Abstract
Introduction and hypothesis
The prevalence of sexual dysfunction in postmenopausal women is high. Theoretically pelvic floor muscle (PFM) strength could influence sexual function, but to date there is scant evidence on this topic. The aim of this study was to evaluate the relationship between PFM strength and sexual function in postmenopausal women. The relationship between reported urinary incontinence (UI) and sexual dysfunction was also investigated.
Methods
This was a cross-sectional study including 113 postmenopausal women. PFM strength was evaluated using vaginal manometry. Sexual function was evaluated using the Female Sexual Function Index (FSFI). A score of ≤26.5 was considered to indicate sexual dysfunction. Urinary incontinence reports were evaluated using the International Consultation on Incontinence Questionnaire-Urinary Incontinence (ICIQ-UI) Short Form. Statistical analysis was performed using Spearman’s rank correlation coefficient (ρ), the Mann–Whitney test and 95 % confidence intervals.
Results
The median age of the women was 53 years (range 42 – 65 years) and their median body mass index was 27.9 kg/m2 (range 20 – 42 kg/m2). Women without sexual dysfunction showed significantly higher PFM strength (median 41.8, range 11.3 – 94.0 cmH2O) than women with sexual dysfunction (median 30.3, range 3 – 112 cmH2O; p = 0.02). A weak correlation was found between the total FSFI score and the total ICIQ-UI score (ρ = −0.21, p = 0.03).
Conclusions
Postmenopausal women with sexual dysfunction showed lower PFM strength than women without sexual dysfunction. There was a weak correlation between urinary incontinence severity and sexual function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Female sexual function is influenced by physical, psychological, social and cultural factors. Sexual dysfunction has been defined as a disturbance in any phases of sexual response (e.g., desire/excitement, orgasm, sexual satisfaction) or the presence of pain during sexual intercourse causing personal distress or interpersonal challenges [1]. The prevalence of female sexual dysfunction is high, ranging from 38 to 85.2 % [2, 3]. Aging increases the prevalence of sexual dysfunction; however, the transitional phase after the menopause contributes to female sexual dysfunction regardless of chronological age [3, 4]. The main changes that occur in sexual function after menopause are decreased sexual desire, reduced vaginal lubrication, anorgasmia and dyspareunia [5].
Some authors have postulated different mechanisms by which pelvic floor muscle (PFM) strength may influence female sexual function. Kegel suggested that PFM weakness could contribute to the inability of a woman to achieve orgasm [6]. According to Shafik, an increase in the strength of the muscles attached to the corpus cavernosum of the clitoris could lead to increased arousal and orgasm [7]. Graber and Kline-Graber found a significantly lower pubococcygeus muscle strength in women who had anorgasmia compared with women who had orgasms [8]. Another study that included women with primary complaints of sexual dysfunction showed that moderate and strong PFM strength was associated with the highest Female Sexual Function Index (FSFI) scores [9]. However, others have found no association between sexual function and PFM strength [10, 11].
Studies have shown that after menopause, there may be decreased function of the PFM due to estrogen deficiency [12, 13]. Although postmenopausal status can be considered a risk factor for the development of sexual dysfunction, there is scant knowledge on the relationship between sexual function and PFM strength. This study aimed to evaluate the relationship between PFM strength and sexual function in postmenopausal women. The relationship between reported urinary incontinence (UI) and sexual function was also evaluated.
Materials and methods
This was a cross-sectional clinical study approved by the Research Ethics Committee of the School Health Center of the Ribeirão Preto Medical School, University of São Paulo (CSE-FMRP-USP) under protocol no. 259/CEPCSE-FMRP-USP. All women recruited for the study gave written informed consent to participate.
Participants
The study was advertised on local radio and at the School Health Center of the Ribeirao Preto Medical School at the University of São Paulo, Ribeirão Preto City. Women interested in participating in the project were asked to contact an assistant researcher to receive more information about the study at the School Health Center of the Ribeirao Preto Medical School. After receiving information and agreeing to be evaluated for eligibility screening, women who fulfilled all the inclusion criteria were included in the study.
For inclusion the women had to be heterosexual and to have been postmenopausal for a maximum of 10 years, with the criterion for postmenopausal status being cessation of menstrual cycles for more than 12 months (World Health Organization), and to be currently sexually active with intercourse. Sexual intercourse was defined as penile penetration of the vagina in the previous 4 weeks [14, 15]. Exclusion criteria were diabetes mellitus and any reported thyroid disease, intolerance of or discomfort during the examination to evaluate PFM strength, allergy to gel or latex condoms, prolapse greater than stage 1, and inability to contract the PFM as assessed by vaginal palpation.
Measurements
The ability to contract the PFM was first evaluated by digital palpation. PFM strength was evaluated using vaginal manometry (PeritronTM, Cardio-Design, Lara Victoria, Australia). Peritron has been found to have good intrarater and moderate interrater reliability [16, 17]. Before PFM measurement, the woman completed the FSFI [15] and the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) [18]. The examiner of PFM strength was blinded to the results of the FSFI and the ICIQ-UI SF. The FSFI is a self-reported 19-item questionnaire validated for the Portuguese language [15]. It covers six domains of sexual function: lubrication, arousal, desire, pain, orgasm, and global satisfaction. The total scores range between 2 and 36. The domain scores and total scores are associated with better sexual function. The use of cut-off values on the FSFI enables the identification of women with sexual dysfunction [11]. A total score of 26.5 or less is considered to indicate sexual dysfunction [19]. The ICIQ-UI SF is used to evaluate the symptoms, severity and impact of UI on quality of life. The questionnaire has been validated in the Portuguese language and shows good test–retest reliability [20]. The third question (prevalence of UI) on the ICIQ-UI SF was used to identify the presence of UI. UI was classified into four severity levels on the basis of the mean questionnaire scores according to the system proposed by Klovning et al. [21]: mild (score 1 – 5), moderate (score 6 – 12), severe (score 13 – 18), and very severe (score 19 – 21) [21]. Question 6 was used only to classify the type of UI.
The PFM was assessed by one physiotherapist at the Laboratory of Functional Evaluation of the Pelvic Floor, Ribeirão Preto Medical School. The participants were informed about PFM anatomy and function using diagrams. Digital palpation was performed with the woman in the supine position with semiflexed hips and knees. Circular closing around the palpating fingers with movement in a cranial ventral direction was considered a correct contraction [16]. Five minutes after vaginal palpation, the probe of the Peritron™ (Cardio-Design, Lara Victoria, Australia) covered with a latex condom coated with aqueous lubricating gel was inserted above the level of the hymenal ring to the full extent of the compressible portion until 1 cm of the sheath remained visible outside the vaginal introitus [17]. Three maximum voluntary contractions (MVC) were requested, with a 30-s interval between each contraction. In all measurements, the inward movement of the probe and the perineum were used as an indication that the device was recording PFM contraction correctly [16]. Cocontraction of the hip adductors and the gluteus muscle was discouraged by requesting the woman to perform the Valsalva maneuver. The mean pressure of three MVCs was used in the analysis of PFM strength.
Statistical power and analysis
The sample size to detect a difference of 8 cmH2O using the Peritron™, with a standard deviation of 15, was calculated as 108. For allocation of subjects to each group we considered the prevalence of sexual dysfunction [22] assuming a proportion around 2.5 participants with sexual dysfunction for each participant without sexual dysfunction. A statistical power of 80 % and alpha 0.05 were used (G*Power power analysis program, version 3.1.7).
The data were analyzed using SAS® software, version 9.2. The relationship between the two quantitative variables (FSFI score and ICIQ-UI SF score) was quantified using Spearman’s rank correlation coefficient (ρ). Values between 0.10 and 0.29 were considered to indicate a weak correlation, values between 0.30 and 0.49 a moderate correlation, and values between 0.50 and 1 a strong correlation [23]. Fisher’s exact test was used to compare the following variables between the groups with and without sexual dysfunction: age, body mass index (BMI), marital status, number of vaginal births, number of nulliparous women, and number of women with UI complaint. The Pearson’s chi-squared test was used to compare the use of hormone therapy between the groups. The Mann–Whitney test for independent samples was used to compare PFM strength (MVC pressure) between women with and without sexual dysfunction.
Results
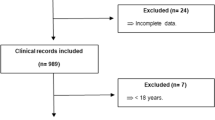
Of 154 postmenopausal women recruited, 39 were not eligible because they had not had sexual intercourse in the previous 4 weeks, and 2 were not included because they were not able to contract their PFM. Thus a total of 113 women fulfilled the eligibility criteria and were included in the study. Table 1 shows the demographics of the women with and without sexual dysfunction. There were no statistically significant differences between the groups in any of the variables.
In women with sexual dysfunction the mean FSFI scores for all domains were significantly lower than in women without sexual dysfunction (Table 2). PFM strength was significantly lower in woman with sexual dysfunction than in women without sexual dysfunction (Table 2). The median ICIQ-UI SF score was 4 (range 0 – 69.2) for the whole sample (n = 113). Table 3 shows the type and severity of UI symptoms in women with and without sexual dysfunction. There was no significant difference in the severity of UI between the two groups (p = 0.07). There was a negative weak correlation between the total ICIQ-UI SF score and the FSFI domain scores (Table 4).
Discussion
The main finding of the present study was that women without sexual dysfunction had stronger PFM. UI prevalence and severity were similar between women with and without sexual dysfunction and there was a weak negative correlation between UI severity and sexual function. It has been estimated that around 50 % of postmenopausal women have some complaints of sexual dysfunction, with the most common being hypoactive sexual desire, dyspareunia and anorgasmia [5]. The prevalence of sexual dysfunction found in this study was high, but is in agreement with previously reported rates in the range 38 % to 85.2 % [24]. In this study, the FSFI scores for all domains were lower in women with sexual dysfunction. The desire domain median score of less than 3 in the group with sexual dysfunction indicates a specific risk of hypoactive sexual desire disorder. A desire domain score of less than 3 is an established cut-off value to differentiate women with and without this condition [25].
It has been postulated that the PFM may play an important role in sexual function. The pubococcygeus and ileococcygeus muscles are responsible for involuntary contractions during orgasm [9]. Some authors have stated that an increase in PFM strength could lead to better involuntary contraction of the PFM and to increased arousal and orgasmic response [6, 7]. In the present study, women with sexual dysfunction had weaker PFM than those without sexual dysfunction. However, as the present study was cross sectional, it is not possible to establish a cause–effect relationship. A systematic review of the literature on the effects of PFM training on female sexual function did not demonstrate a clear relationship between PFM strength and sexual function [26]. In most of the eight RCTs included in this review this analysis was not performed. Conflicting results were found between one study that did not show an association between PFM strength (Brink score) and sexual function [27] and one study that showed a medium correlation between changes in sexual function and PFM strength (manometry) [28].
Few other previous cross-sectional studies have specifically evaluated the relationship between PFM strength and sexual function. Lowenstein et al. [9] conducted a retrospective chart review of 176 women with primary complaints of sexual dysfunction recruited in a tertiary urogynecological clinic who were evaluated using the FSFI (47 % had libido dysfunction, 40 % anorgasmia, 8 % dyspareunia and 5 % other complaints) [9]. Women with moderate to strong PFM had higher scores in the orgasm and arousal domains. However, the study used a scale that has not been validated for assessment of PFM strength. In a study including 40 nulliparous women, Martinez et al. found an association between higher scores on the desire domain and total FSFI scores and higher PFM strength. Although they used a vaginal manometer to evaluate muscle strength, they did not report reliability and validity data for the device. In addition, for analytical purposes, the PFM contractions measured with the perineometer were arbitrarily classified as strong or weak using a cut-off value above and below 8.8 cmH2O [29]. The mean age of the women included in the two studies discussed above was lower than of those participating in the present study, and Martinez et al. did not report the prevalence of UI or its association with sexual function [29]. Lowenstein et al. found that 45 % of women with weak PFM had UI compared with 25 % of those with moderate to strong PFM.
UI is a distressing symptom for postmenopausal women [30]. In the present study, a large number of women reported UI. Several studies have shown a higher prevalence of sexual dysfunction in women with UI [10, 31]. However, this relationship frequently disappears when confounding variables, such as menopause itself, lack of desire and pain, are controlled for. The prevalence of reported UI of 48.1 % in women with sexual dysfunction found in the present study is consistent with the prevalence range of 19 % to 50 % reported in the literature [31]. We found no significant difference in ICIQ-UI SF scores between women with and without sexual dysfunction. There was a small negative correlation between the desire, arousal, satisfaction, pain and total FSFI scores and the total ICIQ-UI SF score. This is in agreement with the findings of other studies, which have also shown lower scores in the desire, satisfaction and pain domains of the FSFI in women with incontinence than in women without incontinence [31].
Severe UI has frequently been correlated with sexual dysfunction [11]. However, most of the women in this study reported moderate UI, and this may have contributed to the weak correlation between sexual function and the impact of UI on quality of life. There was no statistically significant difference between the groups regarding severity of UI, possibly because of the small number of women with each level of severity. These results should therefore be interpreted with caution, and more research is warranted in this area.
The present study had some limitations and strengths that need to be addressed. We acknowledge that the tool used to evaluate sexual function is a screening tool used as a potential aid in the diagnosis of sexual dysfunction and does not allow a complete diagnosis of sexual dysfunction. Moreover, we did not evaluate distress and we did not have any information about the use of drugs that may have influenced sensory function. We cannot discard the possibility that women with hormone alterations leading to anovulation were included, as we used the World Health Organization criteria for postmenopause that do not include hormone levels of follicle-stimulating hormone. Women unable to contract their PFM were excluded, and these women could have had the weakest muscles, but we consider that this would not have interfered with our results as only two such women were excluded. Our study design does not allow any statement to be made as to cause and effect, and other uncontrolled variables could also have influenced sexual function in the postmenopausal women studied. However, as far as we are aware, this study is one of only a few investigating the relationship between PFM strength and sexual dysfunction in women. The study used reliable and valid instruments to evaluate both sexual function and PFM strength. In addition, a single experienced examiner conducted all the examinations.
In conclusion, this study showed that postmenopausal women without sexual dysfunction have a stronger PFM than women with sexual dysfunction. There was a weak correlation between UI severity and sexual function. Further randomized controlled trials are needed to establish the cause–effect relationships between PFM strength and sexual dysfunction and UI in postmenopausal women.
References
Clayton AH, Dennerstein L, Fisher WA, Kingsberg SA, Perelman MA, Pyke RE. Standards for clinical trials in sexual dysfunction in women: research designs and outcomes assessment. J Sex Med. 2010;7:541–560.
Jaafarpour M, Khani A, Khajavikhan J, Suhrabi Z. Female sexual dysfunction: prevalence and risk factors. J Clin Diagn Res. 2013;7(12):2877–2880.
Thomas HM, Bryce CL, Ness RB, Hess R. Dyspareunia is associated with decreased frequency of intercourse in the menopausal transition. Menopause. 2011;18(2):152–157.
Dennerstein L, Alexander JL, Kotz K. The menopause and sexual functioning: a review of the population-based studies. Annu Rev Sex Res. 2003;14:64–82.
da Silva Lara LA, Useche B, Rosa E, Silva JC, Ferriani RA, Reis RM, et al. Sexuality during the climacteric period. Maturitas. 2009;62(2):127–133.
Kegel AH. Sexual functions of the pubococcygeus muscle. West J Surg Obstet Gynecol. 1952;60(10):521–524.
Shafik A. The role of the levator ani muscle in evacuation, sexual performance and pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11(6):361–376.
Graber B, Kline-Graber G. Female orgasm: role of pubococcygeus muscle. J Clin Psychiatry. 1979;40(8):348–351.
Lowenstein L, Gruenwald I, Gartman I, Vardi Y. Can stronger pelvic muscle floor improve sexual function? Int Urogynecol J. 2010;21(5):553–556.
Baytur YB, Deveci A, Uyar Y, Ozcakir HT, Kizilkaya S, Caglar H. Mode of delivery and pelvic floor muscle strength and sexual function after childbirth. Int J Gynaecol Obstet. 2005;88(3):276–280.
Handa VL, Harvey L, Cundiff GW, Siddique SA, Kjerulff KH. Sexual function among women with urinary incontinence and pelvic organ prolapse. Am J Obstet Gynecol. 2004;191(3):751–756.
Betschart C, Mol SE, Lütolf-Keller B, Fink D, Perucchini D, Scheiner D. Pelvic floor muscle training for urinary incontinence: a comparison of outcomes in premenopausal versus postmenopausal women. Female Pelvic Med Reconstr Surg. 2013;19(4):219–224.
Rahn DD, Ward RM, Sanses TV, Carberry C, Mamik MM, et al. Vaginal estrogen use in postmenopausal women with pelvic floor disorders: systematic review and practice guidelines. Int Urogynecol J. 2015;26(1):3–13.
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208.
Pacagnella RC, Martinez EZ, Vieira EM. Construct validity of a Portuguese version of the Female Sexual Function Index. Cad Saude Publica. 2009;25(11):2333–2344.
Bø K, Sherburn M. Evaluation of female pelvic-floor muscle function and strength. Phys Ther. 2005;85(3):269–282.
Kerschan-Schindl K, Uher E, Wiesinger G, Kaider A, Ebenbichler G, et al. Reliability of pelvic floor muscle strength measurement in elderly incontinent women. Neurourol Urodyn. 2002;21(1):42–7.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–330.
Wiegel M, Meston C, Rosen R. The Female Sexual Function Index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005;31(1):1–20.
Tamanini JT, Dambros M, D’Ancona CA, Palma PC, Rodrigues NN. Validation of the “International Consultation on Incontinence Questionnaire–Short Form” (ICIQ-SF) for Portuguese. Rev Saude Publica. 2004;38(3):438–444.
Klovning A, Avery K, Sandvik H, Hunskaar S. Comparison of two questionnaires for assessing the severity of urinary incontinence: the ICIQ-UI SF versus the Incontinence Severity Index. Neurourol Urodyn. 2009;28(5):411–415.
Amidu N, Owired W, Gyasi-Sarpong C, Wood E, Quaye L. Sexual dysfunction among married couples living in Kumasi metropolis, Ghana. BMC Urol. 2011;11(3):3–7.
Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Erlbaum; 1988.
Masliza W, Daud W, Yazid Bajuri M, Shuhaila A, Hatta S, Rohaizat Hassan M, et al. Sexual dysfunction among postmenopausal women. Clin Ter. 2014;165(2):83–89.
Gerstenberger EP, Rosen RC, Brewer JV, Meston CM, Brotto LA, Wiegel M, et al. Sexual desire and the Female Sexual Function Index (FSFI): a sexual desire cutpoint for clinical interpretation of the FSFI in women with and without hypoactive sexual desire disorder. J Sex Med. 2010;7(9):3096–3103.
Ferreira CH, Dwyer PL, Davidson M, De Souza A, Ugarte JA, Frawley HC. Does pelvic floor muscle training improve female sexual function? A systematic review. Int Urogynecol J. 2015;26(12):1735–1750.
Handa VL, Whitcomb E, Weidner AC, Nygaard I, Brubaker L, Bradley CS, et al. Sexual function before and after non-surgical treatment for stress urinary incontinence. Female Pelvic Med Reconstr Surg. 2011;17:30–5.
Braekken IH, Majida M, Ellström Engh M, Bø K. Can pelvic floor muscle training improve sexual function in women with pelvic organ prolapse? A randomized controlled trial. J Sex Med. 2015;12:470–480.
Martinez CS, Ferreira FV, Castro AA, Gomide LB. Women with greater pelvic floor muscle strength have better sexual function. Acta Obstet Gynecol Scand. 2014;93(5):497–502.
Pace G, Silvestri V, Gualá L, Vicentini C. Body mass index, urinary incontinence, and female sexual dysfunction: how they affect female postmenopausal health. Menopause. 2009;16(6):1188–1192.
Salonia A, Zanni G, Nappi RE, Briganti A, Dehò F, Fabbri F, et al. Sexual dysfunction is common in women with lower urinary tract symptoms and urinary incontinence: results of a cross-sectional study. Eur Urol. 2004;45(5):642–648.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by a grant from São Paulo Research Foundation (FAPESP 2012/215239).
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
de Menezes Franco, M., Driusso, P., Bø, K. et al. Relationship between pelvic floor muscle strength and sexual dysfunction in postmenopausal women: a cross-sectional study. Int Urogynecol J 28, 931–936 (2017). https://doi.org/10.1007/s00192-016-3211-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3211-5