Abstract
Background
Studies conducted in orthopedic surgery have suggested that patients with anxiety have less symptomatic improvement following surgery than those without. We hypothesized for this study that patients with anxiety traits experience less symptomatic improvement following pelvic organ prolapse surgery than patients without.
Methods
All patients presenting for prolapse repair surgery were offered enrollment in this prospective cohort study. Prior to surgery, subjects were asked to complete the Spielberger State-Trait Anxiety Inventory and the Pelvic Floor Distress Inventory 20. Subjects were also asked to list up to five goals related to the outcome of surgery for goal-attainment scaling. At the 6–8-week postoperative visit, subjects were asked to repeat the STAI and PFDI questionnaires and respond to the single question tool assessing Patient Global Impression of Improvement. Subjects were also asked to rate on a Visual Assessment Scale how well preoperative goals were met. All three questionnaires were repeated at >12 weeks following surgery.
Results
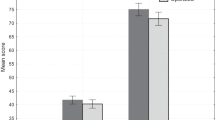
A total of 32 patients with anxiety trait and 58 without were recruited. Preoperatively, the mean STAI-T was 45.0 (± 7.2.) and 27.7 (± 4.9) for subjects with and without anxiety; PFDI 20 scores were 96.1 (± 48.8) and 94.7 (± 57.5), respectively. At 12+ weeks postoperatively, the mean PFDI-20 for subjects with anxiety was 31.3 (± 20.9) and 30.3 (± 27.9) (p = 0.22) for those without.
Conclusions
We did not find the anxiety trait to be a predictor of subjective outcomes following pelvic organ prolapse surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Women with pelvic floor disorders have high rates of anxiety and depression. This finding is frequently attributed to the emotional burden of pelvic organ prolapse and/or incontinence [1]. It is unclear, however, how the relationship between anxiety and pelvic floor symptoms affects the outcome of corrective pelvic floor surgery.
It has been suggested that women with anxiety or depression may be more bothered by their pelvic floor symptoms than their non-anxious peers [2,3,4]. Studies based on quality-of-life measures have shown worse quality-of-life scores related to incontinence in women with co-existing depression than in their non-depressed peers [2,3,4]. While pelvic floor disorders have a clear emotional burden, it is possible that mental health disorders may play a role in the development of or the symptom burden from pelvic floor disorders.
In addition, we must consider the effect mental health disorders may have on treatment outcomes. Multiple studies have shown that anxiety is a predictor of lower treatment outcome scores in a broad range of conditions [5,6,7,8]. For example, following orthopedic surgery, patients with preoperative anxiety have been found to have less symptomatic improvement and are less satisfied with the outcome of their surgery [5, 6]. Further, perioperative anxiety is associated with higher postoperative pain scores following elective surgery [7]. Regarding pelvic floor disorders, women with anxiety have been found to experience less improvement of pelvic floor symptoms with physical therapy compared with women without anxiety [8].
Based on these findings, we hypothesized that women with anxiety will have less symptomatic improvement of pelvic floor symptoms following surgery for pelvic organ prolapse than women without anxiety.
Materials and methods
This is a prospective cohort study conducted over a 2-year period. Approval was obtained from the Institutional Review Board of the University of Rochester. Patients planning to undergo surgical repair of pelvic organ prolapse were approached for enrollment in the study. To be included in this study, women had to be English-speaking, over 18 years old and planning to undergo surgery for pelvic organ prolapse. Women were approached for enrollment after surgery was scheduled and after completing the informed consent process for the surgery. Women with previously diagnosed dementia, visual impairment, or the inability to answer questionnaires were excluded.
At the time of enrollment, all subjects were screened for anxiety using the validated Spielberger State Trait Anxiety Inventory (STAI). The STAI includes domains for “state” and “trait” anxiety to characterize current and long-standing anxiety; the domains are validated to be used independently [9]. Due to the concern that anxiety regarding upcoming surgery may bias our cohort, we used only the trait domain, which is scored on a range from 20 to 80 with higher values corresponding to higher anxiety traits. Subjects with an STAI-T score > 38 (the median quartile for moderate anxiety from prior validation studies) were classified with anxiety trait. In addition, subjective symptom burden was assessed using the PFDI-20 including the Pelvic Organ Prolapse Distress Inventory (POPDI). The PFDI-20 is scored on a range from 0 to 300, with higher scores corresponding to higher symptom burden [10]. Preoperatively, pelvic organ prolapse was quantified using the Pelvic Organ Prolapse Quantification System (POP-Q) staging system [11]. All POP-Q measurements were taken by fellowship-trained urogynecologists. Measurements were recorded to the nearest 0.5 cm. In addition to POP-Q stage, the leading edge was used as a marker for prolapse extent. The leading edge was defined as the most dependent portion of the prolapse (in the anterior, posterior or apical compartments).
In addition to symptom distress, we used patient-reported satisfaction as a secondary measure. Prior to enrollment, all subjects underwent preoperative counseling with the primary attending surgeon regarding the risks and benefits of surgery, anticipated outcomes and alternatives to surgery including expectant management, pessary use and pelvic floor physical therapy. After enrollment, subjects were asked to list up to five personal goals for surgery. We categorized subjects’ listed goals into one of four categories: physical activity, social activities, sexual function and symptom relief. Goal categories were chosen based on previous studies using goal attainment as an outcome [12, 13]. Examples of goals from each category are provided in Table 1.
A second researcher reviewed categorization of goals by comparing the subjects’ verbatim goals to the assigned category.
Subjects were asked to complete STAI and PFDI questionnaires again at their 4–8 week follow-up visit. Additionally, subjects were given the list of their verbatim goals obtained at the preoperative visit and were asked to indicate on a visual analog scale how well each goal was met.
Subjects were further asked to respond to the single-question “Patient Global Impression of Improvement questionnaire”:
How would you describe your overall pelvic floor condition now compared to what it was before surgery? |
Very much better |
Much better |
A little better |
No change |
A little worse |
Much worse |
Very much worse |
All four questionnaires (PFDI-20, STAI, VAS and PGI-I) were repeated at a minimum of 12 weeks after surgery. These questionnaires were mailed to subjects. Those subjects who did not respond to the mailed questionnaires were contacted by phone and were offered to respond to email questionnaires.
The primary outcome of this study was postoperative PFDI-20 score improvement at 6 weeks. Secondary outcomes included postoperative improvement at 12 weeks, patient satisfaction as measured on PGI-I and goal attainment as measured by visual assessment scale. While the VAS is not validated for measuring symptom burden or outcomes, it has previously been shown to be a useful outcome measure when used for goal scaling and measuring goal attainment [8, 9]. The mean VAS for all goals provided by each subject was used as the outcome measure for goal attainment.
STATA IC 13.1 was used for data analysis. A power calculation was performed prior to patient recruitment. Based on previous studies using the PFDI-20, we assumed a 45-point difference in the PFDI score to be clinically relevant. Previously reported mean (SD) PFDI scores are 121.6 (48.2) [10]. For 80% power to detect a difference and α = 0.05, we estimated that a minimum of 20 subjects would be needed in each arm. To account for potential drop-out and under-recruitment of patients with anxiety, we planned to enroll 100 subjects. Because subjects were only screened for anxiety after recruitment, we planned to recruit 100 subjects in anticipation of an anxiety prevalence of 15–20% [14].
Skewness-kurtosis testing was used to test for normal distribution of all variables. For variables approximating a normal distribution, two-sample t-test was used to compare outcomes. PGI-I outcomes were not normally distributed, and a Mann-Whitney U test was used to compare across groups.
Results
A total of 100 subjects were recruited. Twenty patients were approached for enrollment and declined. Five subjects withdrew from the study: two of the subjects felt too anxious about their upcoming surgery to answer further questions. One subject was withdrawn because she did not understand the STAI questionnaires. The remaining two subjects did not give reasons for withdrawing. Five subjects canceled their surgery after being assigned to a cohort, four of which were from the anxiety cohort. The mean follow-up was 6 months. After removing withdrawn subjects, a total of 32 subjects with anxiety and 58 without were assessed. A total of 90 surgeries were performed: 58 subjects (23 anxious and 35 non-anxious) underwent vaginal prolapse repair surgery including vaginal hysterectomy, uterosacral ligament suspension, sacrospinous ligament suspension, and anterior and posterior colporrhaphy. Twenty-one subjects (3 anxious and 18 non-anxious) underwent abdominal sacrocolpopexy; 11 subjects (5 anxious and 6 non-anxious) underwent vaginal obliterative surgery including vaginectomy with colpocleisis and LeFort colpocleisis. In addition to prolapse repair surgery, 11 subjects (3 anxious and 8 non-anxious) also underwent anti-incontinence procedures (TVT). Six- to 8-week data were collected on 80 subjects; 12-week data were collected on 61 subjects (24 anxious and 37 non-anxious). As anticipated, mean STAI scores did not significantly change postoperatively for the state or trait domains in either cohort.
Demographic information is displayed in Table 2 for the entire study population. Table 3 displays the demographic information for each cohort. There was no difference in age, smoking, postmenopausal status or prior hysterectomy or prolapse surgery among the cohorts. There were no current smokers in either group. Anxious-trait subjects were more likely to have previous diagnoses of depression or anxiety; no other baseline demographic differences were observed. All subjects with a diagnosis of anxiety met criteria for anxiety trait by STAI scores.
There was no measured difference in the cohorts regarding PFDI or POPDI symptom scores or in prolapse stage as measured by leading edge. Table 4 displays the preoperative symptom bother (PFDI and POPDI), anxiety (STAI) score and prolapse leading edge for both cohorts.
There was also no difference in the number of goals or the distribution of goal categories for anxiety trait and non-anxiety trait subjects. The most common goals listed were categorized under symptom relief followed by physical activity. Table 5 displays a summary of the 342 goals listed by subjects.
There was no difference in mean postoperative PFDI scores or in goal attainment outcomes as measured by VAS reported by subjects in either cohort. Table 6 displays postoperative subjective outcomes for both cohorts, at 4–8 weeks and at 12 + weeks. Mean STAI scores did not significantly change postoperatively for either the state or trait domains (p = 0.11 and 0.96, respectively). In light of our negative results, we performed simple linear regression analysis using PFDI-20 scores as well as mean VAS scores on the complete sample to evaluate for any potential correlation. No statistically significant correlations were identified using linear regression. We therefore rejected our study hypothesis.
Discussion
Our study had several interesting findings. Most notably, anxiety trait patients had similar subjective outcomes as their non-anxiety trait peers. Further, anxiety did not appear to play a role in their subjective goal attainment and symptom improvement.
These results were unexpected in light of several prior studies evaluating emotional health and pelvic floor disorders [1,2,3,4, 10]. Pizarro and coworkers evaluated PFDI symptoms in subjects with and without depression. Although their cohorts had similar prolapse staging by objective criteria, depressed subjects had higher symptom bother scores on PFDI. Watson and coworkers performed a prospective study evaluating urinary incontinence symptoms in anxious and non-anxious women using both subjective complaints and objective pad weights. Women with anxiety had significantly lower pad weights compared with non-anxious women with the same subjective level of symptom bother, suggesting that women with anxiety may be bothered at a lower level of incontinence [2].Anxiety trait subjects and non-anxiety trait controls in our study had no difference in symptom scores or in prolapse staging. One explanation for this may be that the impact of anxiety on incontinence symptoms as reported in multiple studies is more pronounced than the impact of anxiety on prolapse symptoms. Additionally, different scales used in different studies may create a confounding effect. This study uses the PFDI, which differs from some of the other previous studies, which used the PFIQ and Queensland Pelvic Floor Questionnaire. Additional research is needed to determine if PFIQ scores differ or correspond differently to outcomes. Additionally, we used the STAI to measure anxiety while other studies have used other measures including the HAD, GAD and clinical diagnosis.
In addition, most of the subjects with anxiety trait in this study had mild-to-moderate anxiety, which may have less of an effect on subjective outcome than severe anxiety. Approximately 12/20 subjects declining study participation had been pre-diagnosed with anxiety and more, than half of the patients who canceled surgery were in the anxiety trait cohort, which may have biased our study to include subjects with a lesser degree of anxiety. Therefore, it is possible that the number of subjects with severe anxiety symptoms was too low to detect a different outcome in patients with severe symptoms of anxiety. Thus, we can only conclude that patients with mild anxiety trait are similar to patients without anxiety.
Our negative findings regarding lower satisfaction with surgical outcome in women with anxiety may also be related to our emphasis on patient-selected goals. Since we were using self-selected goals chosen by the subjects rather than externally defined or vague goals, subjects may have felt higher satisfaction regarding improvement of their symptoms. By choosing a specific goal such as “to reduce the rubbing” instead of a vague goal such as “to fix the prolapse,” subjects had a clear measurement of improvement.
The strength of this study is the use of patient-reported outcomes and patient-selected goals. We recognize the short follow-up period, low number of subjects with severe anxiety and limited demographic diversity as a weakness of this study. The fact that there were no smokers in either cohort suggests the possibility of selection bias, as tobacco use is highly concurrent with anxiety disorders. Tobacco use is not a contraindication for surgery at our center. However, we do encourage cessation for smokers, especially when considering surgery. We did not obtain anatomic data at time of intermediate follow-up (3–6 months). However, the focus of this study was on subjective improvement and patient-reported outcomes; the absence of physical examination findings is not a weakness, since it is unlikely that women with anxiety are any more or less likely to experience an anatomic recurrence. Additionally, inclusion of patients with multiple surgeries (vaginal reconstructive surgery, obliterative surgery, sacrocolpopexy) as well as the inclusion of subjects undergoing continence repair may be creating disparities in patient goals (for example, sexual function goals for subjects undergoing colpocleisis will be very different from those undergoing sacrocolpopexy).
An incidental finding of this study was that more than half of the patients who canceled surgery were in the anxiety trait cohort, which was higher than anticipated. Future research could evaluate if patients with anxiety are more or less likely to opt for non-surgical options such as expectant management or pessary. This information could be valuable when considering treatment counseling. Additionally, we know very little about whether or how anxiety affects routes of surgery when multiple options are available. Anxious patients may desire a repair with a higher success rate if they are concerned about recurrence, or they may desire a repair with a lower risk of complications if their concern is with complications from surgery. The surgical choice is ultimately the patient’s, and knowledge of the patient’s preferences can be extremely useful when assessing patient satisfaction.
Based on the previously mentioned orthopedic studies, we had anticipated subjects with anxiety trait to feel less symptomatic improvement following surgery. That this was not the case might be useful during surgical counseling with anxious patients. Some providers may even be less inclined to offer surgery to patients with anxiety as the potential risks may not be justified if patients did not feel any substantial improvement. Our findings, however, that patients with anxiety trait experience significant symptom relief following surgery and can continue to be counseled as such are reassuring. Equally important is our finding of the potential relevance of patient-selected goals. During preoperative counseling, we now discuss the individual goals with all of our patients. Not only does it provide an opportunity to recognize unrealistic goals, it also serves as an indicator for surgical success and outcomes. Considering the increasing importance of patient-related outcomes in healthcare, a clear definition of expectations for surgical outcome is critical.
References
Molinuevo B, Batista-Miranda JE. Under the tip of the iceberg: psychological factor in incontinence. Neurourol Urodyn. 2012;31(5):669–71.
Watson AJ, Currie I, Curran S, Jarvis GJ. A prospective study examining the association between the symptoms of anxiety and depression and severity of urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 2000;88(1):7–9.
Melville JL, Walker E, Katon W, Lentz G, Miller J, Fenner D. Prevalence of comorbid psychiatric illness and its impact on symptom perception, quality of life and functional status in women with urinary incontinence. Am J Obstet Gynecol. 2002;187(1):80–7.
Felde G, Ebbesen MH, Hunskaar S. Anxiety and depression associated with urinary incontinence. A 10-year follow-up study from the Norwegian HUNT study (EPINCONT). Neurourol Urodyn. 2017;36:322–8.
Hanusch BC, O’Connor DB, Ions P, Scott A, Gregg PJ. Effects of psychological distress and perceptions of illness on recovery from total knee replacement. Bone Joint J. 2014;96-B(2):210–6.
Blackburn J, Qureshi A, Amirfeyz R, Bannister G. Does preoperative anxiety and depression predict satisfaction after total knee replacement? Knee. 2012;19(5):522–4.
Katz J, Poleschuck EL, Andrus CH, Hogan LA, et al. Risk factors for acute pain and its persistence following breast cancer surgery. Pain. 2005;119(1–2):16–25.
Khan ZA, Whittal C, Mansol S, Osborne LA, Reed P, Emery S. Effect of depression and anxiety on the success of pelvic floor muscle training for pelvic floor dysfunction. J Obstet Gynaeol. 2013;33(7):710–4.
Spielberger CDGR, Lushene R, Vagg PR, Jacobs GA. Manual for the state-trait anxiety inventory. Palo Alto, AC: Consulting Psychologist Press; 1983.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13.
Bump RC, Mattiasson A, Bo K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7.
Srikrishna S, Robinson D, Cardozo L. A longitudinal study of patient and surgeon goal achievement 2 years after surgery following pelvic floor dysfunction surgery. BJOG. 2010;117(12):1504–11.
Elkadry EA, Kenton KS, Fitzgerald MP, Shott S, Brubaker L. Patient-selected goals: a new perspective on surgical outcome. Am J Obstet Gynecol. 2003;189(6):1551–7.
Vrijens DBerghmans B, Nieman F, Van Os J, van Koeveringe G, Leue C. Prevalence of anxiety and depressive symptoms and their association with pelvic floor dysfunctions – a cross sectional cohort study at a pelvic care center. Neurourol Urodyn. 2017;36(7):1816–23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Collins, A.F., Doyle, P.J., Duecy, E.E. et al. Do anxiety traits predict subjective short-term outcomes following prolapse repair surgery?. Int Urogynecol J 30, 417–421 (2019). https://doi.org/10.1007/s00192-018-3734-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3734-z