Abstract
Introduction and hypothesis
This study aimed to determine the prevalence of urinary incontinence (UI), fecal incontinence (FI), and pelvic organ prolapse (POP) 3–5 years after the first pregnancy and their associated risk factors.
Methods
We assessed 506 women using the Pelvic Floor Distress Inventory (PFDI) and the Pelvic Floor Impact Questionnaire (PFIQ). Maternal characteristics and obstetric data were analyzed using descriptive analysis, independent sample t test, chi-squared test, and logistic regression.
Results
The prevalence of UI, FI, and POP, respectively, at a mean of 43 months after first delivery was 40.8, 6.6, and 10.2% following vaginal delivery (VD) and 22.7, 4.5, and 4.5% following cesarean section (CS). Stress urinary incontinence (SUI) was reported by more women following VD than CS (38.7 vs 22.4%, P = 0.010). Compared with 8 weeks’ postpartum, more women reported SUI at this later follow-up visit (40.1 vs 19.5%, P < 0.001), but fewer reported FI. More women who had an instrumental delivery reported symptoms of POP compared with those who had a normal VD. Higher body weight and weight gain from first trimester were risk factors of SUI [odds ratio (OR) 1.03] and urge urinary incontinence (UUI) (OR 1.18), respectively. Women who delivered vaginally had higher PFDI subscales scores.
Conclusions
VD increased UI risk. Higher body weight and weight gain from first trimester were risk factors for SUI and UUI, respectively. More women reported symptoms of POP following an instrumental delivery than those who had a normal VD.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Pelvic floor disorders impair quality of life and comprise a wide variety of interrelated clinical conditions, such as pelvic organ prolapse (POP), urinary incontinence (UI), and fecal incontinence (FI), which commonly coexist [1, 2]. There is evidence that vaginal delivery and/or pregnancy lead to some form of pelvic floor disorder (PFD). The estimated prevalence of UI postdelivery is between 16 and 40% [3, 4] and FI 5–22% from soon after to 3–4 years after delivery [5]. A recent study showed UI persists in about three quarters of women 12 years postdelivery, and almost half the patients who reported FI at 3 months postdelivery still reported it at 12 years [6, 7].
Many studies have focused on the effect of vaginal delivery (VD) shortly after delivery [8, 9]. We previously reported the prevalence of postnatal stress UI (SUI), urge UI (UUI), and FI was 26, 8.2, and 4.0%, respectively, 1 year after delivery [10].
Long-term data on PFDs in Chinese women is limited, and differences in pelvic connective tissue quality between Chinese and Caucasian women has been suggested [11]. This difference is emphasized by the observation that Asian women have significantly less pelvic organ mobility both during and after pregnancy than Caucasians [12]; also differences in obstetric practice, such as rates of cesarean section (CS), epidural analgesia, and episiotomy are well documented [13, 14]. In this longitudinal study, we determined the prevalence of PFDs in women 3–5 years after their first delivery using relevant standard questionnaires. Potential factors that may affect the prevalence of PFDs, such as maternal characteristics, obstetric parameters, and outcomes, were evaluated.
Materials and methods
This is a follow-up study of two previously published studies. The initial study recruited nulliparous women in the first trimester from August 2009 to September 2010 [15, 16]. None had symptoms of PFDs before pregnancy. The second study recruited primiparous women 1–3 days after instrumental delivery from September 2011 to May 2012 [17]; only three women reported mild SUI and one mild UUI before pregnancy [17]. Details of first delivery were recorded, and urinary, bowel, and POP symptoms and distress level were determined using the Chinese Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire (PFIQ) at postpartum 8 weeks in those studies [18, 19]. Maternal age, gestation period, baby birthweight, , and maternal body mass index (BMI) 8 weeks postpartum were comparable between studies, as were types and indication of instrumental delivery.
From 1 July 2013 to 31 December 2014, women from the two previous studies were invited to join this study, a follow-up appointment was arranged, and written consent was obtained. Women completed the Chinese-validated PFDI and PFIQ, which has demonstrated responsiveness [19], to assess urinary, bowel, and POP symptoms and distress level [2, 18]. Demographic data sheets were used to collect information such as current body weight, subsequent delivery information, if any (mode of delivery, epidural anesthesia, episiotomy, infant birth weight). Exclusion criteria were those who were pregnant at the time of invitation or within 6 months after a delivery, and those who had unrelated pelvic floor injury. If women were unable to attend the follow-up, they were invited to return the data sheet, PFDI, and PFIQ by mail.
A response of yes to PFDI questions 20–22 regarding urine leakage related to coughing, sneezing, or laughing, and physical exercise such as walking, running, aerobics, lifting, or bending over, were regarded as showing the presence of SUI. A response of yes to PFDI question 19 regarding urine leakage associated with a feeling of urgency was regarded as the presence of UUI. Mixed UI (MUI) was defined as the presence of both SUI and UUI; any UI was defined as the presence of either SUI or UUI. In addition, a response of yes to PFDI questions 38–40 regarding lose stool beyond one’s control if the stool is well formed, loose, or liquid were regarded as symptoms of FI with solid or loose stool, respectively. Losing gas from the rectum beyond one’s control was regarded as flatus incontinence. Finally, a response of yes to questions 4–5 regarding sensation of bulging or protrusion from the vaginal area or having a bulge or something falling out that one can see or feel in the vaginal area were regarded as symptoms of prolapse [18, 19]. For women who attended the visit, POP, if any, was assessed using the Pelvic Organ Prolapse Quantification (POP-Q) system [20].
Terminology in this manuscript follows the International Urogynecological Association (IUGA)/International Continence Society (ICS) Joint Report on Terminology for Female Pelvic Floor Dysfunction [21]. Investigators were blinded to PFDI data until the study was completed. Subsequent delivery information was cross-checked from computerized central medical records. Delivery mode was defined as VD, including normal spontaneous delivery (NSD) and instrumental delivery; and CS, including elective CS (ElCS) prior to labor onset and emergency CS (EmCS) after labor onset. All women were taught and then encouraged to perform pelvic floor exercise (PFE) after their first delivery; they were regarded as performing if practicing at least twice per week. [10].
Sample size calculation
There were 645 potential participants for this follow-up study. Assuming that the prevalence of FI after delivery (which is the least common PFD ) is 5%; accepted error 3%, 403 participants assuming 70% response rate: at least 575 respondents are required.
Statistical analysis
Descriptive analysis was used to study prevalence of different types of PFDs. Indices measured in two groups were compared using the independent sample t test. For comparison of frequencies, chi-square test and chi-square test for trend were used, where appropriate. Logistic regression was used to assess factors impacting PFDs: infant birth weight and head circumference; duration of second-stage labor; delivery mode. P < 0.05 was considered statistically significant. PFDI and PFIQ scores were compared using Mann–Whitney U test.
Ethics approval
Ethics approval for the study was granted by the local institutional ethics committee (CRE-2013.332).
Results
For this study, 645 women were invited; 590 responded, 506 (78.4%) agreed to participate, 485 (75.2%) attended the follow-up, and 21 (3.3%) replied by mail. All pregnancies were singleton pregnancies: for the first pregnancy, all delivered ≥37 weeks; for the second pregnancy nine (5.1%) delivered <37 weeks. Mean age at delivery was 30.6 ± 3.8 years; mean BMI at first trimester of first pregnancy was 21.03 ± 2.9 kg/m2, and current mean BMI was 22.0 ± 3.7 kg/m2. Mean duration from first delivery to the follow-up or return of the questionnaire was 42.8 (31.8–65.5) months. There was no significant difference in the age, BMI at recruitment, current BMI, height, parity, or birth weight of the heaviest infant between mail-in or physical follow-up groups.
For the first delivery, 178 (35.2%) had a NSD, 218 (43.1%) vacuum extraction (VE), 42 (8.3%) forceps delivery, 12 (2.3%) ElCS, and 56 (11.1%) EmCS. Among those who had a VD, 427 (97.4%) had a left mediolateral episiotomy; 102 (23.2%) had a first- or second-degree tear, and five (1.1%) had a third-degree tear. Of those who had an EmCS, two had a second-stage CS (3.6%), with no attempt of instrumental delivery. By the time of this study, 174 had given birth again: NSD, VE, forceps delivery, ElCS, and EmCS were 136 (78.6%), four (2.3%), two (1.2%), 26 (15%), and six (3.4%), respectively. Four women had a third delivery (2 NSD, 1 VE, 1 EmCS). Episiotomy rate for the second delivery was 30.9%, and no third- or fourth-degree tear. In all, 426 women had one or more VD, 66 CS, and 14 had one VD and one CS. Among those who had a VD in the first pregnancy, 172 had NSD, 211 a VE, and 44 forceps.
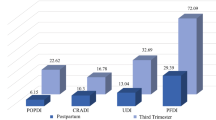
The prevalence of UI, FI, and POP symptoms according to parity and delivery mode are listed in Fig. 1. In primiparous women, significantly more women reported SUI (40.1 vs 24.4% P = 0.045) and any UI (42.9 vs 24.4%, P = 0.019) in the VD compared with the CS group. There is a trend to higher prevalence for UUI, MUI, FI, and POP in the VD compared with the CS group, but it did not reach statistical significance. Among multiparous women, there is a trend of higher prevalence of SUI, UUI, MUI, any UI, FI, and POP in VD compared with the CS group; however, none reached statistical significance. When comparing women with a prior VD to those with a prior CS, significantly more women reported SUI (38.7 vs 22.4% P = 0.010) and any UI (40.8 vs 22.4%, P = 0.04). When comparing one VD with two or more VDs, there was a higher prevalence of all PFD symptoms following one VD, but it only reached statistical significance for POP (12.3 vs 7.2%, P = 0.016). In women with two or more CS, four (19.0%) reported SUI, with no difference as compared to the group with one CS.
Significantly more women who had ever delivered by VE or forceps reported symptoms of POP than those with NSD [NSD only, 10 (5.8%) vs VE ever, 28 (13.3%) vs forceps ever, 8 (18.2%); P = 0.016]. There was a tendency toward more women reporting SUI or UI or flatal incontinence if they ever had a forceps delivery compared with NSD or ever VE; however, these did not reach statistical significance. There was no statistical difference in the prevalence of UI, FI, and POP between having an episiotomy in first or second delivery and having had no episiotomy. Prevalence of UI, FI, and POP 8 weeks after delivery and at this follow-up study is shown in Table 1. Among women who had one VD, significantly more reported SUI (40.1 vs 19.5%, P < 0.001) and any UI (42.9 vs 19.5%, P < 0.001), but fewer reported FI (7.0 vs 8.4%, P < 0.001) at this follow-up compared with 8 weeks. In women with two or more VDs, significantly more reported SUI (35.3 vs 22.3%, P < 0.001) and any UI (36.0 vs 22.3%, P = 0.009), but fewer reported MUI (7.2 vs 13.7%, P = 0.003) and FI (5.0 vs 8.6%, P = 0.009) compared with 8 weeks. In women with one or more CS, there was a trend to more reports of SUI and any UI at the current follow-up, which did not reach statistical significance. There was no difference in FI or POP (Table 1).
The association of UI, FI, and POP with various factors —maternal age, BMI or weight at first trimester of first pregnancy, current body weight and BMI, weight gain since first trimester, body height, gestation at delivery; heaviest infant’s birth weight, infant’s head circumference, duration of labor, and duration of second stage of labor—were evaluated. Body weight, BMI, and weight gain were associated with symptoms of UI. For SUI, only higher current body weight [odds ratio (OR) 1.18, 95% confidence interval (CI) 1.01–1.37, P = 0.035] was an independent risk factor after multivariate analysis and the results are shown in Table 2. More weight gain since first trimester was the only risk factor for UUI (OR 1.33, 95% CI 1.05–1.72, P = 0.019) and MUI (OR 1.41, 95% CI 1.08–1.84, P = 0.011).
PFDI Urogenital Distress Inventory (UDI) score (14.2 vs 19.2, P = 0.006), PFDI Pelvic Organ Prolapse Distress inventory (POPDI) score (18.8 vs 25.8, P = 0.002), and PFDI Colorectal–Anal Distress Inventory (CRADI) scores (31.7 vs 36.6, P = 0.025) were statistically lower in women who had two or more compared with one VD. PFIQ and PFDI scores between prior VD only and prior CS only women did not reach statistical significance.
Significantly more women who reported UI had performed PFE (SUI 55 vs 33%, P = 0.001, UUI 22 vs 8%, P = 0.001, MUI 22 vs 5%, P < 0.001, any UI 55 vs 35%, P < 0.001).
Discussion
In this follow-up study, the prevalence PFD symptoms was assessed 43 months after first delivery. UI among women who had one or more VD was 36–42%, which was comparable with the 37.9% reported in MacArthur et al.’s 12-year longitudinal study in which most participants (95.7%) were non-Asians [6].
In our study, SUI prevalence was higher at 43 months than at 8 weeks postpartum, but not for UUI or MUI. This suggests that the pregnancy and the delivery process might have some long-lasting effect on the mechanism underlying SUI and that other factors, such as increasing age or body weight may be important. Many previous studies reported VD as a risk factor for postpartum UI or SUI [8, 9, 22, 23]. In our study, VD was a risk factor for SUI but not for UUI or FI at 43 months.
Conversely, we found that the prevalence of FI and flatal incontinence decreased at 43 months compared with at 8 weeks. MacArthur et al. reported persistent FI at 12 years was 6%, comparable with the prevalence of 7% in our study population, although there was a low incidence of third-degree tear in our study [7]. The prevalence of flatal incontinence in our population was higher, however, at 24.0%; but this rate was already significantly less compared with the rate of 33% at 8 weeks. Whether this may be due to consequences of episiotomy requires further evaluation. However, among those who reported flatal incontinence, only one reported it as being severe.
POP prevalence was 10.1%, which is comparable with Volløyhaug et al.’s cross-sectional study at 15–23 years after first delivery [24]. In our study, POP prevalence was higher at 8 weeks than at 43 months. This did not reach statistical significance following one VD but was statistically significant following two or more vaginal deliveries. The prevalence of POP was also higher in those who had 1 VD compared to those who had 2 or more vaginal deliveries, this result was surprising, as other studies have reported an increasing number of vaginal births as a risk factor for POP [25–27]. We have no good explanation, and a longer follow-up is needed.
VD is a well-demonstrated risk factor for UI, FI, and POP [5–7, 23–28]. In the study we report here, there was a trend to higher UI, FI, and POP in women with VD compared with CS, although it reached statistical significance for SUI and any UI only. There was a higher prevalence of UI and FI in women with two or more VD compared with all CS, which did not reach statistical significance. This might be due to the small number of women who delivered by CS only.
Multiparity is also a reported risk factor for UI and FI [6, 9]. However, it was not demonstrated in our study, irrespective of parity. Surprisingly, prevalence of UI and POP was higher in women with one VD compared with women with two or more VD. We have no good explanation for these findings. One possibility might be that women are reluctant to have a second pregnancy due to the bothersome symptoms of PFDs. The significantly higher PFDI UDI, PFDI CRADI, and PFDI POPDI scores in this group support this theory. A longer follow-up and more research will be needed to further explore the subject.
The prevalence of UI, FI, and POP was higher in women who had a prior instrumental delivery compared with women who did not. Instrumental delivery has been reported as risk factor for UI, FI, and POP [7, 8, 17, 29, 30]. Forceps delivery, in particular, has been identified as a major contributor to PFDs [29]. The prevalence of UI, FI, and POP was highest in the group who ever had forceps delivery, with the prevalence of UI being significantly higher compared with NSD only (54.5 vs 38.9%). Arya et al. showed UI decreased significantly from 2 weeks to 1 year in NSD and VE groups but not in the forceps group [8]. The prevalence of FI in the forceps group was 9.1%. MacArthur et al. also demonstrated that women who had one or more forceps deliveries are more likely to have persistent FI, with a prevalence of 6% at 12 years [7]. POP prevalence was also significantly higher for forceps than NSD (18.2 vs 5.8%). This is comparable with Trutnovsky et al., who found the highest prevalence of POP in women with at least one forceps delivery [30].
We identified maternal BMI at first trimester as a risk factor for UI in our previous study [10] and it remained so for UUI and MUI at 43 months. Higher current body weight was associated with SUI, UUI, and MUI, which is comparable with other studies [4, 6]. This is a modifiable factor, and better educating women can potentially reduce this risk.
Women who ever had VD only generally had higher PFDI and PFIQ subscales scores, indicating greater symptom distress and a higher impact on their quality of life, although this did not reach statistical significance. Interestingly, women who had one VD had a significantly higher PFDI UDI and CRADI score compared with women who had two or more VD. The higher PFDI UDI scores may be because there were more women with one VD reporting UI compared with two or more VD (42.9 vs 36%). The prevalence of FI was also lower in the group with two or more VD (7.0 vs 5.0%). PFDI scores were generally higher in women who had only VD compared with women who only ever had CS, although this did not reach statistical significance. This could be explained by the higher prevalence in all PFDs in women who had only one prior VD compared with those who had prior CS only.
Strengths and limitations
The response rate of this prospective longitudinal observational study was 78.4%, which is high in a longitudinal study [6, 7]. The obstetric characteristic of the study population, such as age, BMI, intrapartum epidural analgesia, and episiotomy, were comparable with monthly or annual data at our institution and other published data. It is unlikely that the study sample was significantly biased, and our results can be generalized to Chinese women with similar maternal characteristics and delivering in institutions with similar obstetric practice. Standardized and validated questionnaires were used. Some participants were recruited from a previous study, which only recruited primiparous women after an instrumental delivery. The proportion of women who ever had an instrumental delivery was the largest. The number of women who had CS only was relatively low. Thus, subgroup analysis might not have adequate power. As this study addresses Chinese women only, the results may not be generalizable to other populations. Due to the high episiotomy rate, it was not possible to determine if it has an effect on pelvic floor function. This question may be answered by a randomized controlled trial.
Conclusion
The prevalence of SUI, UUI, FI, and POP at a mean of 43 months after first delivery were, respectively, 38.6, 9.8, 6.6, and 10.2% and 22.7, 4.5, 4.5, and 4.5% in women having prior VD only and prior CS only, respectively. Women who had a prior VD had an increased risk of UI. Significantly more women who had delivered by VE or forceps reported symptoms of POP when compared with NSD. Higher current body weight was associated with SUI (OR 1.03). More weight gain from first trimester was significantly associated with UUI (OR 1.18). We believe the findings from this study can provide valuable information to women when deciding their mode of delivery.
References
Jackson SL, Wber AM, Hull TL, et al. Faecal incontinence in women with urinary incontinence and pelvic organ prolapse. Obstet Gynecol. 1997;89:423–7.
Barber MD, Kuchibhatla MN, Pieper CF, et al. Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol. 2001;185:1388–95.
Rortveit G, Daltveit AK, Hannestad YS, et al. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348:900–7.
Gyhagen M, Bullarbo M, Nielsen TF, et al. The prevalence of urinary incontinence 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG. 2013;120:144–51.
Schraffordt ES, Oostvolgel VHAM, HJM. Anorectal symptoms after various modes of vaginal delivery. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:244–9.
MacArthur C, Wilson D, Herbison P, et al. Prolong study group. Urinary incontinence persisting after childbirth: extent, delivery history, and effects in a 12-year longitudinal cohort study. BJOG. 2016;123:1022–9.
MacArthur C, Wilson D, Herbison P, et al. Prolong study group. Faecal incontinence persisting after childbirth: a 12 year longitudinal study. BJOG. 2013;120:169–79.
Arya LA, Jackson ND, Myers DL, et al. Risk of new onset urinary incontinence after forceps and vacuum delivery in primiparous women. Am J Obstet Gynecol. 2001;185:1318–23. discussion 1323–4.
Obioha KC, Ugwu EO, Obi SN, et al. Prevalence and predictors of urinary/ anal incontinence after vaginal delivery: prospective study of Nigerian women. Int Urogynecol J. 2015;26:1347.
Chan SS, Cheung RY, Yiu KW, et al. Prevalence of urinary and fecal incontinence in Chinese women during and after their first pregnancy. Int Urogynecol J. 2013;24:1473–9.
Howard D, DeLancey JO, Tunn R, et al. Racial differences in the structure and function of the stress urinary continence mechanism. Obstet Gynecol. 2000;95:713–7.
Dietz HP. Do Asian women have less pelvic organ mobility than Caucasians? Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:250–3.
Territory-wide Obstetrics and Gynaecology Audit. Hong Kong College of Obstetricians & Gynaecologists; 2004.
Gossett DR, Su RD. Episiotomy practice in a community hospital setting. J Reprod Med. 2008;53:803–8.
Chan SS, Cheung RY, Yiu KW, et al. Pelvic floor biometry during first singleton pregnancy and the relationship with symptoms of pelvic floor disorders: a prospective observational study. BJOG. 2014;121:121–9.
Chan SS, Cheung RY, Yiu KW, et al. Pelvic floor biometry of Chinese primiparous women 1 year after delivery: a prospective observational study. Ultrasound Obstet Gynecol. 2014;43:466–74.
Chung MY, Wan OY, Cheung RY, et al. The prevalence of levator ani muscle injury and health-related quality of life in primiparous Chinese women after instrumental deliveries. Ultrasound Obstet Gynecol. 2015;45:728–33.
Chan SS, Cheung RY, Yiu AK, et al. Chinese validation of Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire (PFIQ). Int Urogynecol J. 2011;22:1305–12.
Chan SS, Cheung RY, Lai BP, et al. Responsiveness of the Pelvic Floor Distress Inventory and Pelvic Floor Impact Questionnaire in women undergoing treatment for pelvic floor disorders. Int Urogynecol J. 2013;24:213–21.
Bump RC, Mattiasson A, Bo K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecologic Association (IUGA) / International Continence Society (ICS) joint report on terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26.
Serati M, Salvatore S, Khullar V, et al. Prospective study to assess risk factors for pelvic floor dysfunction after delivery. Acta Obstet Gynecol Scand. 2008;87:313–8.
Zhu L, Li L, Lang J, et al. Prevalence and risk factors for peri- and postpartum urinary incontinence in primiparous women in China: a prospective longitudinal study. Int Urogynecol J. 2012;23:563–72.
Yang X, Zhang HX, Yu HY, et al. The prevalence of fecal incontinence and urinary incontinence in primiparous postpartum Chinese women. Eur J Obstet Gynecol Reprod Biol. 2010;152:214–7.
Volløyhaug I, Mørkved S, Salvesen Ø, et al. Pelvic organ prolapse and incontinence 15–23 years after first delivery: a cross- sectional study. BJOG. 2015;122:964–71.
Glazener C, Elders A, MacArthur C, et al. Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG. 2013;120:161–8.
Gyhagen M, Åkervall S, Milsom I. Clustering of pelvic floor disorders 20 years after one vaginal or one cesarean birth. Int Urogynecol J. 2015;26:1115–21.
Gyhagen M, Bullarbo M, Nielsen TF, et al. A comparison of the long-term consequences of vaginal delivery versus caesarean section on the prevalence, severity and bothersomeness of urinary incontinence subtypes: a national cohort study in primiparous women. BJOG. 2013;120:1548–55.
Howard D, Makhlouf M. Can pelvic floor dysfunction after vaginal birth be prevented? Int Urogynecol J. 2016;27:1811–1815.
Trutnovsky G, Kamisan Atan I, Martin A, et al. Delivery mode and pelvic organ prolapse: a retrospective observational study. BJOG. 2016;123:1551–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the Health and Medical Research Fund (HMRF) from the Food and Health Bureau of Hong Kong SAR (Grant reference no.: 12130071).
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Ng, K., Cheung, R.Y.K., Lee, L.L. et al. An observational follow-up study on pelvic floor disorders to 3–5 years after delivery. Int Urogynecol J 28, 1393–1399 (2017). https://doi.org/10.1007/s00192-017-3281-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3281-z