Abstract
Introduction and hypothesis
Urogenital symptoms are prevalent in older women, but there is little data available on the prevalence, bother, impact and associations with low back pain (LBP), obesity, parity, mental health (MH) and quality of life (QOL) in young women. Our aim was to determine the prevalence, bother and impact of urogenital symptoms and to explore associations with LBP, obesity, parity, MH and QOL in 22 year-old women.
Methods
This was a cross-sectional evaluation using data collected from 588 women in the Raine Study, a pregnancy cohort in which participants have been regularly followed up from birth until 22 years. Data was analysed using descriptive statistics, univariate comparisons and linear regression models.
Results
Prevalence of urogenital symptoms were stress urinary incontinence (SUI) 6.3%, mixed urinary incontinence (MUI) 11.5%, leakage of drops 5.8%, urge urinary incontinence (UUI) 5.3%, bothersome urinary frequency 41.5%, difficulty emptying 11.8% and urogenital pain 22.9%. Urinary frequency, MUI, difficulty emptying and urogenital pain were most bothersome, whilst difficulty emptying and urogenital pain were associated with greatest impact. Urinary frequency, SUI, leakage of drops, difficulty emptying and urogenital pain were associated with current LBP and LBP ever. Difficulty emptying and urogenital pain were associated with chronic LBP. Urogenital symptoms were not associated with obesity or parity. Women with urogenital symptoms had significantly poorer scores on the Mental Component Score of the Short Form Health Survey (SF)-12 and all aspects of the Depression Anxiety Stress Score.
Conclusions
Urogenital symptoms are prevalent in young women, bothersome for some and are associated with LBP, poorer MH and reduced QOL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urogenital symptoms such as urinary incontinence (UI), lower urinary tract symptoms (LUTS) and urogenital pain have been associated with significant bother and impact, obesity, parity, low back pain (LBP), poorer mental health (MH) and poorer quality of life (QOL) in middle-aged and older women; however, there is less data available pertaining specifically to young women [1,2,3,4,5]. In addition, prevalence studies tend to cluster women from age 18 to the 30s, suggesting that at some point between late adolescence and early adulthood, the prevalence of UI and LUTS begins to increase, but little data is available on the age at which this occurs or about factors associated with these changes. Therefore, more specific estimates during early adulthood may be beneficial [6,7,8]. Practically, understanding this transition period may help improve prevention and management strategies and inform when to target such measures. Recent research suggests that urogenital symptoms do not occur in isolation but are associated with other pain problems and MH-related factors [3]. However, there is little data available for young women, and therefore, detailed comorbidity patterns are not established. Understanding comorbidities could assist in the design of holistic management programs. The first aim of this study was to estimate the prevalence, bother and impact of urogenital symptoms specifically for young women using standardised terminology and validated questionnaires. The second aim was to explore associations between urogenital symptoms and LBP, obesity, parity, MH and QOL in these women.
Materials and methods
Cross-sectional evaluation was conducted using data from participants in the Western Australian Pregnancy Cohort (Raine) Study at the 22-year follow-up [9]. The Raine Study started as a pregnancy cohort and included 2868 babies at birth. Participants have been followed up at regular intervals, with each follow-up including many measures of health, disease and demographics. The cohort has retained good representativeness to the general population [9]. At the 22-year follow-up, 1414 participants completed questionnaires investigating a number of health elements, including urogenital symptoms, current and past history of LBP, parity, MH, QOL and a physical examination where height and weight were measured. Of the 1414 participants, 607 were women and were therefore included in this study. This project was approved by the Raine Study Executive Committee. Ethical approval was obtained through Curtin University (RDHS-122-15).
Measures
The seven urogenital symptoms assessed were UI, stress UI (SUI), urge UI (UUI), mixed UI (MUI), bothersome urinary frequency, difficulty emptying the bladder and urogenital pain. A combined estimate of prevalence and bother was measured using the Urogenital Distress Inventory–Short Form (UDI-6), which has established reliability and validity [10]. Participants were asked the following questions: Do you experience, and, if so, how much are you bothered by: 1. Frequent urination (bothersome urinary frequency)? 2. Urine leakage related to feeling of urgency (UUI)? 3. Urine leakage related to physical activity, coughing or sneezing? 4. Small amounts of urine leakage (drops)? 5. Difficulty emptying your bladder? 6. Pain or discomfort in the lower abdomen/genital area (urogenital pain)?. A urogenital symptom was considered to be present and bothersome when a response of slightly, moderately or greatly was given to any one of the questions.
SUI was defined when a response of either slightly, moderately or greatly was given to leaking urine related to physical activity, coughing or sneezing. Although small amounts of urine leakage (drops) is considered as a stress symptom in terms of the UDI-6, potentially, it could be any form of UI; therefore, in this study, it was analysed separately. MUI was considered when a response of either slightly, moderately or greatly was given to questions 2 (UUI), 3 (SUI) or 4 (leakage of drops).
The Pelvic Floor Impact Questionnaire Short Form 7 (PFIQ-7) has established validity and reliability for assessing the impact of urogenital symptoms on QOL in women [11]. Seven questions ask if urinary problems/pain or discomfort have affected ability to do household chores, physical activities, entertainment activities, travel, participate in social activities, emotional health and frustration [12]. For this study, the responses were scored as follows: not at all = 0; slightly = 1; greatly and moderately (scored together due to low numbers) = 2. Scores were added, with a minimum score of 0 indicating no impact and 14 indicating maximal impact.
LBP prevalence was measured using questions from the modified Nordic Questionnaire, which is both valid and reliable [13]. LBP was classified as chronic (positive response to: Has your low back pain ever lasted for more than 3 months continuously? and/or positive response to: Has your low back pain ever lasted for more than 3 months off and on?); current (positive response to: Has your low back been painful at any time in the last month?) and ever (positive response to: Have you ever had low back pain?). Body mass index (BMI) was calculated as weight (kilogrammes) divided by height (meters) squared, both being reliable and valid [14]. Women were classified as being underweight (BMI < 18.5); normal weight (BMI 18.5- to < 25), overweight (BMI ≥25 to < 30) or obese (BMI ≥30) [15]. Parity was ascertained by: Do you have any biological children? (no = nulliparous, yes = parous). MH was assessed using the short-form Depression Anxiety Stress Scale (DASS-21), a valid and reliable measure of depression, anxiety and stress [16]. QOL was measured using the Short Form 12 Health Survey (SF-12), which consists of 12 questions assessing physical and mental well-being, also valid and reliable for assessing QOL in women [17]. Separate physical (PCS) and mental (MCS) component scores were calculated, standardised to a mean of 50 [standard deviation (SD) = 10] with higher scores indicating better QOL [17].
Statistical analysis
-
Aim 1: For each urogenital symptom, the presence of a bothersome symptom was estimated. Proportions of women with slight and moderate/great bother and with slight (PFIQ-7 = 1–7) or moderate/great impact (PFIQ-7 > 7–14), were calculated. A binary variable was derived denoting the prevalence of having at least one or more symptoms assessed.
-
Aim 2: We examined associations between each urogenital symptom and LBP, obesity, parity, MH and QOL using a series of estimated logistic regressions. Each urogenital symptom was considered as the dependent variable, with the reference group being those without any urogenital symptoms.
MH measures (DASS) displayed skewed distributions and were parametrised in logistic regression models as ordinal [none (z-score > 0.5), mild (z-score 0.5–1.0), moderate (z-score 1.0–2.0) severe (z-score 2.0–3.0), extremely severe (z-score > 3.0) [18] where numbers permitted, or as binary variable categories (none or mild vs moderate or more) to avoid empty or sparse cells for urogenital symptoms with low prevalence. Estimates for MH (DASS-21) and QOL (SF-12) were adjusted for the presence of current LBP in instances where the urogenital symptom was associated with this potential confounder. Odds ratios (OR) with associated 95% confidence intervals (CI) and p values are presented. Data were analysed using IBM SPSS version 24.0 (Armonk, NY, USA). P values <0.05 were considered statistically significant.
Results
Of the 607 women completing the 22-year follow-up questionnaire, 581 (95.6%) provided valid responses for all six questions assessing the presence of the seven urogenital symptoms, whilst 588 (96.7%) provided a valid response to one or more of the six questions. Sample characteristics are shown in Table 1.
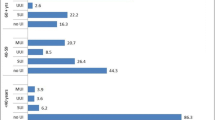
Three hundred and thirty-four participants reported at least one current bothersome urogenital symptom (57.5%). The most prevalent type was MUI (11.5%), followed by SUI (6.3%), small drops of leakage (5.8%) and UUI (5.3%). Prevalence of bothersome urinary frequency was 41.5%; however, most of these women (62.7%) reported only slight bother (Table 2). Prevalence of bothersome urinary frequency at moderate/great levels was 15.5%. Difficulty emptying the bladder was reported by 11.8% and urogenital pain by 22.9%. (Table 2).
Urogenital symptoms presenting as most bothersome (moderate/great) were urogenital pain 47/134 (64.9%), frequency 91/244 (37.3%), MUI 22/67 (32.8%) and difficulty emptying the bladder 17/69 (24.6%). In terms of UI, MUI was more bothersome than SUI or UUI (Table 2).
Urogenital symptoms associated with the greatest impact on QOL of young women were difficulty emptying the bladder [7/67 (10.4%)] and urogenital pain [10/131 (7.6%)] . Although most women with each symptom did not report a level of impact (i.e. PRIQ-7 = 0), slight impact was reported by at least one third of all women experiencing each symptom (Table 2).
Table 3 presents OR for the presence of urogenital symptoms according to LBP, obesity, parity, MH, and physical health. The presence of at least one urogenital symptom was strongly associated with LBP ever (Table 3). LBP ever and current LBP were also significantly associated with bothersome urinary frequency, SUI, leakage of drops, difficulty emptying and urogenital pain. Chronic LBP was associated with difficulty emptying the bladder and urogenital pain (Table 3).
There were no associations between obesity or parity and any urogenital symptoms (Table 3). Higher levels of depression, anxiety and stress were significantly associated with the presence of at least one urogenital symptom and with frequency, MUI, difficulty emptying and pain (Table 3). Lower levels of mental component score were associated with presence of at least one urogenital symptom and frequency, MUI, difficulty emptying and pain. Lower levels of physical component score were not significantly associated with urogenital symptoms (Table 3).
Discussion
Prevalence
This study found that the prevalence of any UI in young, predominantly nulliparous, women to be between 5.3% and 11.5%. This is higher than the reported prevalence of 0.3% for UI in 15–17-year-olds [1] but lower than the prevalence range of 9.3–20.4% currently reported for women <30 [6,7,8]. Prevalence data has previously been reported for mixed aged groups: 15–25 years [6], 16–30 [7] and 18–29 [8], whilst women in this study were all aged 22 years. This may account for the lower prevalence. It is possible that at age 22, the downward trend of UI seen in children and adolescents has begun to turn upward. The prevalence of the main subtypes of UI in this study were SUI 6.3%, UUI 5.3% and MUI 11.5%. The prevalence of SUI and UUI are consistent with the prevalence ranges currently reported in the literature for women aged <30: SUI 5.9–7.7% and UUI 3.4–9% [6,7,8].
However, the prevalence of MUI is much higher in this study than the current prevalence range of 1.9–5.4% in women <30 [6,7,8]. This may be due to the way MUI was defined in the questionnaires used in each study. In our study, UDI-6 was used to measure prevalence of UI subtypes, and leakage of drops of urine was included in MUI, which may have contributed to the higher prevalence. Leakage of drops was analysed separately to SUI, as the researchers were not sure that all women reporting leakage of small drops had SUI. However, results show that leakage of drops and SUI behave in a similar way and therefore it is likely that young women are reporting SUI as leakage of drops. Current literature suggests that the severity of UI increases with increasing age [1]. Given that between 5.3% and 11.5% of the young adult women in our study are already experiencing a form of UI, screening younger women for UI would provide an opportunity for early intervention.
LUTS, such as bothersome urinary frequency, difficulty emptying the bladder and urogenital pain, were prevalent in young women, with 41.5% reporting urinary frequency, 11.8% reporting difficulty emptying the bladder and 22.9% reporting urogenital pain. These prevalence ranges are higher than those reported in literature for women aged younger than 39: frequency 7.9–9.5%, difficulty emptying the bladder 0.6–6.0% and bladder pain 3.9% [19, 20]. However, comparing these results is difficult, as different questionnaires and definitions were used. Definitions used for daytime urinary frequency may be based on the responder’s perception of whether they void too often per day (as recommended by the International Continence Society) or alternatively on a threshold number of voids per day (Irwin et al. 2008). One study [19] used a responder’s perception-based definition: “The complaint that micturition occurs more frequently than previously deemed normal by the woman” [21], whilst the other defined urinary frequency as more than eight voids per day [20]. The UDI-6 used for our study includes a responder’s perception-type question where the young women were asked if they experienced urinary frequency and, if so, how much were they bothered by it. No data were collected on the number of voids per day or fluid intake. Irwin et al. compared prevalence of ICS-defined frequency (responder perception) with a numerical threshold of more than eight voids per day in a population-based sample. They found the prevalence of urinary frequency was higher using the perception definition than using the numerical threshold definition (25% vs 19% of women with overactive bladder) [22] . This may, in part, explain the higher prevalence of frequency in our sample. Nonetheless, further research into the number of day voids and fluid intake in young Australian women is recommended to obtain a better understanding of urinary frequency in this group and whether it is related to higher fluid intake or other lifestyle factors.
For difficulty emptying the bladder, the women in this study were asked whether they experienced—and if so, were they bothered by—difficulty emptying the bladder. In other studies, the International Continence Foundation definitions are used in which difficulty emptying the bladder is described more specifically as straining, hesitancy, intermittency or slow stream, which may explain the higher numbers in our study [19,20,21].
The pain definition used in our study was quite broad: “pain or discomfort in the lower abdomen/genital area”, whereas in other studies, women were asked about bladder pain, which is the likely reason for the higher prevalence in our study. In addition, a recent study reported the prevalence of severe menstrual pain in this same cohort of young women aged at 20 and 22 years to be 17% [23]. Further investigation of urogenital and menstrual pain may be useful, given there could be potential shared underlying pain mechanisms.
Bother and impact
Urogenital pain, urinary frequency and difficulty emptying the bladder caused most bother for the young women in this study, and MUI was be more bothersome than SUI and UUI. Urogenital symptoms associated with the greatest impact on the QOL were difficulty emptying the bladder and urogenital pain, which is similar to current literature on older women [2, 4, 5]. In terms of impact, at least a third of all young women who reported having each urogenital symptom reported slight impact on their ability to perform simple daily activities. Whilst this proportion is fairly small, it is important to remember the young age of these women, and that the tasks being affected are normal activities of daily living, such as shopping, entertaining and household chores. Previous studies have found that UI in young women is also associated with adverse impact on daily life, such as limiting fluid intake, wearing pads due to fear of odour and poorer overall well-being [6, 7].
Correlates of urogenital symptoms
Lower back pain
Strong associations were identified between the presence of at least one urogenital symptom and both LBP ever and current LBP, with SUI and leakage of drops being associated with current LBP and a history of LBP ever. This appears consistent with the finding that pre-existing and/or new-onset UI or LBP can be associated with a higher risk of developing LBP or UI, respectively. [24]. The associations between LBP and UI are likely to be complex and are not yet fully understood. It has been suggested that sensorimotor changes linked to altered motor control of muscles, including abdominal, back and pelvic floor muscles (PFM), known to be associated with a history of LBP and UI, may underpin this relationship [24].
In addition, there were strong associations between difficulty emptying the bladder and urogenital pain with current, chronic and LBP ever. This comorbidity may relate to shared musculature, or shared underlying pain mechanisms [25]. In this study, urogenital pain was considered as any pain in the lower abdominal or genital area, and as such, it is possible that this included some LBP, thus confounding data.
Obesity
Obesity was more strongly associated with SUI and leakage of small drops of urine (although not significant) than with any of the other urogenital symptoms. This may be due to a lack of power, as only 17% of the sample were classified as obese. Also, sensitivity analysis did not identify significant associations. These results are consistent with another study that reported no association between UI and BMI in young nulligravid women [7]. However, there is strong evidence to suggest that obesity increases intra-abdominal pressure, which then predisposes SUI [1], and that women who become obese at a younger age are at a higher risk of developing UI in middle age [1, 26]. In light of this, it is recommended that young women are given advice and education on the risks associated with being obese, strategies to help reduce their BMI and referred on for early diagnosis and treatment of SUI. There is good evidence that both reducing BMI and simple, safe treatments like PFM training (PFMT) can effectively treat and reduce symptoms of SUI [1]. The prospective nature of the Raine study means that additional data on the association between obesity and urogenital symptoms can be gathered as these women age.
Parity
There was no association between parity and UI, which may be due to the very low number of parous women in our study (6.1%), thereby reducing the power, or because most parous women had only one baby. However, parity is an established risk factor for UI, with increasing parity being associated with increased risk of UI, and this association is strongest for women in their 30s and 40s [1]. The underlying mechanisms of exactly how pregnancy and childbirth predispose to UI are still not fully understood [1]. Current research suggests pelvic floor dysfunction may occur as a result of trauma to the muscles, connective tissue, nerves or blood supply during vaginal birth, which can then predispose women to UI [1]. It is possible that parity and obesity were not found to be associated with urogenital symptoms in this study due to the relatively young (all 22 years old), mostly nulliparous, sample. Previous studies finding associations have been in older or mixed age samples, and it may be that the influence of BMI becomes greater with age and parity.
Mental health and quality of life
The results suggest significantly poorer DASS and SF-12 scores in young women with urogenital symptoms as opposed to those without symptoms, even after adjustment for comorbid LBP. However, mean SF-12 scores for the young women with urogenital symptoms were within 1 SD of the population mean (PCS = 52.6; MCS = 43.7). Difference in these scores between women with and without urogenital symptoms was only 1.6 and 2.7 points, respectively, although it was statistically significant. Therefore, clinical relevance of the association between urogenital symptoms, particularly urogenital pain, and poorer MH in young women, is difficult to ascertain. Previous studies reported an association between urogenital symptoms and poorer MH and QOL in middle-aged and older women [1, 4, 5]. Therefore, it could be recommended that young women presenting with urogenital symptoms be screened for MH and QOL. The prospective nature of the Raine study may provide insight into these associations in future follow-up studies.
Our results also showed an association between MUI and higher depression, anxiety and stress scores, which is in accordance with previous studies that included middle-age and older women [4, 27]. An association between UI and depression and MUI and anxiety have been reported; however, the underlying mechanisms for the observed associations are complex and not yet fully understood [1, 4].
Significance and implications
The results indicate that urogenital symptoms are prevalent and bothersome in young women and are associated with significant impact, including poorer MH and QOL. Research has shown that many women who experience urogenital symptoms do not seek help [28] and that younger women have little insight into their urogenital health [6]. It is therefore recommended that primary prevention programmes be developed, such as community-based education sessions, and that health professionals screen young women for urogenital symptoms and their impact during routine episodes of care. Whilst there is Level 1 evidence that simple, safe, cost-effective treatments such as PFMT are effective for treating and reducing urogenital symptoms [29], optimal management of urogenital symptoms requires a multidimensional view that considers physical health, LBP history, MH and QOL to minimise their impact on young women. The Raine Study is a prospective study and as such there is great potential for further follow-up of these women to obtain more detailed information and data on trajectories of urogenital symptoms and associated factors. This study involved a community sample of women of the same age, thus minimising selection bias.
Limitations of study and recommendations
The urogenital symptoms were based on participant self-report and there is thus potential for misclassification, especially for those who reported leakage of small drops of urine. Not all young women were able to attend the physical examination, and therefore numbers available for estimating the association BMI with urogenital symptoms were small. Another limitation is that the association of sexual activity with urogenital symptoms was not assessed, as sexually active women may be at a higher risk of having LUTS.
As this is a cross-sectional evaluation, findings, associations and causality cannot be drawn. Further research is recommended to establish the prevalence of other types of UI in young women (such as postmicturition dribble and passive incontinence, which are not included in the UDI-6), to study specific pain syndromes such as bladder pain syndrome, chronic pelvic pain and urethral pain syndrome, and to determine the direction and underlying mechanisms of associations between urogenital symptoms, QOL and MH in young women.
Conclusion
Urogenital symptoms are both prevalent and bothersome in some young women. They are associated with LBP, poorer MH and QOL and functional impacts.
References
Milsom I, Altman D, Cartwright R, Lapitan M, Nelson R, Sillén U, et al. Committee 1: epidemiology of urinary incontinence (UI) and other lower urinary tract symptoms (LUTS), pelvic organ prolapse (POP) and anal incontinence (AI). In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence. 5th international consultation on incontinence, vol committee 1. Paris: ICUD-EAU; 2013. p. 15–107.
Abrams P, Smith AP, Cotterill N. The impact of urinary incontinence on health-related quality of life (HRQoL) in a real-world population of women aged 45–60 years: results from a survey in France, Germany, the UK and the USA. BJU Int. 2015;115(1):143–52. https://doi.org/10.1111/bju.12852.
Engeler D, Baranowski A, Borovicka J, Dinis-Oliveira P, Elneil S, Hughes J, Messelink E, de Williams AC, Cottrell A, Goonewardene S (2016) EAU GUIDELINES ON CHRONIC PELVIC PAIN. European Association of Urology. Accessed 21/02/2017 2016.
Coyne KS, Kvasz M, Ireland AM, Milsom I, Kopp ZS, Chapple CR. Urinary incontinence and its relationship to mental health and health-related quality of life in men and women in Sweden, the United Kingdom, and the United States. Eur Urol. 2012;61(1):88–95. https://doi.org/10.1016/j.eururo.2011.07.049.
Clemens JQ, Link CL, Eggers PW, Kusek JW, Nyberg LM Jr, McKinlay JB. Prevalence of painful bladder symptoms and effect on quality of life in black, Hispanic and white men and women. J Urol. 2007;177(4):1390–4. https://doi.org/10.1016/j.juro.2006.11.084.
Bardino M, Di Martino M, Ricci E, Parazzini F. Frequency and determinants of urinary incontinence in adolescent and young nulliparous women. J Pediatr Adolesc Gynecol. 2017;28(6):462–70. https://doi.org/10.1016/j.jpag.2015.01.003.
O’Halloran T, Bell R, Robinson P, Davis S. Urinary incontinence in young Nulligravid women. Ann Intern Med. 2012;157:87–93.
Schreiber Pedersen L, Lose G, Hoybye MT, Elsner S, Waldmann A, Rudnicki M. Prevalence of urinary incontinence among women and analysis of potential risk factors in Germany and Denmark. Acta Obstet Gynecol Scand. 2017; https://doi.org/10.1111/aogs.13149.
Straker L, Mountain J, Jacques A, White S, Smith AP, Landau L, Stanley F, Newnham J, Pennell C, Eastwood P (2017) Cohort Profile: The Western Australian Pregnancy Cohort (Raine) Study-Generation 2. Int J Epidemiol.
Uebersax JS, Wyman JF, Shumaker SA, McClish DK. Short forms to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and the urogenital distress inventory. Neurourol Urodyn. 1995;14(2):131–9. https://doi.org/10.1002/nau.1930140206.
Staskin D, Kelleher C, Bosch R, Cotterill N, Coyne K, Kelleher C, et al. Initial assessment of urinary incontinence in adult male and female patients (5A) patient-reported outcome assessment (5B). In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence. 5th international consultation on incontinence, vol committee 5. Paris: ICUD-EAU; 2013. p. 361–428.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13. https://doi.org/10.1016/j.ajog.2004.12.025.
Dionne CE, Dunn K, Croft P, Nachemson AL, Buchbinder R, Walker B, et al. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine. 2008;33(1):95–103.
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Bailey KR, Collazo-Clavell ML, et al. Lopez-Jimenez F (2008) accuracy of body mass index to diagnose obesity in the US adult population. Int J Obes. 2005;32(6):959–66. https://doi.org/10.1038/ijo.2008.11.
World Health Organization (2016) BMI classification. World Health Organization. Accessed 15 June 2016 2016.
Henry JD, Crawford JR. The short-form version of the depression anxiety stress scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44(Pt 2):227–39. https://doi.org/10.1348/014466505x29657.
Ware JE Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. https://doi.org/10.2307/3766749.
Lovibond SH, Lovibond PF (1995) Manual for the depression anxiety stress scales. Psychology Foundation.
Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50(6):1306–15. https://doi.org/10.1016/j.eururo.2006.09.019.
van Breda HMK, Bosch JLHR, de Kort LMO. Hidden prevalence of lower urinary tract symptoms in healthy nulligravid young women. Int Urogynecol J. 2015;26(11):1637–43. https://doi.org/10.1007/s00192-015-2754-1.
Haylen B, de Ridder D, Freeman R, Swift S, Berghmans B, Lee J, et al. An international Urogynecological association (IUGA) / international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4–20.
Irwin D, Milsom I, Kopp Z, Abrams P. EPIC study group. Symptom bother and health care-seeking behavior among individuals with overactive bladder. Eur Urol. 2008;53(5):1029–37.
Slater H, Paananen M, Smith A, O’Sullivan P, Briggs A, Hickey M, et al. Heightened cold pain and pressure pain sensitivity in young female adults with moderate-to-severe menstrual pain. Pain. 2015;156(12):2468–78.
Smith MD, Russell A, Hodges PW. The relationship between incontinence, breathing disorders, gastrointestinal symptoms, and back pain in women: a longitudinal cohort study. Clin J Pain. 2014;30(2):162–7. https://doi.org/10.1097/AJP.0b013e31828b10fe.
Beales D, O’Sullivan P. A person-centred biopsychosocial approach to assessment and management of pelvic girdle pain. In: Grieve’s modern musculoskeletal physiotherapy. London: Elsevier Health Sciences; 2015. p. 488–95.
Mishra G, Hardy R, Cardozo L, Kuh D. Body weight through adult life and risk of urinary incontinence in middleaged women: results from a British prospective cohort. Int J Obes. 2008;32(9):1415–22.
Felde G, Bjelland I, Hunskaar S. Anxiety and depression associated with incontinence in middle-aged women: a large Norwegian cross-sectional study. Int Urogynecol J. 2012;23(3):299–306. https://doi.org/10.1007/s00192-011-1564-3.
Lasserre A, Pelat C, Guéroult V, Hanslik T, Chartier-Kastler E, Blanchon T, et al. Urinary incontinence in French women: prevalence, risk factors, and impact on quality of life. Eur Urol. 2009;56(1):177–83. https://doi.org/10.1016/j.eururo.2009.04.006.
Moore K, Dumoulin C, Bradley C, Burgio K, Chambers T, Hagen S, et al. Adult conservative management. In: incontinence: 5th international consultation on incontinence. Paris: ICUD-EAU; 2013.
Acknowledgements
We would like to acknowledge the Raine Study participants for their ongoing participation in the study, the families of the Raine Study participants, the Raine Study Team for study co-ordination and data collection, the UWA Centre for Science for utilisation of the facility and the Sleep Study Technicians. We would like to acknowledge the University of Western Australia (UWA), Curtin University, the Raine Medical Research Foundation, the UWA Faculty of Medicine, Dentistry and Health Sciences, the Telethon Kids Institute, the Women’s and Infant’s Research Foundation (King Edward Memorial Hospital), Edith Cowan University, Murdoch University and University of Notre Dame for providing funding for the Core Management of the Raine Study. The 22-year Raine Study follow-up was funded by NHMRC project grants 1027449, 1044840 and 1021855.
Funding
Funding was also generously provided by Safework Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Stockil, L., Thompson, J., Briffa, K. et al. Urogenital symptoms: prevalence, bother, associations and impact in 22 year-old women of the Raine Study. Int Urogynecol J 29, 1807–1815 (2018). https://doi.org/10.1007/s00192-018-3639-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3639-x