Abstract
Introduction and hypothesis
The aim of this study was to compare the outcomes in women who underwent laparoscopic sacrocolpopexy (LSC) with or without hysterectomy for pelvic organ prolapse (POP).
Methods
This was a single-centre prospective study. We included women with symptomatic POP (III–IV stage) who underwent LSC with or without hysterectomy. The preoperative evaluation included a history, clinical examination and urodynamic test; all patients completed FSFI, UDI-6 and IIQ-7 questionnaires. They were followed up at 1, 3, 6 and 12 months after surgery and then annually thereafter with the same preoperative flow chart. At the last visit, they also completed the PGI-I questionnaire.
Results
Between 2012 and 2016, a total of 136 patients with POP were included (82 in the LSC with hysterectomy group and 54 in the hysteropexy group). At a median follow-up of 65.3 months (36–84 months), there were improvements in the anatomical and functional outcomes of both groups without differences between the two approaches. The apical success rate was 100% in all women, without recurrence in either group; the anterior and posterior success rates of hysterectomy were higher than those of uterine preservation.
Conclusion
This study showed that there were no differences in the anatomical and functional outcomes between LSC with or without hysterectomy for POP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In previous years, the surgical treatment for pelvic organ prolapse (POP), in particular uterine prolapse, has been pelvic support correction by hysterectomy. Although the current trend is changing, whether the uterus should be preserved is still under debate for reasons related to the surgeon, the patient, and the organ itself. The literature is limited and full of contradictions, which does not help surgeons make this decision. Few studies have compared abdominal hysterectomy and abdominal hysteropexy [1,2,3,4], and only two have used laparoscopic approaches [4, 5]. These studies had short follow-up periods; of these studies, one was a retrospective study [4], and the author of the other study performed subtotal hysterectomy [5]. The majority of studies compared vaginal hysteropexy and vaginal hysterectomy [6,7,8,9,10,11] or the abdominal and vaginal routes [12].
The aim of this study was to compare the long-term anatomical and functional outcomes of laparoscopic hysterectomy with sacrocolpopexy (LHYSP) with those of laparoscopic hysteropexy (LHSP).
Materials and methods
This single-centre prospective series included women who underwent laparoscopic hysterectomy with sacrocolpopexy (LHYSP) and laparoscopic hysteropexy (LHSP) for symptomatic pelvic organ prolapse.
The inclusion criteria were symptomatic POP stage >II according to the Pelvic Organ Prolapse-Quantification (POP-Q) system, no post-menopausal bleeding, no previous cervical intraepithelial neoplasia, and a minimum of 48 months’ follow-up. The exclusion criteria were malignant or benign uterine lesions, pregnancy or lactation. All women without uterine disease were offered the chance of uterine preservation after careful counselling. The preoperative evaluation included a medical and urogynaecological history, a clinical examination and urodynamic testing. Urinary symptoms, anorectal dysfunction symptoms and sexual dysfunctions were diagnosed according to current recommendations [13] and were evaluated both preoperatively and during the follow-up. The patients preoperatively completed the self-administered Urinary Distress Inventory Short Form (UDI-6) [14], the Incontinence Impact Questionnaire–Short Form (IIQ-7) [15] for urinary symptoms and the Female Sexual Function Index Questionnaire (FSFI) for sexual dysfunction [16]. All surgical procedures were performed by two senior surgeons (E.C., A.Z.), with surgical techniques and meshes that have been described in our previous studies [17, 18].
The patient was placed in the gynaecological position; we used a primary umbilical 12-mm trocar for the 0-degree scope, a 10-mm trocar medial to the superior anterior iliac spine in the dominant hand, another 5-mm trocar medial to the superior anterior iliac spine on the other side and a 5-mm trocar halfway between the symphysis and the umbilicus [17]. The anterior vaginal wall was prepared up to the bladder neck, whereas the posterior vaginal wall was dissected down to the level of the levator ani. Two rectangular polypropylene meshes were attached to the anterior and posterior vaginal walls using four absorbable sutures. The tails of both meshes were fixed to the sacral promontory with a non-absorbable polypropylene suture. The peritoneal incision was reapproximated with a running absorbable suture [17, 18]. When hysteropexy was performed, the anterior mesh was a Y-shaped patch that was attached along the anterior vaginal wall. The right and left edges of the Y-shaped mesh were passed through the round ligaments, and the peritoneum was closed over the mesh [17].
All patients underwent check-ups at 1, 3, 6 and 12 months postoperatively and then annually thereafter, with the same preoperative protocol, except for urodynamic testing. At the last visit, the patients completed self-administered UDI-6, IIQ-7, FSFI and Patient Global Impression of Improvement (PGI-I) questionnaires [19]. Anatomical success was defined as prolapse stage <II in all compartments, point C/D ≤5 and a total vaginal length of at least 7 cm. Failure to correct normal support (stage 0 or I) was considered persistent prolapse, and return to a higher stage following the initial correction was considered prolapse recurrence.
Surgical complications were recorded according to the Clavien–Dindo classification [20]. All data were collected and recorded in our database throughout the entire follow-up period. The local ethics committee approved the study, and the patients signed informed consent documents. Statistical analysis was performed using the non-parametric Mann–Whitney U test for the analysis of continuous variables and the Chi-squared test for categorical data. All calculations were performed using IBM-SPSS® version 22.0 (IBM, Armonk, NY, USA). A two-sided p value <0.05 was considered significant.
Results
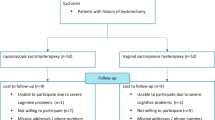
Between January 2012 and January 2016, 139 patients with symptomatic stage >II urogenital POP according to the POP-Q classification underwent sacrocolpopexy in our tertiary urogynaecological centre. Eighty-four women underwent hysterectomy, and 55 chose hysteropexy. Three patients (2 in the LHYSP group and 1 in the LHSP group) were lost to follow-up; thus, a total of 136 patients were included in the study. The demographic and clinical characteristics of the patients included in the hysterectomy group (LHYSP) and hysteropexy group (LHSP) are shown in Table 1. The statistical analysis demonstrated that the women who elected for hysteropexy were younger, were more sexually active, and had less sexual dysfunction than the women who underwent hysterectomy.
Ninety-two percent of women in the LHYSP group were in the menopause. No differences emerged regarding POP, voiding and storage symptoms between the groups.
At a median follow-up of 65.3 months (range 36 to 84 months), the clinical evaluation showed good anatomical correction in both groups (Table 2), with no differences between the LHYSP and LHSP groups. No patients had apical recurrence, and there was a 100% cure rate in both groups. Among the 54 patients in the LHSP group, 4 and 3 patients (7.4% and 5.5%) had asymptomatic anterior and posterior persistence (stage II), respectively. In the LHYSP group, there were three (3.6%) and two (2.4%) cases of asymptomatic stage II persistence in the anterior and posterior compartments, respectively. None of these patients underwent reoperation. None of the women in either group had anterior or posterior prolapse recurrence.
Table 3 shows the functional results, which demonstrate that all symptoms significantly improved postoperatively, with no differences between the two groups.
During the long-term follow-up, there was 1 patient with de novo voiding symptoms and 2 patients with de novo storage symptoms in the LHYSP group, both of whom improved spontaneously. In contrast, in the LHSP group, there were 2 cases of de novo storage symptoms, which were resolved with anticholinergic therapy, although there were 0 cases of de novo voiding symptoms.
Stress urinary incontinence disappeared in 21 (54%) and 15 women (65%) in the LHYSP and LHSP groups respectively. Three cases of de novo SUI developed in each group, and these patients consequently underwent anti-incontinence surgery (tension-free vaginal tape).
Urgency urinary incontinence disappeared in 8 (72.7%) patients in the LHYSP group and 13 (86.6%) patients in the LHSP group, with no differences between the groups. There were no patients with de novo urinary incontinence in either group.
Furthermore, the IIQ-7, UDI-6 and FSFI scores significantly improved in both groups (Table 4).
Regarding patient satisfaction with the operation, the PGI-I scores did not differ between the LHYSP and LHSP groups. The percentages of patients reporting that they were “very much better” or “much better” after the operation were 95% in the LHYSP group and 96% in the LHSP group.
According to the Clavien–Dindo classification, there were two cases of grade I complications (nausea and vomiting) in both groups; there were 5 blood transfusions (grade II) in the LHYSP group, and 1 patient with atrial fibrillation (grade II) and 2 with blood transfusions (grade II) in the LHSP group. In the LHYSP group, there were 9 grade III complications (1 laparocele, 1 ureteral stricture, 1 subcutaneous haematoma and 6 mesh exposures). In the LHSP group, there were 4 complications that required surgical intervention (1 laparocele, 1 stenosis of the sigmoid colon and 2 vaginal mesh exposures). In both groups, the mesh exposure cases were recorded at 12 and 24 months after surgery, and all patients were asymptomatic and did not require treatment. None of the patients had pain or further complications after mesh revision. There were no grade IV or V complications.
All 54 patients in the LHSP group complied with the oncological surveillance guidelines, undergoing annual ultrasound examinations and cervical smears; in 1 patient, evidence of endometrial cancer was found, and this patient was surgically treated.
Discussion
Uterine preservation has always been a highly controversial issue for POP surgery. There are multiple reasons for undergoing uterine-sparing surgery, such as to retain femininity and require a minimally invasive surgery; however, the reasons for undergoing a hysterectomy can also vary, such as to eliminate an unnecessary organ in postmenopausal women, to prevent recurrences and to avoid an eventual second surgery for previous uterine mesh placement. In the literature, there has been only one study that compared laparoscopic hysteropexy with laparoscopic hysterectomy and sacrocolpopexy, and the follow-up was short (median follow-up 33 months) [4].
Our study showed that in the LHSP group, after 5 years, the central prolapse was corrected in 100% of patients, whereas the success rates for the anterior and posterior vaginal compartments were 92.6% and 94.5% respectively. In the LHYSP group, the success rates were 100% for all cases and 96.4% and 97.6% for the anterior and posterior compartments respectively. The time trends were the same for both groups during 5 years of follow-up, without statistically significant differences. There were no recurrences. These results were also confirmed in our previous study with an abdominal approach [1]. In the HYSP group, we showed that 4 years after abdominal surgery, the success rates were 100% for the central compartment, 97.3% for the anterior compartment and 84.21% for the posterior compartment [1]. In the HSP group, the prolapse correction rates were 100%, 85.2% and 91.1% in the central, anterior and posterior compartments respectively [1]. The abdominal technique and the laparoscopic approach were the same.
The HSP group had the highest anterior persistence rate in all our studies, which can be explained by the technical difficulty of dissecting the anterior vaginal wall during uterus-sparing surgery, although the uterus was fixed to the abdominal wall with a straight needle. The persistence rate in the posterior compartment was lower than that in the anterior compartment, probably because of easier dissection of the posterior vaginal wall than of the anterior wall with the laparoscopic approach [17, 21]. Although our laparoscopic technique for dissecting the anterior and posterior vaginal wall and fixing the mesh on the vaginal wall were very different from other techniques presently described in the literature [1, 4], the anatomical success rates and recurrence rates of comparable studies were not similar.
After a median follow-up of 33 months, Pan et al. showed an anatomical success rate of 72.3% in the LHSP group versus 88.2% in the LHYSP group [4], with no difference between the two routes; in their study, there was a recurrence rate of 15% in the vaginal vault after LHSP (p = 0.02) [4]. The patients were treated using vaginal hysterectomy or with a pessary. The difference may be explained by the different anatomical characteristics of the patients or in particular, by the different definitions of success rates used in the two studies. Pan et al. defined an anatomical cure as a prolapse below stage I (all vaginal sites ≥3 cm above the hymenal ring), whereas we defined success as a prolapse below stage II.
The functional outcomes were good in both groups, with no significant differences, as shown by the scores. Good postoperative functional outcomes and improved sexual symptoms were also confirmed after the abdominal approach. In our previous study, 94% of patients resolved the symptoms after HYSP, and 71.4% after HSP [1]. However, in the study by Pan et al., the symptomatic score (PFDI-20, PFIQ-7) after LHYSP was better than that after LHSP (t = 2.40, p = 0.02; t = 2.34, p = 0.02). The authors speculated that this difference was probably due to more subjective discomfort, especially in the lumbosacral region and hypogastrium, and to an increase in anxiety about recurrent uterine prolapse in the LHSP group [4].
The success rate of treating urinary incontinence was high in both groups and did not differ between groups; however, the study conducted by Pan et al. did not explore this parameter [4]. In our study, only 3.7% (LHYSP) and 1.9% (LHSP) of patients have persistent sexual symptoms after surgery. This result was emphasized by improved FSFI scores.
Pan et al. used the PISQ score to evaluate sexual function [4]. The score was better in the LHYSP cohort than in the LHSP group, but the difference was not statistically significant (t = −0.03, p = 0.98). Women in the LHYSP group were more sexually active (41 vs 36 in LHSP), although they were older, than those in the LHSP group (64.8 ± 6.8 vs 56.9 ± 9.2 years). We believe that this finding is only circumstantial; in fact, if we consider the proportion of sexually active women in each group, the proportion is higher in the group who underwent hysteropexy (50% vs 66.7%%), but the difference between the two groups is not significant (p = 0.05). Age can negatively affect sexual activity, but it is not the only factor: personal attitude, a younger or active partner and lifestyle can affect female sexual function. In addition, 22% of the patients in group II had anxiety and depression, which could affect the sexual activity of these women more than age.
After hysterectomy during POP repair, the vaginal length is shorter; however, this does not necessarily result in reduced sexual activity. Many studies have also shown that following vaginal hysterectomy, there is no decline in sexual function.
Siddiqui et al. [22] showed that after colporrhaphy without hysterectomy, the vaginal length was shorter, with a higher frequency of dyspareunia than after colporrhaphy with hysterectomy. However, no significant differences in postoperative sexual function were observed between the two groups. Similar results were also shown by De La Cruz et al. [23] in a retrospective study. In this study, the vaginal length was shorter after vaginal hysterectomy with uterosacral ligament suspension than after robotic-assisted hysterectomy with colpopexy, but sexual function did not differ between the two groups. This can be explained by the improved vaginal bulging symptoms after POP repair, as these symptoms are known to have a negative impact on sexual activity. In the present study, it is important to consider the long-term follow-up and the physiological ageing of women to explain the decrease in sexual activity during the follow-up.
The vaginal mesh exposure rate was low after both techniques, although the rate was higher after LHYSP than after LHSP. All patients were asymptomatic and were managed expectantly [24]. This result was confirmed in the literature, in which the risk of vaginal mesh exposure was significantly increased after total hysterectomy with concomitant sacrocolpopexy (8.6%); in contrast, the rate was 2.2% in those with previous hysterectomy [25,26,27]. In our previous experience, the rate of vaginal mesh exposure was 7.8% after HYSP and 0% after HSP [1]. Pan et al. did not experience vaginal mesh exposure in their two groups [4].
Regarding the other complications, we performed five blood transfusions in the LHYSP group and two blood transfusions in the LHSP group. Our results are from comparing two abdominal techniques. In the literature, there are no studies that compare the perioperative data among abdominal approaches; however, the trend was similar in comparisons of other approaches. In fact, de Oliveira et al. [28], in a systematic review and meta-analysis on hysteropexy versus hysterectomy in the surgical treatment of uterine prolapse, showed that three studies (vaginal hysteropexy versus vaginal hysterectomy without mesh; vaginal hysteropexy versus vaginal hysterectomy with mesh; abdominal hysteropexy versus vaginal hysterectomy without mesh) evaluated intraoperative blood loss in a total of 223 procedures. Overall, the pooled data showed that the volume of blood loss was lower with hysteropexy than with hysterectomy (MD −60.42, 95% CI −71.31 to −49.53; p < 0.00001).
The strengths of our study include the long-term follow-up and an adequate sample size. To our knowledge, this is the only prospective study that compares LHYSP with LHSP.
The weaknesses of this study include the fact that it is a prospective study without randomisation. It is difficult to blind the patients to hysterectomy and uterine preservation for randomisation. Preservation of the uterus, given that the uterus is healthy, should be the patient’s choice, and correct counselling must be provided to the patient, along with the option to change her mind even on the day of the intervention. Finally, the women must be aware that they will need to undergo necessary checks over time if the uterus is preserved. Sometimes the patient does not understand these concepts well and needs several explanations. Furthermore, in this study, counselling was conducted based on our previous results. In our previous trial, we showed that sacrocolpopexy with hysterectomy or hysteropexy had similar results in terms of prolapse resolution, urodynamic outcomes, improved voiding and sexual dysfunctions [1]. Based on these findings, the patients can choose which method they prefer.
In conclusion, the long-term results regarding prolapse resolution, functional outcomes and global patient satisfaction were excellent after both surgical techniques. Therefore, the choice of uterine preservation depends on the technical ability of the surgeon, the presence of uterine diseases and the desires of the patient. In fact, deciding to undergo hysterectomy is a difficult decision for any woman, especially those who are sexually active or have a body image centred upon the uterus. Women should be informed of the surgical procedure and then carefully counselled on the available options to make the decision that is right for them, taking into consideration their desires and expectations.
References
Costantini E, Mearini L, Bini V, Zucchi A, Mearini E, Porena M. Uterus preservation in surgical correction of urogenital prolapse. Eur Urol. 2005;48(4):642–9.
Jeon MJ, Jung HJ, Choi HJ, Kim SK, Bai SW. Is hysterectomy or the use of graft necessary for the reconstructive surgery for uterine prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(3):351–5.
Bai SW, Kim EH, Shin JS, Kim SK, Park KH, Lee DH. A comparison of different pelvic reconstruction surgeries using mesh for pelvic organ prolapse patients. Yonsei Med J. 2005;46(1):112–8.
Pan K, Cao L, Ryan NA, Wang Y, Xu H. Laparoscopic sacral hysteropexy vs laparoscopic sacrocolpopexy with hysterectomy for pelvic organ prolapse. Int Urogynecol J. 2016;27:93–101.
Gracia M, Perello M, Bataller E, et al. Comparison between laparoscopic sacral hysteropexy and subtotal hysterectomy plus cervicopexy in pelvic organ prolapse: a pilot study. Neurourol Urodyn. 2015;34:654–8.
Maher CF, Cay MP, Slack MC, Murray CJ, Milligan M, Schluter P. Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Int Urogynecol J. 2001;12:384–5.
Hefni M, El-Toukhy T, Bhaumik J, Katsimanis E. Sacrospinous cervicocolpopexy with uterine conservation for uterovaginal prolapse in elderly women: an evolving concept. Am J Obstet Gynecol. 2003;188:645–50.
Van Brummen HJ, van de Pol G, Aalders CI, Heintz AP, van der Vaart CH. Sacrospinous hysteropexy compared to vaginal hysterectomy as primary surgical treatment for a descensus uteri: effects on urinary symptoms. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:350–5.
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21(2):209–16.
Hefni MA, El-Toukhy TA. Long-term outcome of vaginal sacrospinous colpopexy for marked uterovaginal and vault prolapse. Eur J Obstet Gynecol Reprod Biol. 2006;127(2):257–63.
Kovac SR, Cruikshank SH. Successful pregnancies and vaginal deliveries after sacrospinous uterosacral fixation in five of nineteen patients. Am J Obstet Gynecol. 1993;168(6 Pt 1):1778–83; discussion 83–8.
Roovers JP, van der Vaart CH, van der Bom JG, van Leeuwen JH, Scholten PC, Heintz AP. A randomised controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function. BJOG. 2004;111(1):50–6.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol Urodyn. 1995;14(2):131–9.
Artibani W, Pesce F, Prezioso D, Scarpa RM, Zattoni F, Tubaro A, et al. Italian validation of the urogenital distress inventory and its application in LUTS patients. Eur Urol. 2006;50:1323–9.
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208.
Illiano E, Ditonno P, Giannitsas K, et al. Robot-assisted vs laparoscopic sacrocolpopexy for high-stage pelvic organ prolapse: a prospective, randomized, single-center study. Urology. 2019;134:116–23.
Balsamo R, Illiano E, Zucchi A. Sacrocolpopexy with polyvinylidene fluoride mesh for pelvic organ prolapse: mid term comparative outcomes with polypropylene mesh. Eur J Obstet Gynecol Reprod Biol. 2018;220:74–8.
Srikrishna S, Robinson D, Cardozo L. Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21:523–8.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Costantini E, Mearini L, Lazzeri M, Bini V, Nunzi E, di Biase M, et al. Laparoscopic versus abdominal sacrocolpopexy: a randomized. controlled trial. J Urol. 2016;196(1):159–65.
Siddiqui NY, Fulton RG, Kuchibhatla M, Wu JM. Sexual function after vaginal versus nonvaginal prolapse surgery. Female Pelvic Med Reconstr Surg. 2012;18(4):239–42.
De La Cruz JF, Myers EM, Geller EJ. Vaginal versus robotic hysterectomy and concomitant pelvic support surgery: a comparison of postoperative vaginal length and sexual function. J Minim Invasive Gynecol. 2014;21(6):1010–4.
Illiano E, Giannitsas K, Li Marzi V, et al. No treatment required for asymptomatic vaginal mesh exposure. Urol Int. 2019;103(2):223–7.
Wu JM, Wells EC, Hundley AF, et al. Mesh erosion in abdominal sacral colpopexy with and without concomitant hysterectomy. Am J Obstet Gynecol. 2006;194(5):1418–22.
Stepanian AA, Miklos JR, Moore RD, Mattox TF. Risk of mesh extrusion and other mesh-related complications after laparoscopic sacral colpopexy with or without concurrent laparoscopic assisted vaginal hysterectomy: experience of 402 patients. J Minim Invasive Gynecol. 2008;15(2):188–96.
Cundiff GW, Varner E, Visco AG, et al. Risk factors for mesh/suture erosion following sacral colpopexy. Am J Obstet Gynecol. 2008;199(6):688.e1–5.
De Oliveira SA, Fonseca MCM, Bortolini MAT, et al. Hysteropreservation versus hysterectomy in the surgical treatment of uterine prolapse: systematic review and meta-analysis. Int Urogynecol J. 2017;28(11):1617–30.
Author information
Authors and Affiliations
Contributions
E.I.: manuscript writing and editing; K.G.: data analysis and manuscript editing; E.C.: project development.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Illiano, E., Giannitsas, K. & Costantini, E. Comparison between laparoscopic sacrocolpopexy with hysterectomy and hysteropexy in advanced urogenital prolapse. Int Urogynecol J 31, 2069–2074 (2020). https://doi.org/10.1007/s00192-020-04260-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04260-1