Abstract
Introduction and hypothesis
An adequate pelvic floor muscle contraction (PFMC) elevates the bladder neck (BN) and stabilizes it during increased intra-abdominal pressure (IAP). A maximal PFMC may increase the IAP and thereby prevent BN elevation. The aim of this study was to assess BN elevation during submaximal and maximal PFMC and their achievable duration.
Methods
We recruited 68 women with stress urinary incontinence and 14 vaginally nulliparous continent controls who were able to perform a PFMC on vaginal palpation. Women were upright and performed a maximal PFMC as long as possible, followed by a submaximal PFMC, controlled by vaginal electromyogram (EMG). BN position was measured with perineal ultrasound, IAP and urethral pressure with a microtip catheter, and breathing with a circular thorax sensor.
Results
A submaximal PFMC elevated the bladder neck 4 mm in continent and incontinent women (p = 0.655) and 4.5 vs. 5 mm during maximal PFMC (0.528). Submaximal PFMC was maintained significantly longer than a maximal PFMC (33 vs 12 s) with no difference between groups. A maximal PFMC resulted in BN descent in 29% of continent and 28% of incontinent women, which was not observed during submaximal PFMC. Breathing was normal in 70% of continent and 71% of incontinent women during submaximal PFMC but stopped completely in 21 and 50%, respectively, during maximal PFMC (p = 0.011). IAP increase was significantly greater with maximal PFMC in both groups (24 vs. 9.6 cmH2O and 17 vs. 9 cmH2O, respectively).
Conclusion
Submaximal PFMC are sufficient to elevate the bladder neck, can be maintained longer, and breathing was not influenced.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic floor muscle training (PFMT) represents the mainstay of conservative treatment of urinary incontinence (UI) in women and is recommended as first-line treatment in many practice guidelines for UI and pelvic organ prolapse (POP) [1,2,3]. A prerequisite of successful PFMT is a correct pelvic floor muscle contraction (PFMC) that leads to elevation of the bladder neck (BN), which can be imaged with perineal pelvic floor ultrasound (PFU). In contrast, increased intra-abdominal pressure (IAP) during coughing or straining results in sonographically demonstrable BN descent [4,5,6] if a pelvic floor precontraction does not prevent this [6, 7]. Easy access, application, and comprehension of perineal PFU render it an excellent assessment and teaching tool. It can also serve as a visual biofeedback tool to teach women the effect of a PFMC [8].
In a study using PFU, it was shown that BN elevation during PFMC might be inhibited by an increased IAP generated by an increase in abdominal muscle activity, especially that of the internal oblique muscle [9]. As many PFM training programs teach maximal PFMC during exercise classes, including abdominal, hip, and low-back muscles, an excessively increased IAP resulting in loss of BN support [10] might be one component to preclude a successful outcome. The physiological muscle reaction to an increasing IAP would be an eccentric contraction that stabilizes urethra and BN during a cough [11]. However, muscle relaxation has been described during coughing in incontinent women [12], which would compromise BN support. Theoretically, a submaximal PFMC may also support the BN, with the possible advantage of a longer contraction, which would be helpful in urgency situations until reaching the toilet and may be a valuable aspect in pelvic floor re-education and fitness classes.
Our research group assessed BN elevation dependent on the strength of a PFMC in continent and incontinent women and presented data at the International Urogynecological Association (IUGA) meeting in 2008 [13]. We found that BN elevation does not linearly increase with increasing PFMC intensity (Fig. 1) and that a perceived effort of only 25% of a maximal PFMC led to a significant elevation in most women. At ~50% of maximal PFMC strength, the BN was elevated sufficiently, especially in relation to the nearly exponentially increasing IAP. The IAP was as high as that produced by a moderate cough in many women, which seems to contradict the aim of a PFMC to elevate the BN. This study was criticized because we used a woman’s subjective estimation only to assess the level of PFMC effort using electromyelographic (EMG) confirmation. Furthermore, data were obtained with women placed in the supine position. It therefore remained unclear how long a maximal PFMC could be maintained in contrast to submaximal PFMC.
Results of perceived pelvic floor muscle contractions (PFMC) with different intensities [13]. Black intra-abdominal pressure (cmH2O), gray bladder-neck movement (mm), dashed lines patients, solid lines healthy women
The aim of this study was to assess BN position during EMG-controlled submaximal and maximal PFMC and their achievable effective duration in continent and incontinent women in the standing position. We sought to assess the effects of submaximal and maximal PFMC on BN position, IAP, breathing, and PFMC duration with adequate BN support. We hypothesized that submaximal PFMC is sufficient to elevate the BN and can be maintained longer.
Methods
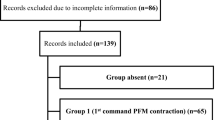
We recruited 68 consecutive women with dominant stress urinary incontinence (SUI) who were invited to take part in a randomized controlled trial comparing different pelvic floor rehabilitation regimes (clinical trial registration DRKS00004218). Fourteen continent women who had had no vaginal deliveries were recruited via advertisements and served as the healthy control group. All women completed a validated pelvic floor questionnaire (German version of the Australian Pelvic Floor Questionnaire) [14] and underwent Pelvic Organ Prolapse Quantification (POPQ) staging [15]. Both assessments were performed as a screening tool to include women with SUI with or without overactive bladder and to exclude women with prolapse beyond the hymenal remnants. The ability to perform a PFMC was checked by vaginal palpation. Exclusion criteria were age <18 years, inability to contract PFM, previous pelvic floor surgery, and POP beyond the hymen. The local Ethics Committee approved the study (EA1/297/10), and all women gave written informed consent.
A surface PFM-EMG electrode attached to a sponge (Disposable Vaginal Surface Electrode, Mediwatch, UK) was placed in the vagina at the level of the puborectalis muscle (PRM) to evaluate PFM activity and ensure that the submaximal PFMC was about half of maximal. In case of levator avulsion, the electrode was positioned higher, at the level of the pubo- or iliococcygeus muscle, or on the other side. No woman had complete loss of pelvic floor musculature strength. The sponge was soaked with lubricating gel and minimized in size to reduce interference with PFU.
BN and PRM position was assessed using perineal US. A curved-array (abdominal) probe (5 MHz, Voluson E8, GE) was placed on the perineum, with the cable vertical and the women in the standing position. A dual Microtip catheter (10 Ch) was inserted urethrally to measure the vesical/abdominal and urethral pressures [16, 17]. The transducers to measure the pressure in the urethra were placed at 3- or 9-o’clock positions, as recommended [18]. The location of the maximum urethral pressure was identified during a resting urethral pressure profile. The catheter was taped to the thigh at this position. A surface EMG electrode to record predominantly the external and internal obliquus muscles was placed just medial to the upper anterior iliac spine after cleaning the skin with an alcohol pad.
To monitor breathing, a sensor (Sleep Sense, S.L.P. Inc., USA) detecting stretching was placed around the thorax. Figure 2 shows the setting.
With a comfortably full bladder, between 150 and 300 ml, women were asked to stand relaxed and perform a maximal PFMC and maintain it as long as possible. After an appropriate rest, women were asked to perform a perceived submaximal PFMC at ~50% of their maximal and hold it for as long as they could. Women were not allowed to observe the measurement screen, thus avoiding visual feedback. Measurements were stopped when PFM-EMG decreased by ~50% or BN support was lost on perineal US.
IAP, EMG, breathing measurements, and US videos were recorded on one screen with one timeline and stored for later analyses using the software Tele Myo, Human Performance Measurements Solutions MR 3.0 (Noraxon, USA Inc.). Given the nature of the tasks it was not possible to blind the analyst regarding the task but regarding continence status. Position and height of the BN and PRM behind the rectum were measured from a horizontal line using the dorsal edge of the pubic symphysis as the reference point, as recommended by Dietz et al. [19]. The Noraxon software track points of interest (BN position and PRM) on-screen. This system is similar to the validated vector-based system [20] and allows correction of visible shifting of the probe in relation to the pubic bone during tasks, as described by Reddy et al. [20]. A ventrocranial displacement of the BN and PRM was considered a positive vector (BN elevation), whereas a dorsocaudal displacement was described as a negative vector (BN descent) [21,22,23]. EMG signals were filtered using a band pass between 30 and 1000 Hz [24]. To compare EMG amplitudes during maximal and submaximal PFMC, root mean squares (RMS) were computed over a period of 500 ms. Loss of BN support on perineal US was defined as visible BN descent of at least 3 mm (minimal detectable change) [25]. We considered a difference of 20 s between maximal and submaximal PFMC as clinically significant and calculated that ten women are necessary with a power of 80% and α = 0.05 [two-sided, one-sample test, standard deviation (SD) 30 s]. To compare nonnormally distributed variables, we performed the nonparametric Wilcoxon test; for between-groups differences, the Mann–Whitney U test was used. SPSS 21 was employed.
Results
Incontinent women were a median age of 47 years (28–77), median BMI 24 (18-50), and parity ranged from 0 to 8 (median 1). Continent women were significantly younger (median 31 years, range 21–52; p < 0.001) and had a lower BMI (23, range 18–27). Parity was similar (median 1.5, range 0–3), although continent women had only cesarean sections. BN position at rest was significantly lower in incontinent women (1.9 vs 2.4 mm; p = 0.001). With a submaximal PFMC, it was significantly elevated to a median of 2.2 and 2.75 mm in continent and incontinent women, respectively (p < 0.001 for both groups, p = 0.005 between groups). During a maximal PFMC, BN height was marginally higher at 2.3 and 2.9 mm, respectively (fat rest, p = 0.008 and p < 0.001 in continent and incontinent women; p = 0.002 between groups). BN elevation (positive vector) was measured between 4 and 5 mm, showing no differences between continent and incontinent women or submaximal and maximal PFMC (Table 1).
A submaximal PFMC was maintained significantly longer than a maximal PFMC (33 vs 12 s; p < 0.001) in both continent and incontinent women, with no differences between groups (Table 1). During a maximal PFMC, the BN descended in 19/68 (28%) of incontinent women and in 4/14 (29%) controls. During submaximal PFMC, no BN descent was observed in either group. Breathing was irregular or stopped completely in 55 and 21% of incontinent and 36 and 50% of continent women during a maximal PFMC, respectively (p = 0.011). In contrast, during a submaximal PFMC, a normal breathing pattern was observed in 70 and 71% in continent and incontinent women, respectively (p = 0.4). Breathing patterns differed significantly between maximal and submaximal PFMC (p < 0.001). IAP and abdominal muscle EMG increased significantly more with a maximal vs. a submaximal PFMC in both groups, without differences between groups, and urethral closure pressure increased adequately during maximal and submaximal PFMC, also without a difference between groups (Table 1). Age, BMI, and parity did not correlate with BN and PRM movement. Figure 3 demonstrates an example of recordings of maximal and submaximal contractions.
Record of vesical/abdominal pressure (Pves), urethra pressure (Pura), pelvic floor (PFM) and abdominal (ABD) muscle electromyographic (EMG) activity and breathing pattern (Resp), as well as perineal ultrasound during maximal and submaximal PFM contraction (PFMC). Note the increase in intra-abdominal pressure and abdominal muscle activity simultaneously with a maximal PFMC (highest EMG values—dotted line) while breathing stops completely. During a submaximal PFMC, breathing appears regular and intra-abdominal pressure does not raise
Discussion
When both incontinent women and continent controls perform a submaximal PFMC, adequate BN elevation can be maintained twice as long as with a maximal PFMC, which lasted ~12 s in our study. A maximal PFMC resulted in a statistically and clinically significant increase in IAP due to undue activation of the abdominal muscles. Subsequently, BN descent was observed in nearly a third of continent and incontinent women. Also, normal breathing stopped in most women during maximal PFMC but rarely during a submaximal PFMC. These advantages of a submaximal PFMC should be helpful in PF rehabilitation to oppose prolonged IAP increases during repetitive coughing, walking stairs, or gardening and during urgency episodes.
Our previous data (Fig. 1) showed that the BN is not elevated linearly with increasing PFMC strength. To use BN elevation as a surrogate parameter for PFMC strength is therefore limited. In our current and previous study, the abdominal muscles were recruited more intensively with a maximal PFMC (Fig. 3 and Table 1), which also increased the IAP [9]. We know that an increased IAP during straining results in BN descent [26, 27]. This might counteract BN elevation and was exhibited clearly by 28% of incontinent women in whom the BN became depressed during maximal PFMC. The amount of maximal BN elevation nearly matched the 6.4 mm demonstrated by Peschers et al. [28]. Hypothetically, a submaximal 50% PFMC would lead to only a 3-mm elevation. This was already achieved with 25% of effort in our previous study (Fig. 1). A recent study showed that PRM movement highly correlated with PFM-EMG but that BN movement was more variable [29]. In agreement with our study, there was greater elevation of PRM on perineal US (PUS) than of the BN. In contrast to the directly assessed PFM action, the BN is only indirectly elevated by the endopelvic fascia and does not represent direct muscle action. Perineal US represents an excellent assessment tool with which to observe BN mobility and PFM function during coughing, straining, or PFMC [26, 30]. Women can be taught the different phases of PFM action during a contraction before IAP increases and how to maintain that contraction while expiring intensively during the cough. PFU can serve as a visual biofeedback instrument because women can easily follow instructions on the US screen. While we would encourage physiotherapists to use US during rehabilitation, it might not be essential. However, in a randomized controlled trial comparing selective activation of multifidi muscles during the motor-learning process in back pain, US implementation as a biofeedback tool was superior to explanation alone regarding selective activations [31].
BN support is an important factor in maintaining continence [6, 7, 26, 32]. Submaximal PFMC also elevates the BN and might be sufficient during coughing. Although incontinent women started with a lower BN position, they achieved a comparable BN elevation with continent women. Interestingly, the elevated BN position was similar to the resting position in continent women. Whether this BN position is sufficient to prevent urinary leakage during coughing in incontinent women remains open. Further studies will be necessary to prove the effectiveness of submaximal PFMC for treating UI.
Clinical implication
Submaximal PFMC significantly elevates the BN and can be maintained much longer without increasing IAP. High IAP might counteract BN elevation and lead to BN descent. Especially for women with OAB, it might be beneficial to practice submaximal PFMC so they have more time to reach the toilet without increasing pressure on the bladder and urethra. While we demonstrated that submaximal PFMC elevates the BN and can be held longer, it is not meant to substitute maximal PFMC with the intention to improve PFM strength and size. although formal PFM strength training did not seem to improve BN position at rest and during coughing in a study by Hung et al. [33].
Preactivation of PFM during coughing has been integrated into pelvic floor rehabilitation programs and is known as the “Knack” [34] . Sonographically, it was demonstrated that the BN descends less with a PF precontraction [4, 7]. Our data show that the BN can be sufficiently elevated with a submaximal PFMC, providing the advantages of not unduly increasing IAP and women’s ability to maintain it during breathing [9]. Continent and incontinent women demonstrated similar patterns, with no differences between groups. It appears encouraging that both continent and incontinent women can activate their PFM, resulting in similar effects on BN support between them.
Common urge strategies include performing five maximal PFMC [35]. Well-maintained submaximal PFMC might be more effective, which has to be proven in randomized controlled trials. In a follow-up study, we previously showed that 79% of women improved after PFM rehabilitation with advice to perform a submaximal PFMC as an urge strategy [8].
One aim of PF strength exercises is muscle hypertrophy [36], which results in a reduction in hiatal area when the PFM are at rest, most likely due to muscle thickness increase [37]. This might not be achieved with submaximal contractions. However, hypertrophy can only be maintained with regular life-long exercises with protocols following strength-training programs.
Strengths and limitations of the study
The strengths of this study include validated measurement and assessment tools in a physiological standing position. The digitalized assessment of BN and PRM on PFU was indispensable and had been validated previously [20]. The required sample size was reached in both continent and incontinent women. Furthermore, the person analyzing the measurements offline was blinded to continence status. PFMC strength was controlled by pelvic floor EMG. The study is limited by the lack of an age-, BMI-, and parity-matched control group. Also, selection of vaginally nulliparous controls resulted, ase expected, in a higher BN resting position [28]. Further limitations are that blinding the assessor to maximal or submaximal PFMC was impossible. It remains unclear how BN and PRM are influenced in women who cannot contract their PFM. IAP was measured intravesically to avoid insertion of a rectal line, and equal pressure distribution can be expected [38].
Concluding message
Submaximal PFMC significantly elevates the BN and can be maintained for more than twice as long as maximal PFMC. Maximal PFMC does not elevate the BN much further and has the disadvantage of considerably increasing the IAP. Especially in women with pelvic floor disorders, this might offset the initial functional BN elevation and result in increased urgency. Implementation of submaximal PFMC training might therefore be beneficial in incontinent women. Submaximal PFMC might not replace PFM strengthening programs if muscle power and augmentation is required to improve PF symptoms.
References
Dumoulin C, Hay-Smith EJ, Mac Habee-Seguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2014;5:CD005654. https://doi.org/10.1002/14651858.CD005654.pub3.
Baessler K, Aigmuller T, Albrich S, Anthuber C, Finas D, Fink T, et al. Diagnosis and therapy of female pelvic organ prolapse. Guideline of the DGGG, SGGG and OEGGG (S2e-level, AWMF registry number 015/006, April 2016). Geburtshilfe Frauenheilkd. 2016;76(12):1287–301. https://doi.org/10.1055/s-0042-119648.
Reisenauer C, Muche-Borowski C, Anthuber C, Finas D, Fink T, Gabriel B, et al. Interdisciplinary S2e guideline for the diagnosis and treatment of stress urinary incontinence in women: short version - AWMF registry no. 015-005, July 2013. Geburtshilfe Frauenheilkd. 2013;73(9):899–903. https://doi.org/10.1055/s-0033-1350871.
Howard D, Miller JM, Delancey JO, Ashton-Miller JA. Differential effects of cough, valsalva, and continence status on vesical neck movement. Obstet Gynecol. 2000;95(4):535–40.
Dietz HP, Clarke B, Herbison P. Bladder neck mobility and urethral closure pressure as predictors of genuine stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(5):289–93.
Peschers UM, Vodusek DB, Fanger G, Schaer GN, DeLancey JO, Schuessler B. Pelvic muscle activity in nulliparous volunteers. Neurourol Urodyn. 2001;20(3):269–75.
Miller JM, Perucchini D, Carchidi LT, DeLancey JO, Ashton Miller J. Pelvic floor muscle contraction during a cough and decreased vesical neck mobility. Obstet Gynecol. 2001;97(2):255–60.
Junginger B, Seibt E, Baessler K. Bladder-neck effective, integrative pelvic floor rehabilitation program: follow-up investigation. Eur J Obstet Gynecol Reprod Biol. 2014;174:150–3. https://doi.org/10.1016/j.ejogrb.2013.12.022.
Junginger B, Baessler K, Sapsford R, Hodges PW. Effect of abdominal and pelvic floor tasks on muscle activity, abdominal pressure and bladder neck. Int Urogynecol J. 2010;21(1):69–77. https://doi.org/10.1007/s00192-009-0981-z.
Baessler K, Junginger B. Traditional gymnastic exercises for the pelvic floor often lead to bladder neck descent - a study using perineal ultrasound. Geburtshilfe Frauenheilkd. 2017;77(7):765–70. https://doi.org/10.1055/s-0043-103460.
Lovegrove Jones RC, Peng Q, Stokes M, Humphrey VF, Payne C, Constantinou CE. Mechanisms of pelvic floor muscle function and the effect on the urethra during a cough. Eur Urol. 2009.
Smith MD, Coppieters MW, Hodges PW. Postural response of the pelvic floor and abdominal muscles in women with and without incontinence. Neurourol Urodyn. 2007;26(3):377–85. https://doi.org/10.1002/nau.20336.
Junginger B, Baessler K. The effect of maximal and submaximal pelvic floor contractions on bladder neck elevation and intraabdominal pressure. Int Urogynecol J. 2008;19(Suppl 1):S71.
Baessler K, O'Neill SM, Maher CF, Battistutta D. A validated self-administered female pelvic floor questionnaire. Int Urogynecol J. 2010;21(2):163–72. https://doi.org/10.1007/s00192-009-0997-4.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JOL, Klarskov P, et al. The standardisation of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7.
Anderson RS, Shepherd AM, Feneley RC. Microtransducer urethral profile methodology: variations caused by transducer orientation. J Urol. 1983;130(4):727–8.
Ulmsten U, Asmussen M, Lindstrom K. A new technique for simultaneous urethrocystometry including measurements of the urethral pressure profile. Urol Int. 1977;32(2-3):127–36.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21(1):5–26.
Dietz HP. Ultrasound imaging of the pelvic floor. Part I: two-dimensional aspects. Ultrasound Obstet Gynecol. 2004;23(1):80–92.
Reddy AP, DeLancey JO, Zwica LM, Ashton-Miller JA. On-screen vector-based ultrasound assessment of vesical neck movement. Am J Obstet Gynecol. 2001;185(1):65–70.
Peng Q, Jones R, Shishido K, Constantinou CE. Ultrasound evaluation of dynamic responses of female pelvic floor muscles. Ultrasound Med Biol. 2007;33(3):342–52.
Shek KL, Dietz HP. The urethral motion profile: a novel method to evaluate urethral support and mobility. Aust N Z J Obstet Gynaecol. 2008;48(3):337–42. https://doi.org/10.1111/j.1479-828X.2008.00877.x.
Rahmanian S, Jones R, Peng Q, Constantinou CE. Visualization of biomechanical properties of female pelvic floor function using video motion tracking of ultrasound imaging. Stud Health Technol Inform. 2008;132:390–5.
Smith MD, Coppieters MW, Hodges PW. Postural activity of the pelvic floor muscles is delayed during rapid arm movements in women with stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2006.
Thompson JA, O'Sullivan PB, Briffa NK, Neumann P. Comparison of transperineal and transabdominal ultrasound in the assessment of voluntary pelvic floor muscle contractions and functional manoeuvres in continent and incontinent women. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(7):779–86.
Peschers UM, Gingelmaier A, Jundt K, Leib B, Dimpfl T. Evaluation of pelvic floor muscle strength using four different techniques. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(1):27–30.
Schaer GN, Perucchini D, Munz E, Peschers U, Koechli OR, Delancey JO. Sonographic evaluation of the bladder neck in continent and stress-incontinent women. Obstet Gynecol. 1999;93(3):412–6.
Peschers U, Schaer G, Anthuber C, Delancey JO, Schuessler B. Changes in vesical neck mobility following vaginal delivery. Obstet Gynecol. 1996;88(6):1001–6.
Thibault-Gagnon S, Auchincloss C, Graham R, McLean L. The temporal relationship between activity of the pelvic floor muscles and motion of selected urogenital landmarks in healthy nulliparous women. J Electromyogr Kinesiol. 2018;38:126–35. https://doi.org/10.1016/j.jelekin.2017.11.012.
Wijma J, Tinga DJ, Visser GH. Perineal ultrasonography in women with stress incontinence and controls: the role of the pelvic floor muscles. Gynecol Obstet Investig. 1991;32(3):176–9.
Van K, Hides JA, Richardson CA. The use of real-time ultrasound imaging for biofeedback of lumbar multifidus muscle contraction in healthy subjects. J Orthop Sports Phys Ther. 2006;36(12):920–5. https://doi.org/10.2519/jospt.2006.2304.
Baessler K, Junginger B. Which mechanisms keep us continent?-the role of pelvic floor muscles, bladder neck support and motor control. Int Urogynecol J. 2012;23(2 Suppl):219–20.
Hung HC, Hsiao SM, Chih SY, Lin HH, Tsauo JY. Effect of pelvic-floor muscle strengthening on bladder neck mobility: a clinical trial. Phys Ther. 2011;91(7):1030–8. https://doi.org/10.2522/ptj.20100186.
Miller JM, Ashton-Miller JA, DeLancey JO. A pelvic muscle precontraction can reduce cough-related urine loss in selected women with mild SUI. J Am Geriatr Soc. 1998;46(7):870–4.
Burgio KL, Kraus SR, Menefee S, Borello-France D, Corton M, Johnson HW, et al. Behavioral therapy to enable women with urge incontinence to discontinue drug treatment: a randomized trial. Ann Intern Med. 2008;149(3):161–9.
Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int Urogynecol J. 2017;28(2):191–213. https://doi.org/10.1007/s00192-016-3123-4.
Braekken IH, Majida M, Engh ME, Bo K. Morphological changes after pelvic floor muscle training measured by 3-dimensional ultrasonography: a randomized controlled trial. Obstet Gynecol. 2010;115(2 Pt 1):317–24. https://doi.org/10.1097/AOG.0b013e3181cbd35f.
Dolan LM, Dixon WE, Brown K, Ord T, Hilton P. Randomized comparison of vaginal and rectal measurement of intra-abdominal pressure during subtracted dual-channel cystometry. Urology. 2005;65(6):1059–63. https://doi.org/10.1016/j.urology.2004.12.025.
Acknowledgements
This study was part of a project supported by the German Research Foundation (Deutsche Forschungsgemeinschaft – DFG): Project number: 157173310.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Junginger, B., Vollhaber, H. & Baessler, K. Submaximal pelvic floor muscle contractions: similar bladder-neck elevation, longer duration, less intra-abdominal pressure. Int Urogynecol J 29, 1681–1687 (2018). https://doi.org/10.1007/s00192-018-3725-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3725-0