Abstract
Introduction and hypothesis
The efficacy and safety of removing or preserving the uterus during reconstructive pelvic surgery is a matter of debate.
Methods
We performed a systematic review and meta-analysis of studies that compared hysteropreservation and hysterectomy in the management of uterine prolapse. PubMed, Medline, SciELO and LILACS databases were searched from inception until January 2017. We selected only randomized controlled trials and observational cohort prospective comparative studies. Primary outcomes were recurrence and reoperation rates. Secondary outcomes were: operative time, blood loss, visceral injury, voiding dysfunction, duration of catheterization, length of hospital stay, mesh exposure, dyspareunia, malignant neoplasia and quality of life.
Results
Eleven studies (six randomized and five non-randomized) were included involving 910 patients (462 in the hysteropreservation group and 448 in the hysterectomy group). Pooled data including all surgical techniques showed no difference between the groups regarding recurrence of uterine prolapse (RR 1.65, 95% CI 0.88–3.10; p = 0.12), but the risk of recurrence following hysterectomy was lower when the vaginal route was used with native tissue repair (RR 10.61; 95% CI 1.26–88.94; p = 0.03). Hysterectomy was associated with a lower reoperation rate for any prolapse compartment than hysteropreservation (RR 2.05; 95% CI 1.13–3.74; p = 0.02). Hysteropreservation was associated with a shorter operative time (mean difference −12.43 min; 95% CI −14.11 to −10.74 ; p < 0.00001) and less blood loss (mean difference −60.42 ml; 95% CI −71.31 to −49.53 ml; p < 0.00001). Other variables were similar between the groups.
Conclusions
Overall, the rate of recurrence of uterine prolapse was not lower but the rate of reoperation for prolapse was lower following hysterectomy, while operative time was shorter and blood loss was less with hysteropreservation. The limitations of this analysis were the inclusion of nonrandomized studies and the variety of surgical techniques. The results should be interpreted with caution due to potential biases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) is a common condition that affects more than 40% of women over the age of 50 years. Approximately 11% of women have undergone surgery for POP or urinary incontinence by the age of 80 years, and approximately 30% of them require a revision procedure due to recurrence [1]. There are two primary surgical access routes for reconstructive pelvic surgery: the abdominal approach (via laparotomy or laparoscopy) [1, 2] and the vaginal approach [3, 4]. Techniques that include subtotal or total hysterectomy are the most common approaches to the repair of symptomatic uterine prolapse [5]. However, some authors consider that hysterectomy increases the risk of complications and morbidity and question the need for uterine removal, while others believe that prolapse will recur more frequently if the uterus is preserved [6].
We performed this review and meta-analysis to examine the current available evidence comparing reconstructive pelvic floor surgical procedures that involve hysteropreservation or hysterectomy in the management of uterine prolapse in relation to efficacy and complications.
Materials and methods
The Research Ethics Board of the Federal University of São Paulo approved this study (CCAE number 35,071,014.0.0000.5505). This systematic review was also registered with the PROSPERO database (CRD42016037053). We used the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement to report the results [7].
Eligibility criteria
For a study to be selected for this review, it had to include women with symptomatic uterine prolapse, to compare hysteropreservation with hysterectomy in the surgical treatment of uterine prolapse, to be a prospective, controlled and randomized trial or a prospective and comparative cohort study, and to be published in a peer-reviewed journal. A study was not included if it was published in the form of an abstract, letter to the editor or comments, if its publication was not controlled by a commercial publisher (“gray literature”), if it was a meta-analysis or a review article, or if it included colpocleisis as a surgical procedure.
Search strategy
An exhaustive electronic search was performed of the MEDLINE, PubMed, SciELO and LILACS databases from inception until January 2017. The references of the identified articles were also searched. The search was restricted to articles published in English, Spanish, French and Portuguese. The search was based on the following combined relevant terms and MeSH (Medical Subject Headings of the National Library of Medicine) descriptors: “uterine prolapse”, “vaginal prolapse”, “hysterectomy”, “hysteropexy”, “organ preservation”, “colpohysterectomy”, “surgical meshes”, “quality of life”, “operative time”, “surgery time length”, “operative time”, “complication, postoperative”, “complication, peri-operative”, “complication, intraoperative”, “surgical injury”, “recurrences”, “prevention, primary”, “tumor”, “neoplasia”, and “cancer” (Supplementary Material).
Study selection, data collection and extraction
Two reviewers (S.A.de O. and M.C.M.F.) independently selected and combined the articles, and further extracted the data using a standardized form. Any divergence in study selection and/or extraction of data was resolved by consensus between the two reviewers or by a third reviewer (R.A.C.). Initially, the reviewers evaluated the title and abstract of all studies that were found using the search strategy. Full texts were evaluated if the reports did not provide sufficient information in the title and abstract. Only studies that met the inclusion criteria and did not involve colpocleisis as the treatment for POP were included. A list of potential studies for inclusion in the systematic review was generated. The references in the reviews and the excluded articles were examined to identify studies that possibly could not be captured using the primary search strategy. Only studies that reported the standard deviation (SD) of each variable in question were included in the meta-analysis.
The standardized form included the following information: study title, authors, journal of publication, year of publication, sample size, study design and duration, inclusion and exclusion criteria, randomization, the demographics of the participants, type of procedure, outcome measurements and their results.
Outcomes measured
Primary outcomes included: recurrence rate of uterine prolapse defined as symptomatic prolapse of stage II or more with Pelvic Organ Prolapse Quantification System (POP-Q) point C >0, and reoperation rate related to the repair of prolapse of any compartment after the primary procedure. Secondary outcomes included: operative time related to the uterine prolapse in minutes, intraoperative blood loss in milliliters, visceral injury (bowel or bladder), voiding dysfunction (incomplete micturition with presence of postvoid residual or low urine flow rate), duration of catheterization in days, length of hospital stay in days, mesh exposure, postoperative dyspareunia, malignant neoplasia and quality of life. The terminology and definitions recommended by the International Urogynecology Association were used [8].
Analysis and assessment of the risk of bias
The guidance suggested by the Cochrane Collaboration to assess the risk of bias was followed [9]. The studies were combined into groups according to the surgical techniques and approaches used, and all the data were combined so that the following analyses could be performed:
-
1.
Comparison between hysteropexy and hysterectomy performed vaginally with native tissues in the treatment of uterine prolapse during reconstructive pelvic surgery
-
2.
Comparison between hysteropexy and hysterectomy performed vaginally using mesh in the treatment of uterine prolapse during reconstructive pelvic surgery
-
3.
Comparison between hysteropexy and hysterectomy performed by the abdominal route in the treatment of uterine prolapse during reconstructive pelvic surgery
-
4.
Comparison between abdominal hysteropexy and vaginal hysterectomy in the treatment of uterine prolapse during reconstructive pelvic surgery
-
5.
Overall comparison between hysteropreservation and hysterectomy in the management of uterine prolapse during reconstructive pelvic surgery
Data on dichotomous outcomes from the original studies were pooled to obtain the risk ratio (RR) for the occurrence of an outcome event and the corresponding 95% confidence interval (CI). The outcome data from each study were pooled using a Mantel–Haenszel model and a fixed-effects model was applied. Outcomes for continuous variables were pooled from the original studies using the inverse variance method to obtain the mean difference (MD) for the occurrence of an outcome event and to present the corresponding 95% CIs. Statistical significance was set at p < 0.05. The I 2 statistic was used to describe variations across trials that were due to heterogeneity and not sampling error, and to quantify statistical heterogeneity. The random effects model was applied when the heterogeneity was greater than 50% (I 2 > 50%) [9]. Review Manager 5 software was used for the meta-analysis.
Results
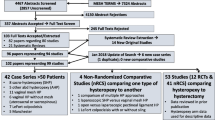
After removing duplicate items, the database search found a total of 1,226 articles. At the end of the review process, 11 studies met the criteria for inclusion and were described and evaluated (Fig. 1) [4, 10,11,12,13,14,15,16,17,18,19]. There were five randomized controlled and six prospective comparative cohort trials comparing hysteropreservation techniques to hysterectomy in patients with uterine prolapse. The included studies accounted for 910 patients (462 in the hysteropreservation and 448 in the hysterectomy groups). The characteristics of the studies included in this review are presented in Table 1. A total of 158 studies were excluded because they did not meet the inclusion criteria or did not provide sufficient data for inclusion in the meta-analysis. Of these studies, 11 compared hysteropreservation and hysterectomy, but they were retrospective cohort studies [20,21,22,23,24,25,26,27,28,29]. Figure 2 shows the quality assessment of the included studies.
Primary outcomes
Recurrence rate
Recurrence rates were reported in ten studies involving a total of 390 patients in the hysteropreservation groups and 378 who had hysterectomy as the treatment for uterine prolapse [4, 10,11,12,13,14,15,16,17,18]. The concept of recurrence was uniform across the studies (symptomatic apical prolapse, POP-Q point C point >0), except in the study by Jeng et al. [19] that included patients with moderate to severe POP, but without a clear classification. The follow-up for the diagnosis of recurrence varied among the studies, ranging from 6 to 29.8 months, mean 18 months (SD 17). Pooled data showed no significant difference between the groups (RR 1.65, 95% CI 0.88–3.10; p = 0.12), but there was a tendency for a lower rate of recurrence with hysterectomy (Fig. 3).
Grouping the studies according to the surgical procedures and approaches, in procedures using the vaginal route with native tissue, the recurrence rate was significantly lower with hysterectomy than with hysteropexy, independent of the technique used for fixation of the apical defect (sacrospinal vault suspension or uterosacral ligament fixation; RR 10.61, 95% CI 1.26–88.94; p = 0.03; Fig. 3). The recurrence rates with both techniques using the vaginal approach with mesh, or both using the abdominal approach were similar whether or not the uterus was preserved, but individual analysis showed that in the majority of the studies the recurrence rate was lower with hysterectomy (Fig. 3). Carramão et al. [18] found recurrence rates of 25% (4 of 16 patients) with vaginal hysteropexy and 13% (2 of 16 patients) with vaginal hysterectomy using mesh, while Rosen et al. [17] found recurrence rates of 12% (4 of 32 patients) with laparoscopic hysteropreservation and 3% (1 of 32 patients) with laparoscopic hysterectomy, both with sacropexy. No difference in recurrence rates was found between abdominal hysteropexy and vaginal hysterectomy (Fig. 3).
Reoperation rate
The same ten studies [4, 10,11,12,13,14,15,16,17,18] that evaluated apical prolapse recurrence rates also reported reoperation rates for any prolapse compartment, with follow-up ranging from 6 to 29.8 months (mean 18 months, SD 17 months). Overall, pooled data showed that the reoperation rate was significantly lower with hysterectomy than with hysteropreservation (RR 2.05, 95% CI 1.13–3.74; p = 0.02; Fig. 4). There were no differences in reoperation rates among procedures using the vaginal approach with native tissue or mesh, or those using the abdominal route, but the majority of the studies reported a higher rate of revision procedures following hysteropexy (Fig. 4). Although a similar finding was observed comparing abdominal hysteropreservation and vaginal hysterectomy with native tissue, Roovers et al. [15] found reoperation rates of 22% (9 of 41 patients) with abdominal hysterosacropexy and 2.4% (1 of 41 patients) with vaginal hysterectomy with cardinal and uterosacral ligament fixation.
Secondary outcomes
Operative time
Four studies [4, 10, 15, 18] evaluated the operative time in a total of 314 procedures. Overall, pooled data showed that the operative time was shorter with hysteropreservation than with hysterectomy (MD −12.43, 95% CI −14.11 to −10.74; p < 0.00001), and also in all subanalyses of groupings of techniques and routes (Fig. 5).
Blood loss
Three studies [4, 15, 18] evaluated the intraoperative blood loss in a total of 223 procedures. Overall, pooled data showed that blood less was less with hysteropreservation than with hysterectomy (MD −60.42, 95% CI −71.31 to −49.53; p < 0.00001; Fig. 6). Among the included studies, only that of Roovers et al. [15] did not show a difference in intraoperative blood loss between abdominal hysterosacropexy and vaginal hysterectomy with native tissue.
Visceral injury
Three studies reported intraoperative visceral injuries in a total of 263 procedures [4, 15, 16]. Two rectal injuries were reported in 124 vaginal hysterectomy procedures with native tissue (one described by Hefni et al. [4] comparing vaginal hysteropexy and vaginal hysterectomy, and one reported by Roovers et al. [15] comparing abdominal hysterosacropexy and vaginal hysterectomy). No visceral injury was observed in the 139 hysteropreservation procedures. Overall, pooled data showed no differences in visceral injuries between the groups (OR 0.30, 95% CI 0.03–2.79; p = 0.29).
Voiding dysfunction
Six studies reported voiding dysfunction following a total of 425 procedures [4, 11, 13, 15, 17, 18]. Overall, pooled data showed similar rates of voiding dysfunction between the groups (RR 1.19, 95% CI 0.39–3.65; p = 0.76; Fig. 7).
Although analyses have also not shown differences in the rate of voiding dysfunction following procedures preserving and removing the uterus, we observed a tendency for the rate to be lower following hysteropexy via the vaginal route. Dietz et al. [13] observed voiding dysfunction rates of 8.5% (3 of 35 patients) with vaginal hysteropexy and 25.8% (8 of 31 patients) with vaginal hysterectomy, both with sacrospinous fixation with native tissue. On the other hand, for procedures performed via the abdominal route, the rate of voiding dysfunction tended to be lower with hysterectomy. Costantini et al. [11] reported voiding dysfunction rates of 11.8% and 2.6% for abdominal hysterosacropexy and abdominal hysterectomy with colposacropexy, respectively.
Duration of catheterization
Only two studies evaluated the duration of catheterization after surgery [10, 15]. Chu et al. [10] compared catheterization duration following vaginal hysteropexy in 52 patients and vaginal hysterectomy in 39 patients, both using anterior and posterior mesh, and found mean catheterization durations of 2.4 and 2.7 days, respectively (MD −0.30, 95% CI −0.51 to −0.09; p = 0.005). In contrast, Roovers et al. [15] compared catheterization duration following abdominal hysterosacropexy and vaginal hysterectomy and vault suspension with native tissue with 41 patients in each arm, and found similar durations of 3.3 and 3.2 days, respectively (MD 0.10, 95% CI −0.02–0.22; p = 0.09). Pooled data from hysteropreservation procedures and hysterectomy revealed no statistically significant difference between the groups (MD −0.00, 95% CI −0.10–0.11; p = 0.94).
Length of hospital stay
Three studies compared the length of hospital stay after surgery in a total of 252 patients [10, 14, 15]. Pooled data showed similar RRs for both procedures (MD −0.06, 95% CI −0.17 to 0.04; p = 0.23). For vaginal techniques with mesh, hospital stay was shorter with hysteropreservation than with hysterectomy (MD −1.45, 95% CI −1.77 to −1.13; p < 0.000001). This finding was mainly accounted for by the study of Neuman et al. [14] who reported mean hospital stays of 1.5 days for hysteropexy in 35 patients and 4.2 days for hysterectomy in 44 patients (MD −2.70, 95% CI −3.17 to −2.23). However, Chu et al. [10] did not observe such a difference, finding mean hospital stays of 4.9 days in 52 patients who had vaginal hysteropexy and 5.3 days in 39 patients who had vaginal hysterectomy (MD −0.40, 95% CI −0.83 to 0.03). Roovers et al. [15] found similar mean hospital stays following abdominal hysterosacropexy (7.7 days) and vaginal hysterectomy (7.6 days), with 41 patients in each group (MD 0.10, 95% CI −0.01 to 0.21).
Mesh exposure
Mesh exposure was reported by four studies in a total of 273 procedures [10, 11, 14, 18]. Mean follow-up was 18 months (SD 10.24 months). Pooled data did not show different RRs between preserving or removing the uterus (RR 0.55; 95% CI 0.26–1.15; p = 0.11; Fig. 8). However, all the included studies showed a higher incidence of mesh exposure when the uterus was removed, with tendency for a lower incidence with hysteropexy. Chu et al. [10] reported an exposure rate of 3.8% (2 of 52 patients) after vaginal hysteropexy and a rate of 13% (5 of 39 patients) after vaginal hysterectomy, both using anterior and posterior mesh. The only study that used the abdominal approach [11] showed a higher incidence of mesh exposure with hysterectomy (Fig. 8).
Dyspareunia
Four studies evaluated the postoperative incidence of dyspareunia in a total of 333 patients [14, 17,18,19]. There was no difference in the RR for dyspareunia between techniques that preserve or remove the uterus (RR 0.79, 95% CI 0.30–2.08; p = 0.63), nor in the analyses combining surgical techniques and routes (Fig. 9).
Malignant neoplasia
None of the included studies reported the occurrence of uterine cancer.
Quality of life
None of the included studies reported quality of life by means of validated instruments.
Discussion
Severe uterine prolapse is classically treated by removing the uterus with concomitant pelvic reconstruction, but the evolution of anatomical knowledge and surgical techniques make the need for hysterectomy questionable. Also, women are more likely to prefer uterine preservation if its removal is not necessary [30]. The aim of this systematic review and meta-analysis was to address this important and relevant clinical topic for both clinicians and patients. In the surgical management of POP, reoperation is performed mainly for prolapse recurrence that is commonly associated with an unsuccessful outcome [2, 17]. This meta-analysis did not demonstrate that hysterectomy was significantly associated with a lower rate of recurrence of uterine prolapse, but there was a clear tendency for hysterectomy to be associated with a lower rate in the majority of the studies included, even with the different techniques used in the studies. Attention should be given to these findings since they may be of clinical relevance despite not being statistically significant.
Interestingly, when hysterectomy or hysteropexy were both performed vaginally with native tissue, removing the uterus resulted in a significantly lower rate of recurrence of uterine prolapse, independent of the technique used for fixation of the apical defect. This finding was not demonstrated with the use of transvaginal mesh. If vaginal hysterectomy is planned as part of reconstructive surgery, techniques using native tissue should be the optimal choice. In contrast, it is still not clear whether the use of a synthetic mesh is preferred when vaginal hysteropexy is the option.
We expected a higher rate of recurrence of apical prolapse in patients who received vaginal hysterectomy and reconstructive surgery with native tissue than in those undergoing abdominal hysteropexy, since attachment to the sacrum by mesh interposition is considered the gold standard technique to restore the apical compartment. However,, this meta-analysis did not show a lower rate of recurrence with hysteropreservation even using this procedure.
Although the statistical analysis showed that the rate of reoperation but not the rate of recurrence was lower with hysterectomy, the forest plots of both outcomes (Figs. 3 and 4) showed similar behavior patterns, indicating that recurrence of POP is directly related to reoperation. It is important to highlight that the criterion of recurrence concerns apical prolapse, and reoperation concerns any vaginal compartment. While we believe that the majority of the revision procedures were performed to repair apical prolapse, the included studies were not precise about which compartments were affected at the time of the revision.
As expected, hysteropreservation techniques yielded average operative times and blood loss similar to those usually obtained with procedures requiring less dissection. This finding is particularly relevant in women at high risk of recurrence in whom perioperative morbidity should be avoided or reduced to a minimum. Several authors have suggested that hysteropreservation is preferable when using mesh to reduce the risk of mesh exposure [31,32,33], but we were not able to confirm this finding in our study. These patients might be followed for longer since exposure may occur as a late complication. Unfortunately, quality of life evaluated by validated instruments was not reported by the authors. Further studies are required to address subjective outcomes properly.
A history of cervical or uterine abnormalities, such as abnormal uterine bleeding, polyps, fibroids or cancer, is an important and well-established factor in the choice between hysteropreservation and hysterectomy [3]. There were no reports of malignant uterine disease in the studies included in this meta-analysis. The follow-up times may not have been long enough for conclusions to be drawn about the risk of preserving the uterus in this population.
Our study addressed a subject still not well explored. We included 11 randomized trials and prospective comparative cohort studies with a large sample size. We compared hysteropreservation and hysterectomy in general independent of the technique, the route of access (vaginal, abdominal or laparoscopic) or the combination of procedures. Analysis of forest plots did not show important differences in outcomes between the randomized controlled trials and nonrandomized studies, so the potential bias from including nonrandomized studies can be considered low. We acknowledge that some biases are unavoidable when performing meta-analyses, especially those evaluating surgical treatments. There are too many inherent variables related to individual characteristics, surgeons’ preferences and skills, the combination and choice of multiple procedures required to reconstruct the pelvic floor other than those involved in the treatment of the uterine prolapse itself, that prevent two treatments being perfectly controlled. Care must be taken in interpreting these results.
In an attempt to decrease the biases and narrow our evaluation, we also analyzed subgroups of the included studies to compare surgical techniques and/or different approaches such as using or not using mesh, and vaginal or abdominal routes. Some specific conclusions can be drawn from this analysis. We conclude that overall the rate of recurrence of uterine prolapse is not lower but the rate of reoperation for POP is lower with hysterectomy. The rate of recurrence of uterine prolapse following vaginal hysterectomy is significantly lower than following vaginal hysteropexy, independent of the technique with native tissue used to repair the apical defect. Operative time is shorter and blood loss is less with hysteropreservation.
We believe that this study contributes to the still unsettled debate as to whether to remove or retain the uterus during prolapse repair. Additional studies and longer follow-up will help arrive at definite conclusions on this matter.
References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6.
Detollenaere RJ, den Boon J, Stekelenburg J, et al. Treatment of uterine prolapse stage 2 or higher: a randomized multicenter trial comparing sacrospinous fixation with vaginal hysterectomy (SAVE U trial). BMC Womens Health. 2011;11:4.
Kow N, Goldman HB, Ridgeway B. Management options for women with uterine prolapse interested in uterine preservation. Curr Urol Rep. 2013;14:395–402.
Hefni M, El-Toucky T, Bhaumik J, Katsimanis E. Sacrospinous cervicocolpopexy with uterine conservation for uterovaginal prolapse in elderly women: an evolving concept. Am J Obset Gynecol. 2003;188:645–50.
Wilcox LS, Koonin LM, Pokras R, Strauss LT, Xia Z, Peterson HB. Hysterectomy in the United States. Obstet Gynecol. 1994;83:549–55.
Thomas AG, Brodman ML, Dottino PR, Bodian C, Friedman F Jr, Bogursky E. Manchester procedure vs. vaginal hysterectomy for uterine prolapse. A comparison. J Reprod Med. 1995;40:299–304.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:332–9.
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association IUGA/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26.
Higgins JPT, Green S (editors). Cochrane handbook for systematic reviews of interventions, version 5.1.0. The Cochrane Collaboration; 2011. www.cochrane-handbook.org. Accessed 23 Jul 2017.
Chu LC, Chuang FC, Kung FT, Huang KH. Comparison of short-term outcomes following pelvic reconstruction with Perigee and Apogee systems: hysterectomy or not? Int Urogynecol J. 2012;23(1):79–84.
Costantini E, Mearini L, Bini V, Zucchi A, Mearini E, Porena M. Uterus preservation in surgical correction of urogenital prolapse. Eur Urol. 2005;48:642–9.
Costantini E, Porena M, Lazzeri M, Mearini L, Bini V, Zucchi A. Changes in female sexual function after pelvic organ prolapse repair: role of hysterectomy. Int Urogynecol J. 2013;24:1481–7.
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Koops SES. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descensus: a randomized study. Int Urogynecol J. 2010;21:209–16.
Neuman M, Lavy Y. Conservation of the prolapsed uterus is a valid option: medium term results of a prospective comparative study with the posterior intravaginal slingoplasty operation. Int Urogynecol J. 2007;18(8):889–93.
Roovers JPWR, van der Vaart CH, van der Bom JG, van Leeuwen JHS, Scholten PC, Heintz APM. A randomised controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function. BJOG. 2004;111:50–6.
Rahmanou P, Price N, Jackson SR. Laparoscopic hysteropexy versus vaginal hysterectomy for the treatment of uterovaginal prolapse: a prospective randomized pilot study. Int Urogynecol J. 2015;26:1687–94.
Rosen DMB, Shukla A, Cario GM, Carlton MA, Chou D. Is hysterectomy necessary for laparoscopic pelvic floor repair? A prospective study. J Minim Invasive Gynecol. 2008;5(6):729–34.
Carramão S, Auge APF, Pacetta AM, et al. A randomized comparison of two vaginal procedures for the treatment of uterine prolapse using polypropylene mesh: hysteropexy versus hysterectomy. Rev Col Bras Cir. 2009;36(1):65–72.
Jeng CJ, Yang YC, Tzeng CR, Shen J, Wang LR. Sexual functioning after vaginal hysterectomy or transvaginal sacrospinous uterine suspension for uterine prolapse. J Rep Med. 2005;50(9):669–74.
Huang LY, Chu LC, Chiang HJ, Chuang FC, Kung FT, Huang KH. Medium-term comparison of uterus preservation versus hysterectomy in pelvic organ prolapse treatment with Prolift™ mesh. Int Urogynecol J. 2015;26(7):1013–20.
de Boer TA, Milani AL, Kluivers KB, Withagen MI, Vierhout ME. The effectiveness of surgical correction of uterine prolapse: cervical amputation with uterosacral ligament plication (modified Manchester) versus vaginal hysterectomy with high uterosacral ligament plication. Int Urogynecol J. 2009;20(11):1313–9.
Thys ST, Coolen AL, Martens IR, et al. A comparison of long-term outcome between Manchester Fothergill and vaginal hysterectomy as treatment for uterine descent. Int Urogynecol J. 2011;22:1171–8.
Bedford ND, Seman EI, O’Shea RT, Keirse MJNC. Effect of uterine preservation on outcome of laparoscopic uterosacral suspension. J Minim Invasive Gynecol. 2013;20(2):172–7.
Fedorkow DM, Kalbfleisch RE. Total abdominal hysterectomy at abdominal sacrovaginopexy: a comparative study. Am J Obstet Gynecol. 1993;169(3):641–3.
Bai SW, Kim EH, Shin JS, Kim SK, ParK KH, Lee DH. A comparison of different pelvic reconstruction surgeries using mesh for pelvic organ prolapse patients. Yonsei Med J. 2005;46(1):112–8.
Romanzi LJ, Tyagi R. Hysteropexy compared to hysterectomy for uterine prolapse surgery: does durability differ? Int Urogynecol J. 2012;23:625–31.
Marschalek J, Trofaier ML, Yerlikaya G, et al. Anatomic outcomes after pelvic organ prolapse surgery comparing uterine preservation with hysterectomy. Eur J Obstet Gynecol Reprod Biol. 2014;183:33–6.
Shi RX, Sun HT. Total pelvic floor reconstruction versus transvaginal hysterectomy for pelvic organ prolapse: a retrospective cohort. Clin Exp Obstet Gynecol. 2014;41(3):323–7.
Iliev VN, Andonova IT. Uterus preserving vaginal surgery versus vaginal hysterectomy for correction of female pelvic organ prolapse. Pril (Makedon Akad Nauk Umet Odd Med Nauki). 2014;35(1):243–7.
Korbly NB, Kassis NC, Good MM, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):470.e1–e6.
Jirschele K, Seitz M, Zhou Y, Rosenblatt P, Culligan P, Sand P. A multicenter, prospective trial to evaluate mesh-augmented sacrospinous hysteropexy for uterovaginal prolapse. Int Urogynecol J. 2015;26(5):743–8.
Kovac SR, Cruikshank SH. Successful pregnancies and vaginal deliveries after sacrospinous uterosacral fixation in five of nineteen patients. Am J Obstet Gynecol. 1993;168:1778–86.
Gamble T, Aschkenazi S, Nguyen A, et al. Bilateral, graft-augmented sacrospinous hysteropexy, anatomic and functional outcomes at one year. J Pelvic Med Surg. 2008;14:213–352.
Acknowledgements
We thank Vinícius Fernando Calsavara who helped with the statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
None.
Electronic supplementary material
ESM 1
(DOCX 129 kb).
Rights and permissions
About this article
Cite this article
de Oliveira, S.A., Fonseca, M.C.M., Bortolini, M.A.T. et al. Hysteropreservation versus hysterectomy in the surgical treatment of uterine prolapse: systematic review and meta-analysis. Int Urogynecol J 28, 1617–1630 (2017). https://doi.org/10.1007/s00192-017-3433-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3433-1