Abstract
Objective
Obstetric fistula is a devastating childbirth injury that leaves women incontinent, stigmatized and often isolated from their families and communities. In Ethiopia, although much attention has focused on treating and preventing obstetric fistula, other more prevalent childbirth-related pelvic floor disorders, such as pelvic organ prolapse, non-fistula-related incontinence and post-fistula residual incontinence, remain largely unattended. The lack of international and local attention to addressing devastating pelvic floor disorders is concerning for women in low- and middle-income countries. The objective of this article is to highlight the need for a more comprehsive approach to pelvic floor care and to share our experience in addressing it.
Methods
Here, we share our experience launching one of the first formal training programs in Female Pelvic Medicine and Reconstructive Surgery (FPMRS) in Ethiopia.
Results
This fellowship program provides quality care while strengthening the health system in its local context. This program has positioned Ethiopia to be a regional leader by providing comprehensive training of surgeons and allied health professionals, building appropriate health system and research infrastructure, and developing a formal FPMRS training curriculum.
Conclusion
We hope that sharing this experience will serve as a template for others championing comprehensive pelvic floor care for women in low- and middle-income countries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Obstetric fistula is a devastating childbirth injury that leaves women incontinent, stigmatized and often isolated from their families and communities. In 2003, the United Nations Population Fund (UNFPA) launched the global Campaign to End Fistula, striving to make fistulas as rare in developing countries as they are in the developed world [1]. The prevalence of obstetric fistula is difficult to determine since many women are hesitant to disclose their symptoms for fear of ostracization. Large community-based studies needed to estimate prevalence are difficult to conduct and cost-prohibitive [2]. While meta-analyses calculated the fistula burden among Ethiopian woman (based solely on symptoms) at 71:10,000 [3], in 2015, a smaller cross-sectional, community-based study with diagnostic confirmation estimated the prevalence in three rural zones of Ethiopia as low as 6:10,000 [2]. In Ethiopia, progress in preventing and treating obstetric fistula is largely attributed to the pioneering efforts of Drs. Catherine and Reginald Hamlin, who founded the Addis Ababa Fistula Hospital and its satellite centers. These centers not only provide comprehensive obstetric fistula care, but also train skilled midwives who provide obstetric care in rural communities. The Ethiopian government has also established several initiatives to expand obstetric services [4].
Although much attention has focused on obstetric fistula, other childbirth-related pelvic floor disorders such as pelvic organ prolapse and non-fistula-related incontinence, which are more prevalent, are largely unattended. According to the cross-sectional, community-based study in three rural zones in Ethiopia noted above (n = 23,023 women), researchers found that the prevalence of symptomatic pelvic organ prolapse was much higher (100:10,000) than the prevalence of obstetric fistula (6:10,000) [2]. Women in low- and middle-income countries (LMIC) may acquire more severe pelvic floor disorders at a younger age because of high parity, high risk of prolonged labor, high physical strain in daily life, poor nutrition, and delayed or insufficient care of pelvic floor pathologies [5]. Pelvic floor disorders include prolapse characterized by loss of vaginal support with descent of the uterus, bladder and/or rectum resulting in difficulty in emptying the bladder and/or bowel, urinary and fecal incontinence and pelvic pain. Women are often devastated by these conditions [6,7,8,9]. Although women with and without a history of obstetric fistula are at risk, those treated for obstetric fistulas have sustained greater injuries to their pelvic floor and may be at a higher risk [10,11,12]. An estimated 19–40% of women with obstetric fistula suffer from persistent urinary incontinence even after “successful” closure of their fistula [13,14,15]. While the progress in obstetric fistula prevention and care in Ethiopia is encouraging, the management of the full range of pelvic floor disorders is still in its infancy.
Despite the high prevalence of pelvic floor disorders in LMICs, there are very few formally trained pelvic floor specialists. Although many specialists from developed nations provide evaluation and surgical treatment through humanitarian missions, they generally provide clinical care on a short-term basis with little attention to building long-term local capacity. This is further complicated by the fact that most medical volunteers seem to favor providing care for obstetric fistula patients over other pelvic floor disorders. This is partly due to the availability of funds ear-marked for fistula services, the emotional impact of these women’s stories and the attractiveness for Western medical teams to have a unique global surgical experience in LMIC where obstetric fistulas occur [16]. Furthermore, most global health funding agencies and surgeons involved in the care of fistula patients define success of fistula repair as “successful closure of the hole in the bladder” which gives the false short-term reassurance of “job completed” to donors and healthcare providers alike. Unfortunately, this “success” does not capture the large number of women who continue to have significant pelvic floor dysfunction.
Adequate care for pelvic floor disorders requires training a multidisciplinary team that includes nurses, pelvic floor physical therapists, social workers and physicians specializing in the treatment of pelvic floor disorders. Treatment options need to include both conservative management (first line) and surgical interventions under the direction of specialists in female pelvic medicine and reconstructive surgery. As of 2015, there was no formal training program in this specialty in Ethiopia. Most OBGYN residents trained in LMICs do not have access to specialized expert mentors. Furthermore, the huge unmet need for immediate obstetric care tends to crowd out other less urgent issues, limiting their ability to provide such training. As a result, available training leaves them ill equipped to manage the full range of complexities associated with these conditions. Most women with pelvic organ prolapse or incontinence therefore continue to suffer as their condition worsens. Women who do receive care are often treated by general gynecologists who do not have the proper skills to provide optimal surgical treatment, leaving the women at higher risk for surgical complications or recurrence [17].
Here, we share our experience launching one of the first formal training programs in Female Pelvic Medicine and Reconstructive Surgery (FPMRS) (more commonly known as urogynecology) in Ethiopia. This fellowship program is structured to provide high-quality care while strengthening the health system in its local context [18]. This program has positioned Ethiopia to be a regional leader in pelvic floor care by providing comprehensive training of surgeons and allied health professionals. Such ambitious undertakings require careful oversight and benefit from close partnership with the government, academic institutions, nongovernmental organizations (NGOs), experts and scholars.
Pillars of capacity building
Right partners, right time
The first step in building the FPMRS fellowship training program in Ethiopia was forming trusting partnerships with the appropriate stakeholders at the right time. The impetus to initiate this fellowship program was driven primarily by Ethiopian obstetric fistula surgeons who wanted to expand their training as they struggled to meet the needs of their growing population of patients suffering from prolapse and post-fistula or non-fistula related incontinence. As the numbers of obstetric fistulas have fallen in Ethiopia [4], the awareness of other pelvic floor disorders is on the rise, and the Ministries of Health and Education recognized the need for subspecialty training as a critical step to address these problems. The timing was right for the partners to champion the creation of such a training program.
Sustainable partnership
The key partners in this endeavor included the Mekelle University College of Health Sciences, Hamlin Fistula Ethiopia with its Addis Ababa Fistula Hospital and allied satellite centers, the Worldwide Fistula Fund, Hamlin Fistula USA, Oregon Health & Science University’s (OHSU) Footsteps to Healing, international interdisciplinary faculty, community-based outreach organizations such as Healing Hands of Joy and the Tigray Women’s Association, the Tigray Regional Health Bureau, and the Ethiopian Ministry of Health and the Ministry of Education. These partnerships are built upon trust developed over years of collaboration. As a result, the commitment was strong to champion this goal, to take ownership and to have the capacity to scale it up in the long run.
Partnership agreement
Our multi-institutional partnership agreement involved clear delineation of expected contributions by each partner (Table 1). This agreement is reviewed as needed in consultation with all partners. Core faculty from the US and Europe help provide program oversight, curriculum updates and ongoing mentorship. NGO partners provide financial and human resource support and participate in the fellowship oversight committee. Partners work closely with community-based organizations to reach patients needing clinical care and to help coordinate relevant clinical research. Successful completion of the fellowship training is acknowledged by a certificate bestowed by Mekelle University, the academic home of the fellowship program.
Fellowship training
Curriculum development
The process of curriculum development and training required modification of existing FPMRS training models from developed countries to fit Ethiopian needs. Ethiopian fellows hone their skills in conservative management options and the surgical interventions that can be done safely with limited resources. In Ethiopia, opportunities for intraoperative consultation by subspecialists are limited. Our program incorporates training in basic urologic and colorectal surgery as well as capacity-building in nursing and critical care medicine. Selected faculty mentors with expertise in urogynecology, colorectal surgery, urology, physical therapy, nursing and research from international academic partners in Europe, the US and Latin America provide training. The same faculty mentors return regularly to maintain consistency and continuity. The fellowship training takes 3 years and includes clinical, didactic and research components to ensure that it meets international standards. The senior Ethiopian urogynecology fellows assist in training the junior fellows, thus building their teaching skills as they transition to independence. Fellows also provide training for OBGYN residents from affiliated universities who rotate through the training sites. This promotes cultivation of clinical practitioners who are well informed about appropriate management of women with pelvic floor disorders. This also encourages more gynecologists to champion the establishment of pelvic floor centers at their academic institutions.
During curriculum development, the team discussed the appropriate frequency and duration of visits by mentorship teams. The leadership team sought advice from colleagues at the College of Physicians and Surgeons in Ghana where the first African urogynecology program was launched in collaboration with the International Urogynecologic Association (IUGA). The team discussed ways to ensure that the teaching of fellows did not disrupt their ongoing clinical and administrative responsibilities. This is particularly important in settings where physicians are in low supply and have many other overlapping responsibilities. This was accomplished through brief but high intensity training periods of 1–2 weeks every 1–2 months in tandem with advanced and well-coordinated planning. Other hospital-based capacity-building projects were integrated in a similar fashion. The curriculum was developed by the partners and formally approved by the Ethiopian Ministry of Education in 2015.Table 2 outlines the fellowship curriculum from 2016 to 2017.
Administrative and leadership infrastructure
A fellowship oversight committee meets annually in Ethiopia in conjunction with a week-long continuing medical education program at Mekelle University. The fellowship director, an experienced recently retired urologic surgeon from Germany who specializes in female reconstructive surgery, spends 6–8 months on the ground teaching and overseeing fellowship education. Other members of the committee include representatives of the partnering organizations and qualified faculty mentors. The logistical requirements for a fellowship include the development of an administrative support structure, funding to cover travel and lodging of visiting faculty, and support for educational and research programs for the fellows. Ethiopian fellows are paired with faculty mentors and sometimes with fellows from the US in joint projects to develop their capacity for independent research.
Recruitment
Fellowship candidates submit applications each year, which are reviewed by the fellowship oversight committee. Suitable candidates are interviewed before admission to the program. Our first cohort of fellows was primarily recruited from within the Hamlin Fistula organization from centers across Ethiopia. It was logical to begin in this way because the Hamlin fistula surgeons championed the creation of the fellowship training program as a means of expanding their scope of care. Furthermore, these surgeons are experts in treating obstetric fistula patients with complex pelvic floor conditions. In addition, Hamlin Fistula Centers are well established at multiple sites across Ethiopia, providing an ideal setup to scale up education and clinical services. Many of the Hamlin Fistula Centers are affiliated with academic institutions, which allows fellows and their mentors to provide training to OBGYN residents who rotate through these centers as part of their basic specialty training. This serves to increase urogynecologic clinical skills in the affiliated institutions and stimulates further interest in urogynecology.
Evaluation and certification
The fellows are evaluated by their faculty mentors at the conclusion of each educational block. Feedback is provided to the fellows by the fellowship director. All fellows take written and oral examinations at the conclusion of their training administered by the fellowship director and participating faculty. These examinations include case presentations by the fellows and case-based questions from the faculty, focusing on the comprehensive management of pelvic floor disorders. Fellows must also submit their clinical case logs prior to their oral board examination. Fellows then present their research project at the annual Mekelle Medical Education Collaboration (MMEC), which is hosted by the Mekelle University College of Health Sciences and sponsored by the Worldwide Fistula Fund. The MMEC is a week of intensive didactic education in urogynecology and other women’s health topics presented by fellowship faculty mentors and other invited guest lecturers who are global leaders in women’s health research and education.
Beyond fellowship training
Our program goes beyond fellowship training to include building the overall healthcare capacity of our university partners in areas of nursing, physical therapy education, critical care, hospital quality and systems improvement, and inter-professional team training. Our physical therapy faculty is involved in both individualized pelvic health education and teaching topics related to physical therapy care for pregnancy, labor and delivery as part of a master’s degree program in physical therapy at the Mekelle University College of Health and Sciences. The physical therapists see patients at the Hamlin Fistula centers and on the gynecology wards and clinics at Ayder Comprehensive Specialized Hospital. The partnership is also involved in quality improvement training at the hospital including supporting a master’s level training in International Health Administration and Leadership at McGill University for the director of Quality Improvement at Ayder Referral Hospital. This has resulted in launching new initiatives such as instituting a new inter-professional postoperative pain management program at Ayder Hospital. We use interprofessional team simulation training modules geared towards improving communication between healthcare teams with the goal of improving patient safety and quality of care. A large portion of this work involves identifying systemic and cultural issues that impede communication and effective care.
Impact of fellowship training
Clinical care beyond mission trips
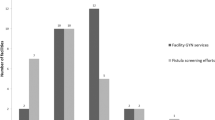
Since the launch of the fellowship in 2015, the care of women with pelvic floor disorders has improved. It is now possible to provide care year-round by local providers. Older, less-effective treatments for prolapse are slowly being replaced by more effective, evidence-based treatments. With the number of documented obstetric fistula repairs occurring in parts of Ethiopia decreasing because of improvements in obstetric care, the Hamlin Fistula Centers have demonstrated their capacity to treat women with more pelvic floor disorders. Figure 1 shows the trend in two satellite Hamlin Fistula Centers where fellowship training is given. Senior fellows are now performing these surgeries with minimal supervision, and newly graduated urogynecologists are involved training junior fellows. We have provided training for our fellows at four different Hamlin Fistula Centers and at Ayder Referral Hospital (Mekelle University College of Health and Sciences). To date, our fellows have provided care for > 500 women with advanced pelvic organ prolapse. The fellowship program is also training other healthcare providers (nurses, midwives, physical therapists, etc.) in conservative management techniques for pelvic floor disorders, such as the use of pessaries, behavioral interventions and pelvic muscle rehabilitation.
Evidence-based medicine
One of the priority areas for the fellowship program is building research infrastructure. The urogynecology fellows are required to complete a research project as part of their training. Fellows are mentored by both local and international research faculty. Examples of current research projects include assessing the outcomes of different surgical procedures for prolapse in Ethiopian women, characterizing the nature of post-repair incontinence in prior fistula patients and assessing feasibility and acceptability of pessary care by midlevel providers in rural district hospitals. These research projects will provide information that can be used to improve the overall quality of care and help identify patients who need treatment. These projects also help reinforce community partnerships with organizations such as Healing Hands of Joy (a fistula reintegration program), the Tigray Women’s Association (a women’s advocacy group with a large community outreach) and the Tigray Regional Health Bureau.
Leadership in pelvic floor health
Our program is developing the future leaders in FPMRS in Ethiopia. The first two urogynecology fellows graduated from this program in March 2018, and five more fellows are currently in training. One of these new fellows, who is an OBGYN faculty member at Mekelle University, will work on developing an academic urogynecology center at his home institution. The two recent graduates from our program currently serve as faculty providing training for the fellows in the program and residents who rotate through their centers. They will also soon take over the fellowship oversight role as fellowship directors.
The fellows’ perspectives
Fellowship training has changed the philosophy of care embraced by fellows with respect to pelvic floor disorders. A selection of fellows shared their perspectives as described below:
“Previously I used to think the patient has a hole in the bladder and once you close the hole, nothing else matters. But that is not true. It turns out the kidney, the ureters, the bladder, the urethra are all part of a single unit. So, when you repair the hole, you have to think about the whole picture. So, I think [the fellowship] totally changed the way I think. Closing the hole is one thing and restoring the function of the urinary system is another. Whenever I think of closing a ‘hole,’ I should think of the ‘whole’ system.”
“For me, the fellowship is a turning point. We recognize the public health problem in this country and the high prevalence of pelvic organ prolapse. The fellowship brings new thinking behind standardizing the proper interventions in prolapse treatment. I’m excited about it because I never thought it would grow in the way it has. So, the fellowship is at the core of everything that is changing: the patients, the doctors and the institutions. Everything goes into this academic exercise and I think that’s the way it should be.”
“I believe we need to create centers of excellence in pelvic floor health to address one of the core issues: improving quality of pelvic floor care. I feel we have a lot to give in terms of training more healthcare providers. So, the fellowship is building capacity. Now it is time to work on how health providers can become compassionate and caring, with a service attitude that they emulate from their mentors.”
Challenges
Coordination of faculty and partners
Coordinating the faculty mentors from various institutions and ensuring that they meet the curricular goals are challenging. Open, clear and regular communication among partners is key to ensuring smooth coordination. In our case, having a dedicated fellowship director at the primary training location was key to alleviating this challenge. Selecting and recruiting expert faculty mentors who volunteer their time on an ongoing basis requires advanced planning. Leveraging relationships with national societies such as the American Urogynecologic Society, International Continence Society and various academic institutions has been very helpful. Political stability is also a challenge where travel is sometimes disrupted by instability in Ethiopia. The declaration of a state of emergency in Ethiopia in 2016 forced some US-based institutions to restrict travel by faculty members. This obstacle has been surmounted by having a wider pool of faculty participants from multiple institutions. Any gains we have made in this fellowship program are certainly at risk of being compromised by any unanticipated instability in leadership and funding among all partner organizations.
Research challenges
Providing sound clinical research training has been challenging in an environment where research infrastructure is lagging. The fellows generally have no more than one local and one international faculty mentor for research. Although they receive didactic sessions in epidemiology and biostatistics, this training is not sufficient. Clinical outcomes research, though critical, is challenging to conduct because of poor access to patients in rural communities. Follow-up continues to be a challenge where patients do not have specific addresses, lack access to mobile phones and do not have reliable transportation. This can partly be surmounted by sound partnership with community outreach organizations. Building the infrastructure for formal, ongoing, clinical research is a long-term priority for our partnership.
Resource limitations
There is limited access to pessaries, suture and other surgical materials, equipment, surgical instruments and medications. Most supplies are donated or purchased from other countries. Even when medical equipment is available, appropriate skills are lacking in maintaining them. Resource limitations and safety concerns require thoughtful planning concerning the types of interventions that can be offered to patients. For example, it is unwise and cost-prohibitive to perform mid-urethral mesh slings in the absence enough resources to carry out the number of procedures needed to master the procedures and to identify and manage complications. In our case, fellows are taught incontinence procedures using autologous fascia or retropubic colposuspensions instead. Another example is the choice of vaginal apical suspension procedure. A sacrospinous ligament fixation is likely safer than a uterosacral ligament suspension if cystoscopy is not routinely available, given the higher risk of ureteric injury with the latter. Even with access to cystoscopy, such complications can occur if a monitor is not available for careful simultaneous visualization of ureteric efflux by mentors and trainees. It is critical that strict ethical oversight is maintained in these resource-limited settings to protect vulnerable patients and minimize unnecessary harm due to mesh- or device-related complications. This requires careful vetting and orientation of faculty mentors. The temptation to use free donated material without proper ethical considerations can do more harm than good.
Recruitment of trainees
Recruiting fellowship candidates who have the commitment to overcome the challenges of a pioneering training program of this kind is challenging. In starting this program, we had one fellow from an academic institution discontinue participation because of conflicting academic demands and lack of adequate commitment to the training program. These challenges have been reduced by recruiting the first six fellows in this program from Hamlin Fistula Centers where they had fewer competing demands beyond pelvic floor care. Hamlin Fistula Ethiopia is also committed to providing the patient care infrastructure and fellow support necessary to sustain the training.
Scaling up: The future of urogynecology training in Ethiopia
Fellowship training in urogynecology in Ethiopia needs to expand across academic centers in the country with appropriate central oversight. Further work is needed to balance the high clinical demands for general OBGYN care with academic requirements for fellows. This is challenging given obstetrician-gynecologists are in short supply and are already stretched in academic institutions. Because most specialists supplement their income through private practice outside of their academic duties, this can compromise available time to commit to more training. This requires special consideration as we help build an infrastructure that will maintain the quality of training. We propose several steps to take to accomplish this goal in Table 3.
Conclusion
Although Ethiopia is making great strides in preventing and treating obstetric fistulas through improvements in maternal health services, comprehensive care for women with other pelvic floor disorders lags significantly behind. These challenges will not be overcome through short-term surgical campaigns by general gynecologists as currently advocated in some parts of Ethiopia. In fact, this strategy may predispose women to worse long-term outcomes. Pelvic organ prolapse and incontinence are chronic conditions in both developing and developed nations and will continue to persist as long as women have babies, grow old and experience risk factors associated with these conditions. These are not disorders that can be “eradicated.” Adequate care for pelvic floor disorders in LMIC requires capacity building in pelvic floor care that goes beyond general gynecologic surgery or obstetric fistula care. The approximate direct cost of running our fellowship program was between $50–60,000/year (not including other hospital capacity-building projects) and relied on contributions from host country institutions as well as international partners. Our program has relied heavily on creating sustainable partnerships, context-specific education and close alignment between mission and vision while promoting the highest values of care. Since the fellowship launched in 2015, many women in Ethiopia are receiving quality pelvic floor care by Ethiopian providers. We acknowledge that setting up a formal urogynecology fellowship training program is not the only way to achieve quality pelvic floor health care as long as gynecologists are provided quality training in advanced pelvic floor medicine and reconstructive surgery and are supported by nurses and pelvic floor physical therapists who can provide conservative care options. We hope that our experience will serve as a practical template for others championing sustainable clinical capacity building not only in Ethiopia but also in other resource-restricted settings where existing partnerships can be leveraged. Our long-term vision is that this program will be transitioned fully to our local partners and scaled across academic centers.
References
Campaign to End Fistula Now Active in 30 Countries | UNFPA - United Nations Population Fund. https://www.unfpa.org/press/campaign-end-fistula-now-active-30-countries. Accessed 4 Jan 2019.
Ballard K, Ayenachew F, Wright J, Atnafu H. Prevalence of obstetric fistula and symptomatic pelvic organ prolapse in rural Ethiopia. Int Urogynecol J. 2016;27:1063–7. https://doi.org/10.1007/s00192-015-2933-0.
Maheu-Giroux M, Filippi V, Samadoulougou S, Castro MC, Maulet N, Meda N, et al. Prevalence of symptoms of vaginal fistula in 19 sub-saharan africa countries: a meta-analysis of national household survey data. Lancet Glob Heal. 2015;3:e271–8. https://doi.org/10.1016/S2214-109X(14)70348-1.
Wright J, Ayenachew F, Ballard K. The changing face of obstetric fistula surgery in Ethiopia. Int J Womens Health Volume. 2016;8:243–8. https://doi.org/10.2147/IJWH.S106645.
Islam RM, Oldroyd J, Karim MN, Hossain SM, Md Emdadul Hoque D, Romero L, et al. Systematic review and meta-analysis of prevalence of, and risk factors for, pelvic floor disorders in community-dwelling women in low and middle-income countries: a protocol study. BMJ Open. 2017;7:1–6. https://doi.org/10.1136/bmjopen-2016-015626.
Ghetti C, Skoczylas LC, Oliphant SS, Nikolajski C, Lowder JL. The emotional burden of pelvic organ prolapse in women seeking treatment: a qualitative study. Female Pelvic Med Reconstr Surg. 2015;21:332–8. https://doi.org/10.1097/SPV.0000000000000190.
Lowder JL, Ghetti C, Nikolajski C, Oliphant SS, Zyczynski HM. Body image perceptions in women with pelvic organ prolapse: a qualitative study. Am J Obstet Gynecol. 2011;204:441.e1–5. https://doi.org/10.1016/J.AJOG.2010.12.024.
Dunivan GC, Anger JT, Alas A, Wieslander C, Sevilla C, Chu S, et al. Pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2014;20:322–7. https://doi.org/10.1097/SPV.0000000000000077.
Laganà AS, La Rosa VL, Rapisarda AMC, Vitale SG. Pelvic organ prolapse: the impact on quality of life and psychological well-being. J Psychosom Obstet Gynecol. 2018;39:164–6. https://doi.org/10.1080/0167482X.2017.1294155.
Murray C, Goh JT, Fynes M, Carey MP. Urinary and faecal incontinence following delayed primary repair of obstetric genital fistula. BJOG An Int J Obstet Gynaecol. 2002;109:828–32. https://doi.org/10.1016/S1470-0328(02)00124-6.
Goh JTW, Krause H, Tessema AB, Abraha G. Urinary symptoms and urodynamics following obstetric genitourinary fistula repair. Int Urogynecol J. 2013;24:947–51. https://doi.org/10.1007/s00192-012-1948-z.
Wall LL. Residual incontinence after obstetric fistula repair. Obstet Gynecol. 2016;128:943–4. https://doi.org/10.1097/AOG.0000000000001734.
Siddle K, Vieren L, Fiander A. Characterising women with obstetric fistula and urogenital tract injuries in Tanzania. Int Urogynecol J. 2014;25:249–55. https://doi.org/10.1007/s00192-013-2185-9.
Browning A. Risk factors for developing residual urinary incontinence after obstetric fistula repair. BJOG An Int J Obstet Gynaecol. 2006;113:482–5. https://doi.org/10.1111/j.1471-0528.2006.00875.x.
Kopp D, Tang J, Bengtson A, Chi B, Chipungu E, Moyo M, et al. Continence, quality of life, and depression following surgical repair of obstetric vesicovaginal fistula: a cohort study. BJOG An Int J Obstet Gynaecol. 2018. https://doi.org/10.1111/1471-0528.15546.
Wall LL, Arrowsmith SD, Lassey AT, Danso K. Humanitarian ventures or “fistula tourism?”: the ethical perils of pelvic surgery in the developing world. Int Urogynecol J. 2006;17:559–62. https://doi.org/10.1007/s00192-005-0056-8.
Gjerde JL, Rortveit G, Adefris M, Belayneh T, Blystad A. Life after pelvic organ prolapse surgery: a qualitative study in Amhara region, Ethiopia. BMC Womens Health. 2018;18:74. https://doi.org/10.1186/s12905-018-0568-2.
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Heal. 2018;6:1196–252. https://doi.org/10.1016/S2214-109X(18)30386-3.
Acknowledgements
We thank the following organizations that have made this work possible: Worldwide Fistula Fund, Hamlin Fistula Ethiopia, Hamlin Fistula USA, Mekelle University, OHSU’s Footsteps to Healing Global Women’s Health Initiative, Ethiopian Ministry of Health and Education, Tigray Regional Health Bureau, Tigray Women’s Association, Healing Hands of Joy, and various faculty from partner academic institutions and organizations who volunteered their time to teach.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The fellowship program is funded by Worldwide Fistula Fund, Hamlin Fistula Ethiopia, Hamlin Fistula USA and Oregon Health & Science University Footsteps to Healing Global Women’s Health Initiative. Dr. Yibrah Berhe and Dr. Renate Roentgen get small salary support from the partners. Drs. Rahel Nardos, Christopher K Payne and Theresa Spitznagle are board members of Worldwide Fistula Fund, Dr. L. Lewis Wall is founder and consultant to Worldwide Fistula Fund, and Dr. Karen Gold is a board member of Hamlin Fistula USA.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nardos, R., Ayenachew, F., Roentgen, R. et al. Capacity building in female pelvic medicine and reconstructive surgery: Global Health Partnership beyond fistula care in Ethiopia. Int Urogynecol J 31, 227–235 (2020). https://doi.org/10.1007/s00192-019-04197-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04197-0