with reported prevalence of 29.3% from Turkey [10]. A reported 65.6% women with PFD seeking health care from Lebanon and 57% from USA [27] are higher than our estimate of 32%. And 12.9% prevalence of health care seeking reported from Nigeria [8] is lower than ours. Diversity in care seeking rates is likely due to the differences in cultural background and living standards of the population. In our study 85% of study participants has no formal education, whereas study participants in both Lebanon and USA are more educated. Education as a facilitating factors of care seeking may contribute for difference in care seeking [28]. Similar to our finding, other study demonstrated that women with pelvic organ prolapse more likely to seek health care followed by urinary symptoms, and anal incontinence [27]. The most probable reason why women with pelvic organ prolapse (POP) seek health care more than other types of PFDs may be associated with complication (severity) of advanced POP and availability of surgical treatment in the country.
Against Ethiopian national reproductive health strategy target of treating all (100%) women with Pelvic organ prolapse at hospitals [29], less than half seek care, and 15.5% of them visited non-conventional care (traditional medicine) for their PFDs. Findings from Ethiopia and other developing countries is in agreement with this finding. [8, 11, 26]. Physical discomfort associated with medical diagnosis and treatment, and perceived ineffectiveness of modern medicine to cure PFDs were cited as reasons for women to prefer traditional medicine than modern medicine [26]. Their knowledge on the cause of PFDs influences where to seek health care. Women who have associated evil spirit and bad eye as cause of PFD believed that their condition would not be treated by modern medicine [11, 12]. Moreover, women may seek care from traditional medicine considering it as effective as modern medicine, or their choice may related to cost of treatment as traditional medicine are less expensive compared to modern medicine. Women who seek care from unproven traditional medicine, delay in obtaining scientific and advanced care from health facilities [30]. Relying on traditional medicine may exacerbate their condition and eventually lead to complications and mortality. Working on awareness creation about pelvic floor disorder causes and its treatability at community level or health facilities may minimize delay of care seeking and improve care seeking from health facilities.
Among 479 women who did not seek health care in this study, about half reported they perceived PFDs has no treatment. A significant number of women also avoid seeking care because of economic reasons. Privacy matters to disclose the problem, and inaccessibility of health care services were also mentioned as reason not to seek care for PFDs. Women with PFDs in this setting are challenged with social taboos, lack of information about treatability of the symptoms, and their economic burden. Similar to our findings, other studies from different countries identified lack of knowledge about option of PFDs treatment, behaviors and sex of health care workers, shyness and hesitation to disclose their condition, unaffordability, and access to health facilities as a barrier to care-seeking [4, 5, 26].
Women with gynecological problem in Ethiopia delayed three years in average (ranges 1–10 year) without seeking health care after recognizing their symptom and secretly hiding their condition, even from their family members [25]. Delay in seeking care and suffering in silence would worsen the problem by deterring family support and medical care [11, 12]. These deterrents of health care seeking need a context specific community intervention that will enhance health care seeking by breaking taboos and improving knowledge about prevention and treatment options for pelvic floor disorder. Strengthening community and health service delivery linkage may help to refer women with PFDs for medical care as early as the symptoms observed. Providing free service for gynecological morbidity similar to that of maternal and child health care services in Ethiopia, may encourage women to seek health care, which they missed because of economic reasons [29].
Better economic status, and decision-making power of women for their health are independently associated with health care seeking for the PFDs. This study identified that women who have little economic constraints tend to sought health care. This finding is supported by other studies [5, 11]. In countries, where health care is widely unavailable women’s economic condition affects their access to health care. Women’s empowerment is likely to increase their ability to seek and use health services for their problems. Women who are involved in decision making about their health have had better understanding of treatment and improvement in health outcomes [31]. This study is consistent with other studies concerning women who receive reproductive health services in Ethiopia [23].
Severity of PFDs’ impact on quality of life, and longer duration of the symptoms are strongly associated with health care seeking behavior. Health care seeking for PFDs was higher by 40% among women whose quality of life is severely affected by PFD than those whose quality of life was affected mildly, and health care seeking behavior was higher by 50% among women who had pelvic floor disorder for more than five years compared to those with less than one year. This study demonstrated that women adapt themselves to pelvic floor disorders without seeking health care until their quality of life is severely impacted and the symptoms persist for a longer duration without subsiding. Our finding is consistent with other studies [4, 5, 27].
Limitation of the study
A limitation of this study is that a cross-sectional study design may prove an association but not causality. The self-reported nature of the questionnaire meant that recall and reported bias was inevitable. Moreover, the questionnaire was sensitive to traditional women, under reporting is inevitable.
The main strength of this study is that the study was conducted in an established Health and Demographic Surveillance System location, which provided a robust platform to randomly select participants. Furthermore, data collectors and supervisors were well trained and all questionnaire items were clearly stated, and quality control of the interviews ensured the validity and completeness of the results. Thus, it provides better picture of health care seeking for PFDs than common study conducted at facilities level among women attended health care for various health problem rather than PFDs.
Conclusion
Tolerating and living with this problem may affect the productivity of the women. Cultural taboos associated with reproductive health problem, lack of knowledge on PFDs treatment, and economical constraints have played a great role in deterring women with PFD from seeking health care. On the other hand, women’s empowerment and better wealth status facilitate women to seek health care for their pelvic floor disorder.
This calls for urgent and tailored intervention to enhance health care seeking behaviors of women with PFD: Providing adequate education about cause and treatment PFD, locating available service including conservative treatment, and providing proper incentives (free gynecological morbidity service as with other maternal health services) for the treatment of the PFDs may help women to overcome obstacles that prevent them from seeking health care.
References
Doshani A, Teo REC, Mayne CJ, Tincello DG. Uterine prolapse. BMJ. 2007;335:819–23. https://doi.org/10.1136/bmj.39356.604074.BE.
Brækken IH (2010) Pelvic floor muscle function and Pelvic Organ Prolapse Dissertation from the Norwegian School of Sport Sciences; Oslo.
Lawrence JM, Lukacz ES, Nager CW, Hsu J-WY, Luber KM. Prevalence and co-occurrence of pelvic floor disorders in community-dwelling women. Obstet Gynecol. 2008;111:678–85.
Limpawattana P, Kongbunkiat K, Sawanyawisuth K, Sribenjalux W. Help-seeking behaviour for urinary incontinence: experience from a university community. Int J Urol Nurs. 2015;9(3):143–8. https://doi.org/10.1111/ijun.12065.
Pakgohar M, Sabetghadam S, Rahimparvar SFV, Kazemnejad A. Quality of life (QoL) and help-seeking in postmenopausal women with urinary incontinence (UI): a population based study. Arch Gerontol Geriatr. 2014;59:403–7.
Ian M, Karin SC, Sean N, Marion K, Chieh-I C, Alan JW. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. Eur Urol. 2015;65:7 9–9 5. https://doi.org/10.1016/j.eururo.2013.08.031.
Isuzu M, Holly ER. Impact of fecal incontinence and its treatment on quality of life in women. Women's Health (Lond Engl). 2015;11(2):225–38. https://doi.org/10.2217/whe.14.66.
Morhason-Bello I, Adedokun, Ojengbede, Okonkwo, Kolade (2012) Help-seeking behavior among women currently leaking urine in Nigeria: is it any different from the rest of the world? Patient Prefer Adherence: 815. https://doi.org/10.2147/ppa.s24911.
Fritel X, Panjo H, Varnoux N, Ringa V. The individual determinants of care-seeking among middle-aged women reporting urinary incontinence: analysis of a 2273-woman cohort. Neurourol Urodyn. 2014;33(7):1116–22. https://doi.org/10.1002/nau.22461.
Kılıç M (2016) Incidence and risk factors of urinary incontinence in women visiting Family Health Centers. Springerplus. 5(1331). https://doi.org/10.1186/s40064-016-2965-z.
Gjerde JL, Rortveit G, Muleta M, Blystad A. Silently waiting to heal; experiences among women living with urinary incontinence in Northwest Ethiopia. Int Urogynecol J. 2013;24:953–8.
Gjerde JL, Rortveit G, Muleta M, Adefris M, Blystad A. Living with pelvic organ prolapse: voices of women from Amhara region, Ethiopia. Int Urogynecol J. 2017;28(3):361–6. https://doi.org/10.1007/s00192-016-3077-6.
Wu C, Sun T, Guan X, Wang K. Predicting delay to treatment of urinary incontinence among urban community-dwelling women in China. International Journal of Nursing Sciences. 2015;2(1):34–8. https://doi.org/10.1016/j.ijnss.2015.01.015.
Minassian VA, Yan X, Lichtenfeld MJ, Sun H, Stewart WF. The iceberg of health care utilization in women with urinary incontinence. Int Urogynecol J. 2012;23:1087–93.
Central Statistical Agency (2016) Ethiopian demographic Health Sruvillance https://www.usaid.gov/sites/default/files/documents/1860/EthiopiaDHS2016KIR-Final10-17-2016.pdf. Accessed 5 December, 2016.
Assefa N, Oljira L, Baraki N, Demena M, Zelalem D, Ashenafi W, et al. HDSS profile: the Kersa health and demographic surveillance system. Int J Epidemiol. 2016;45(1):94–101. https://doi.org/10.1093/ije/dyv284.
Dheresa M, Worku A, Oljira L, Mengiste B, Assefa N, Berhane Y (2018) One in five women suffer from pelvic floor disorders in Kersa district Eastern Ethiopia: a community-based study. BMC Women's Health. 18(95). https://doi.org/10.1186/s12905-018-0585-1.
Minassian VA, Yan X, Lichtenfeld MJ, Sun H, Stewart WF. Predictors of care seeking in women with urinary incontinence. Neurourol Urodyn. 2012;31:470–4.
Lukacz ES, Lawrence JM, Buckwalter JG, Burchette RJ, Nager CW, Luber KM. Epidemiology of prolapse and incontinence questionnaire: validation of a new epidemiologic survey. Int Urogynecol J. 2005;16:272–84.
Haylen BT, Dd R, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An international Urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26. https://doi.org/10.1007/s00192-009-0976-9.
Gyhagen M, Åkervall S, Milsom I. Clustering of pelvic floor disorders 20 years after one vaginal or one cesarean birth. Int Urogynecol J. 2015;26:1115–21.
Ethiopian Centeral statistics Agency. ETHIOPIA demographic and health survey 2016. Rockville: Key Indicators Report; 2016.
Central Statistical Agency, ICF International. Ethiopia demographic and health survey 2011 central statistical agency and ICF international. Ethiopia and Calverton: Addis Ababa; 2012.
Nosti PA, McDermott CD, Stehman FB, Schilder JM, Woodman PJ. Symptoms of pelvic floor disorders and quality of life measures in postoperative patients WithEndometrial Cancer. Clinical Ovarian & Other Gynecologic Cancer. 2012;5(1):27–30.
Zeleke BM, Ayele TA, Woldetsadik MA, Bisetegn TA, Adane AA (2013) Depression among women with obstetric fistula, and pelvic organ prolapse in northwest Ethiopia. BMC Psychiatry. 13(236). https://doi.org/10.1186/1471-244X-13-236.
Hemachandra NN, Rajapaksa LC, Manderson L. A “usual occurrence:” stress incontinence among reproductive aged women in Sri Lanka. Soc Sci Med. 2009;69:1395–401.
Morrill M, Lukacz ES, Lawrence JM, Nager CW, Contreras R, Luber KM. Seeking healthcare for pelvic floor disorders: a population-based study. Am J Obstet Gynecol. 2007;197(1):86 e81–6. https://doi.org/10.1016/j.ajog.2007.02.051.
Xu D, Wang X, Li J, Wang K. The mediating effect of ‘bothersome’ urinary incontinence on help-seeking intentions among community-dwelling women. J Adv Nurs. 2015;71(2):315–25. https://doi.org/10.1111/jan.12514.
Ethiopian Minstry of Health (2016) Nationla Reproductive Health Strategy 2016–2020. Ethiopia, Addis Ababa.
Slavin SL, Rogers RG, Komesu Y, Omotosho T, Hammil S, Lewis C, et al. Complementary and alternative medicine (CAM) use in women with pelvic floor disorders: a cohort study. Int Urogynecol J. 2009;21(4):431–7. https://doi.org/10.1007/s00192-009-1058-8.
Sung VW, Raker CA, Myers DL, Clark MA. Treatment decision-making and information-seeking preferences in women with pelvic floor disorders. Int Urogynecol J. 2010;21(9):1071–8. https://doi.org/10.1007/s00192-010-1155-8.
Acknowledgements
We would like to acknowledged Haramaya University and Addis Continental Institute of Public health for their technical and financial support. We thankful to women who responded to this survey.
Funding
This study was financially supported by Haramaya University and Addis Continental Institute of Public Health.
Author information
Authors and Affiliations
Contributions
MD, AW, LO, BM, NA, and YB, contributed to the study design, MD, LO, BM and NA carried out the data collection. MD and AW lead the data analysis and MD, YB, AW, LO, BM and NA reviewed the various version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethics and consent
The study protocol was approved by Haramaya University Health and Medical Sciences College institutional health research ethics review committee. Written informed consent was obtained from each participant. In order to protect the confidentiality of the information, names and ID was not included in the written questionnaires.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dheresa, M., Worku, A., Oljira, L. et al. Women’s health seeking behavior for pelvic floor disorders and its associated factors in eastern Ethiopia. Int Urogynecol J 31, 1263–1271 (2020). https://doi.org/10.1007/s00192-020-04309-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04309-1