Abstract
Background
Pelvic floor disorders, which diminish the quality of life, disproportionally affect women in developing countries. However, there is a knowledge gap in the understanding of the factors associated with the problem in many countries including Ethiopia. Therefore, we aimed to assess the factors associated with pelvic floor disorders in Ethiopia.
Materials and methods
A community-based cross-sectional study was conducted among 3432 ever-married women selected through a stratified multistage sampling procedure from the Kersa Health and Demography Surveillance System. Data were collected using structured questionnaires through face-to-face interviews. A Poisson regression model with robust variance estimation was used to investigate the association of the independent variable with pelvic floor disorder. The results are reported in adjusted prevalence ratios with 95% confidence intervals.
Results
Overall, the prevalence of pelvic floor disorders was 20.5% (95% CI: 19%–22%). Women who had no education (APR = 1.47; 95% CI: 1.06, 2.04) or had undergone five or more vaginal deliveries (APR = 1.56; 95% CI: 1.18, 2.05), an abortion (APR = 1.85; 95% CI: 1.43, 2.38) or episiotomy (APR = 1.39; 95% CI: 1.02, 1.90) were independently associated with having pelvic floor disorders.
Conclusion
Obstetric events are strongly associated with pelvic floor disorders. This finding highlights the greater need for policies to focus on prevention, diagnosis and treatment services to mitigate women's suffering from pelvic floor disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic floor disorder (PFD), which diminishes quality of life, is a major public health concern for women [1]. It occurs because of defects or disruptions of the pelvic support structures [2]. Weakness of the pelvic musculature, ligaments and fascial support results in pelvic organ prolapse, urinary incontinence and anal incontinence [2, 3].
A combination of anatomical, physiological, genetic, lifestyle and obstetric events contributes to PFD [4, 5]. Although the etiology is known to be multifactorial, obstetric trauma during childbirth has been reported to be one of the key risk factors [6] . High parity and multiple vaginal deliveries contribute to the occurrence of all types of PFD [6, 7].
Underlying causes of PFD such as poor socioeconomic status, being engaged in manual labor on a regular basis, early childbirth and high parity vary greatly among countries [8,9,10]. Thus, women in developing countries are disproportionally affected by PFD. Moreover, racial background influences the magnitude and risk factors of PFD [11]. Identifying relevant PFD risk factors will help to design appropriate prevention strategies to promote women’s health in rural areas of Ethiopia.
Women in rural Ethiopia have low socioeconomic status, low literacy and high fertility with poor obstetric care and as a result suffer greatly from pelvic floor disorders. However, PFD-related information is not collected by national health surveys in Africa [9, 12]. The scanty information generated in Ethiopia is hospital based [13, 14]. Hence, this community-based study focusing on factors associated with PFD was conducted to fill the knowledge gap.
Materials and methods
Study setting and design
A community-based cross-sectional study was conducted from August 10 to September 4, 2016, in the Kersa Health and Demographic Surveillance System (Kersa HDSS) site, Kersa district, Ethiopia. The district has 28.5% arable land, 2.3% pasture and 6.2% forest, and the remaining 56.3% is built up, degraded or otherwise unusable. Khat (Chat Edulis), fruits and vegetables are important cash crops. The study district has 38 kebeles (the smallest administrative unit in Ethiopia) of which 24 randomly selected kebeles were included in Kersa HDSS. The site constitutes 26,061 households and 127,000 inhabitants of which 23% are women of reproductive age [15, 16].
Population and sampling technique
Ever-married women who had resided in the study site for at least 6 months were included in the study. A multi-stage, stratified, random sampling procedure was used to enroll 3444 participants. The sample size was calculated with an assumption of 95% CI, power 80%, a prevalence of PFD among nulliparous women of 13% and of parous women of 18% [17], and a design effect of 2. The Kersa HDSS database was used as a sampling frame. The names of the selected participants and their household IDs were retrieved from the database.
Data collection tools
A standardized data collection tool was customized and adapted from an International Urogynecologic Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female PFD [18], Swedish Pregnancy, Obesity and Pelvic Floor [19] and Epidemiology of Incontinence and Prolapse Questionnaire [20]) to measure pelvic floor disorders. Socio-demographic and obstetric conditions of the study participants were also collected using a structured questionnaire adopted from a health-related national survey [9]. The original questionnaire was prepared in the English language and later translated into the local languages (Amharic and Afan Oromo) for data collection. Forward and backward translations were performed by two bilingual translators.
The content of the questionnaire was validated by gynecologists and reproductive health experts. We pretested the questionnaire in a similar setting and refined the tool based on the feedback we obtained. Experienced female data collectors and field supervisors who can speak the local languages fluently were recruited and trained for 4 days. Field supervisors checked compliance with field procedures and the completeness of questionnaires in the field. They also conducted a spot check for randomly selected interviews. The data collectors conducted interviews in a private setting at the interviewee’s house. The details of this section were presented in a previous study [16]. The study protocol was approved by Haramaya University Health and Medical Sciences College Institutional Health Research Ethics Review Committee. Written informed consent was obtained from each participant. To protect the confidentiality of the information, names and IDs were not included in the written questionnaires.
Measurement
PFD was the outcome variable of this study. PFD was assessed based on women’s reporting of symptoms. Each PFD [stress urinary incontinence (SUI), overactive bladder (OAB), pelvic organ prolapse (POP) and anal incontinence (AI)] was dichotomized as present or absent based on responses to each symptom domain. Women who had at least one PFD were categorized as ‘have PFD,’ and women who did not report at least one PFD were categorized as ‘do not have PFD.’
The independent variables included socio-demographic characteristics, obstetric history and personal characteristics. Socio-demographic variables included marital status, coded as currently married and widowed/divorced; frequency of marriage, coded as married once and married more than once; educational level, coded as has no education and has some education; age at first marriage, categorized as 10–14 years old, 15–18 years old and 19 years old and above. The obstetric history was coded as follows: vaginal parity, coded as vaginal para 1–4 and vaginal para 5 and above; ever had an abortion, coded as yes and no; ever had an episiotomy, coded as yes and no. Personal characteristics including khat chewing, and current contraceptive use was coded as yes and no. Khat (Chat edulis) is an evergreen shrub that grows in Ethiopia, Kenya and Yemen. The use of khat is an established cultural tradition for many social situations in the areas of primary cultivation, East Africa and the Arabian Peninsula [21]. We considered khat in this study since it is commonly consumed in the study area.
Data analysis
Study participants were dichotomized into women with and without PFD based on reported symptoms. Factors associated with PFD were examined using independent variables, including socio-demographic variables, obstetric variables and personal behaviors. Data were analyzed using STATA version 14 (StataCorp 2015, College Station, TX).
A Poisson regression analysis model with robust variance estimation was used to investigate the association of the independent variables with pelvic floor disorder. The variables with a p value < 0.2 in bivariate analysis were considered for a subsequently built multivariable model. Four separate regression models were built to assess the association of independent variables with PFD. The first three models were used to check the effect of variables on each other in a block before entering them into the final model. Model I was built to examine the association of socio-demographic variables with pelvic floor disorder. Subsequently, obstetric history variables were included in Model II to assess their association with PFDs when controlling for socio-demographic variables. The third model (Model III) was built with personal behavior variables when controlling for other variables. Lastly, all variables with a p value < 0.2 from the three separate models were entered together into the final model (Model IV). The results were reported as adjusted prevalence ratios (APRs) with 95% CI. The statistical level of significance was set at alpha 5%. Multi-collinearity was assessed by variance inflation factors (VIFs), and interactions were checked among the independent variables. Age of respondents, gravida and parity were not included in the model as they were correlated with the vaginal delivery variable.
Results
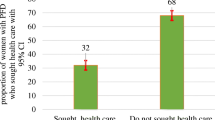
Three thousand four hundred thirty-two women were included in this analysis. Among the participants, 704 (20.5%) (95% CI: 19%, 22%) were classified as having PFD. Further description of PFDs among this population can be found in a previous manuscript [16]. A higher prevalence of PFD was observed among remarried women compared with women who married only once [24.5% (95% CI: 20.25, 29.0) vs. 20.0 (95% CI: 18.5, 21.4)] (Fig. 1). Moreover, the prevalence of PFD among women with grand multi gravida was 23.4% (95% CI: 21.6, 25.3) compared with women with gravida < 4 [15.8% (95% CI: 13.9, 17.9)] (Fig. 2).
After controlling for confounding factors, the prevalence of PFD was 47% higher (APR = 1.47; 95% CI: 1.06, 2.04) among uneducated women compared with women who had some education. The prevalence of PFD was 56% higher (APR = 1.56; 95% CI: 1.18, 2.05) among women who delivered five or more children vaginally compared with women who delivered four and fewer children vaginally. Having a history of abortion was associated with having PFD compared with no history of abortion (APR = 1.85; 95% CI: 1.43, 2.38). Having a history of episiotomy was significantly associated with PFD (APR = 1.39; 95% CI: 1.02, 1.90) (Table 1).
Discussion
Illiteracy, having had five or more vaginal deliveries, an abortion and episiotomy were found to be factors independently associated with pelvic floor disorder. The prevalence of PFDs was significantly higher among uneducated than educated women. Uneducated women might be forced to marry early, engage in heavy labor (like farming), have a large number of children and return to work shortly after delivery. Such women may be less aware of preventive measures to maintain their well-being and become vulnerable to PFDs [8, 22]. This finding is in accordance with previous studies [10, 13].
Repeated vaginal childbirths pose a continuous strain on the pelvic floor muscles, which in turn results in weakening and damaging of the pelvic floor. Excessive strain and stretching of the muscles related to the delivery of the fetal head can result in damage of the levator ani muscle and nerve, thereby disrupting the motor signaling and possibly leading to laxity of the pelvic muscle [1]. This explains the observed association between PFD and five or more vaginal deliveries in this study.
In countries where the fertility rate is high and vaginal delivery is common, the probability of PFD affecting women’s general health and social life is inevitable. Primary and secondary prevention strategies include fertility reduction through contraception, the mode and management of delivery, providing pelvic muscle exercises and advising women during pregnancy. These steps have played a major role in reducing the burden of PFD related to vaginal multiparity. This finding is in agreement with previous related reports [10, 19, 23].
Women who had a history of abortion were reported to have a significantly higher prevalence of PFD compared with women who had no history of abortion. The mechanism by which abortion contributes to PFD is not clear. In developing countries, abortion is often conducted in a clandestine environment where aseptic techniques and the qualifications of the performer are a concern. Thus, its consequences may contribute to PFD. This finding is also supported by other studies [24, 25].
Furthermore, episiotomy was found to be a risk factor for PFDs. It is usually performed to prevent spontaneous tears and ease the fetal delivery. However, the association between episiotomy and PFDs remains controversial. Some studies reported no association [26, 27], while others reported protective effects against PFD [19, 28]. The variation in the effect of episiotomy among studies may have arisen from the differences in the episiotomy prevalence and procedures. Mediolateral episiotomy is regarded as more protective than median episiotomy [29]. Episiotomy has been shown to reduce perineal muscle strength because of extensive tissue separation in the postpartum period [30].
A limitation of this study is that a cross-sectional study design may prove an association but not causality. The self-reported nature of the questionnaire meant that recall and reporting bias was inevitable. Furthermore, we did not perform pelvic examinations since that would be unacceptable during a household survey, and it is possible that mild cases were missed because of under-reporting. In addition, women may have under-reported symptoms because of social stigma and shame. Thus, the prevalence of PFD reported in this study could be an underestimate of the true magnitude. Finally, it was not possible to assess the effect of the length of the second stage of labor on pelvic floor disorders as it is difficult to determine prolonged labor from uneducated respondents.
The main strengths of this study include the high response rate and large representative sample size from a community-based survey. This study was conducted in an established Health and Demographic Surveillance System location, which provided a robust platform to randomly select participants. Furthermore, data collectors and supervisors were well trained, all questionnaire items were clearly stated, and quality control of the interviews ensured the validity and completeness of the results. Thus, the findings provide a reasonable estimate of the magnitude of PFDs and can be generalized to a large segment of the rural agrarian women in Ethiopia.
Conclusions
Five or more vaginal deliveries, illiteracy, a history of abortion and episiotomy were modifiable independent factors associated with pelvic floor disorder. This finding highlights the greater need for policies to focus on prevention strategies, such as a reduction of the number of pregnancies through contraception, improved safe delivery services and educating women about pelvic floor exercises to prevent PFD.
References
Milsom I. Can we predict and prevent pelvic floor dysfunction? Int Urogynecol J. 2015;26:1719–23.
Trutnovsky G, Kamisan Atan I, Ulrich D, Martin A, Dietz HP. Levator ani trauma and pelvic organ prolapse—a comparison of three translabial ultrasound scoring systems. Acta Obstet Gynecol Scand. 2016;95(12):1411–7.
Loubeyre P, Copercini M, Petignat P, Dubuisson JB (2012) Levator ani muscle complex: anatomic findings in nulliparous patients at thin-section MR imaging with double opacification. Radiology 262(1). https://doi.org/10.1148/radiol.11111014/-/DC1.
Vergeldt TFM, Weemhoff M, IntHout J, Kluivers KB. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J. 2015;26:1559–73.
Dieter AA, Wilkins MF, Wu JM. Epidemiological trends and future care needs for pelvic floor disorders. Curr Opin Obstet Gynecol. 2015;27(5):380–4.
Dietz HP. Pelvic floor trauma in childbirth. Aust N Z J Obstet Gynaecol. 2013;53(3):220–30. https://doi.org/10.1111/ajo.12059.
Giraudet G, Patrouix L, Fontaine C, Demondion X, Cosson M, Rubod C. Three dimensional model of the female perineum and pelvic floor muscles. Eur J Obstet Gynecol Reprod Biol. 2018;226:1–6. https://doi.org/10.1016/j.ejogrb.2018.05.011.
Islam RM, Bell RJ, Billah B, Hossain MB, Davis SR. The prevalence of symptomatic pelvic floor disorders in women in Bangladesh. Climacteric. 2016. https://doi.org/10.1080/13697137.2016.1240771.
Central Statistical Agency. Ethiopian demographic Health Sruvillance. 2016. https://www.usaid.gov/sites/default/files/documents/1860/Ethiopia%20DHS%202016%20KIR%20-%20Final%2010-17-2016.pdf. Accessed 5 Dec 2016.
Akter F, Gartoulla P, Oldroyd J, RM I. Prevalence of, and risk factors for, symptomatic pelvic organ prolapse in rural Bangladesh: a cross-sectional survey study. Int Urogynecol J. 2016;27(11):1753–9.
Berger MB, DeLancey JO, Fenner DE. Racial differences in fecal incontinence in community-dwelling women from the EPI study. Female Pelvic Med Reconstr Surg. 2013;19(3):169–74. https://doi.org/10.1097/SPV.0b013e3182874709.
Uganda Bureau of Statistics, ICF. Uganda demographic and health survey. 2018. https://dhsprogram.com/pubs/pdf/FR333/FR333.pdf. Accesed 26 May 2018.
Asresie A, Admassu E, Setegn T. Determinants of pelvic organ prolapse among gynecologic patients in Bahir Dar, north West Ethiopia: a case–control study. Int J Womens Health. 2016;8:713–9.
Gjerde JL, Rortveit G, Muleta M, Adefris M, Blystad A. Living with pelvic organ prolapse: voices of women from Amhara region, Ethiopia. Int Urogynecol J. 2017;28(3):361–6. https://doi.org/10.1007/s00192-016-3077-6.
Assefa N, Oljira L, Baraki N, Demena M, Zelalem D, Ashenafi W, et al. HDSS profile: the Kersa health and demographic surveillance system. Int J Epidemiol. 2016;45(1):94–101. https://doi.org/10.1093/ije/dyv284.
Dheresa M, Worku A, Oljira L, Mengiste B, Assefa N, Berhane Y. One in five women suffer from pelvic floor disorders in Kersa district Eastern Ethiopia: a community-based study. BMC Womens Health. 2018;18(95). https://doi.org/10.1186/s12905-018-0585-1.
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–6. https://doi.org/10.1001/jama.300.11.1311.
Haylen BT, Dd R, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26. https://doi.org/10.1007/s00192-009-0976-9.
Gyhagen M, Åkervall S, Milsom I. Clustering of pelvic floor disorders 20 years after one vaginal or one cesarean birth. Int Urogynecol J. 2015;26:1115–21.
Lukacz ES, Lawrence JM, Buckwalter JG, Burchette RJ, Nager CW, Luber KM. Epidemiology of prolapse and incontinence questionnaire: validation of a new epidemiologic survey. Int Urogynecol J. 2005;16:272–84.
Bongard S, Al'Absi M, Khalil NS, Al Habori M. Khat use and trait anger: effects on affect regulation during an acute stressful challenge. Eur Addict Res. 2011;17(6):285–91. https://doi.org/10.1159/000330317.
Walker GJA, Gunasekera P. Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J. 2011; 22(127–135).
Gyhagen M, Bullarbo M, Nielsen T, Milsom I. The prevalence of urinary incontinence 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG. 2013;120:144–51.
Ge J, Yang P, Zhang Y, Li X, Wang Q, Lu Y. Prevalence and risk factors of urinary incontinence in Chinese women: a population-based study. Asia Pac J Public Health. 2015;27(2):1118–31. https://doi.org/10.1177/1010539511429370.
Gjerde JL, Rortveit G, Muleta M, Blystad A. Silently waiting to heal; experiences among women living with urinary incontinence in Northwest Ethiopia. Int Urogynecol J. 2013;24:953–8.
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I. Faecal incontinence 20 years after one birth: a comparison between vaginal delivery and caesarean section. Int Urogynecol J. 2014. https://doi.org/10.1007/s00192-014-2390-1.
Kılıç M. Incidence and risk factors of urinary incontinence in women visiting Family Health Centers. Springerplus. 2016; 5(1331). https://doi.org/10.1186/s40064-016-2965-z.
Liu B, Wang L, Huang SS, Wu Q, Wu DL. Prevalence and risk factors of urinary incontinence among Chinese women in Shanghai. Int J Clin Exp Med. 2014;7(3):686–96.
Handa VL, Blomquist JL, McDermott KC, Friedman S, Mun A. Pelvic floor disorders after vaginal birth effect of episiotomy, perineal laceration, and operative birth. Obstet Gynecol. 2012;119:233–9.
Bozkurt M, Yumru AE, Sahin L. Pelvic floor dysfunction, and effects of pregnancy and mode of delivery on pelvic floor. Taiwan J Obstet Gynecol. 2014;53:452–8.
Acknowledgements
We acknowledged Haramaya University and Addis Continental Institute of Public Health for their technical and financial support. We are thankful to the women who responded to this survey.
Funding
This study was financially supported by Haramaya University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Dheresa, M., Worku, A., Oljira, L. et al. Factors associated with pelvic floor disorders in Kersa District, eastern Ethiopia: a community-based study. Int Urogynecol J 30, 1559–1564 (2019). https://doi.org/10.1007/s00192-018-3776-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3776-2