Abstract
Introduction and hypothesis
The objective was to assess the feedback from a quality improvement training programme to reduce obstetric anal sphincter injuries (OASIS).
Methods
Training sessions were organised that included evidence-based information on OASIS risk factors and training on models to measure perineal body length (PBL), perform episiotomies with standard and 60° fixed angle scissors (EPISCISSORS-60®), and measure post-delivery episiotomy suture angles with protractor transparencies. Feedback forms using a Likert scale (1–4) were completed and analysed. The setting was an evidence-based quality improvement programme (Strategy for Using Practical aids for Prevention of OASIS, Recording episiotomies and clinician Training [SUPPORT]) at two National Health Service (NHS) Hospitals in the UK. The participants were midwives and doctors attending the SUPPORT training programme
Results
All of the participants (100 %) would recommend the training programme to a friend or colleague. 92 % felt that the training session improved their knowledge of the impact of PBL and perineal distension and their knowledge of the relationship between episiotomy angle and OASIS “a lot” or “somewhat”.
Conclusion
Based on this feedback, we recommend the addition of the knowledge content of the SUPPORT programme to other centres providing perineal assessment and repair courses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quality improvement in healthcare involves improving patient experience and outcomes by changing providers’ behaviour. The Institute of Medicine has suggested dimensions [1] of quality care, which include safety (avoiding harm to patients from care that is intended to help them), effectiveness (providing services based on scientific knowledge that produces a clear benefit) and individualisation (providing care that is responsive to individuals’ needs).
Quality improvement approaches include understanding the risk factors leading to the problem, developing care-bundles and creating error-free processes that deliver high-quality, consistent care. Clinician engagement is also vital to the success of any interventions [2].
The Perineal Assessment and Repair Longitudinal Study (PEARLS), was a customised multi-professional training package that focused on recognition and suturing of perineal trauma. Introduction of the PEARLS has been shown to improve outcomes, with the implementation of evidence-based best practice [3], and skills scores in a multi-professional setting [4].
Currently, there are no programmes to provide knowledge on preventative measures for reducing obstetric anal sphincter injuries (OASIS). The revised Royal College of Obstetricians and Gynaecologists (RCOG) green-top guidance 29 recommends three preventative measures to reduce the risk of OASIS. These are performing episiotomies at 60° to the midline at crowning, manual perineal protection and warm perineal compresses in the second stage of labour [5].
There is a high degree of variability in mediolateral (MLE) episiotomy incisions in simulation settings and actual patients. The importance of structured instructions about the parameters for correct MLE and episiotomy cutting technique has been stressed [6]. Post-delivery suture episiotomy angles (EA) less than 30° or more than 60° carry the risk of significantly more OASIS. To reduce the risk of litigation and promote best practices, there is a need to measure the angles of episiotomies and permanently record this information in a permanent way in the patient’s notes. Perineal body length (PBL) is defined as the distance from the lower edge of the vagina to the anus. The incidence of OASIS can be as high as 40 % in women with a short PBL (less than 25–30 mm) compared with those with a normal PBL (37–41 mm) [7–13]. Measurement of PBL would be the first step in identifying women who are at a higher risk of OASIS.
Although the Cochrane Database does not show any benefits to it, manual perineal protection (MPP), with a clear description of the techniques involved, has been shown to reduce OASIS [14, 15].
The identified unmet clinical needs for reducing OASIS during childbirth were:
-
As a practical aid to enable cutting an episiotomy at 60°.
-
The need to measure PBL during the first stage of labour
-
The need to actively monitor OASIS outcomes in women with a short PBL
-
To provide knowledge of the latest evidence in perineal anatomy and changes at different points during childbirth and the post-partum period; relationship between the episiotomy angles and OASIS, discussion of the different components of manual perineal protection (controlled delivery of the fetal head and perineal digital support), and weightage of the known risk factors for OASIS, including parity, forceps, ventouse, occipito-posterior, birth weight and previous OASIS
Hence, a quality improvement programme was devised, named the Strategy for Using Practical aids for Prevention of OASIS, Recording episiotomies and clinician Training (SUPPORT©) programme, which incorporated all the above unmet needs.
Applications were successfully made to NHS England’s innovation fund for implementation of the programme by two NHS hospitals. A time series analysis will be performed to track the impact of the interventions. We present the results of the feedback obtained from clinicians who attended the SUPPORT training sessions at both hospitals.
Materials and methods
Two English NHS Hospitals participated. A session was organised that included evidence-based information on OASIS risk factors and training on models to measure PBL, perform episiotomies with standard and 60° fixed angle scissors (EPISCISSORS-60®), and measure post-delivery episiotomy suture angles with protractor transparencies. The sessions were open-ended, included a power-point presentation and encouraged questions at every step. A feedback form with a Likert scale (1–4) was used.
“High-fidelity” simulations that involved a full practice of the situation or environment were used to support healthcare improvements. An episiotomy cutting training model was adapted from Silf et al. [6] using the Keele and Staffs episiotomy trainer (Limbs and Things, Bristol, UK). It is designed to provide a realistic representation of the distended perineum at crowning with 7 cm of the fetal head seen. Clinicians were encouraged to cut as per their normal practice. Most clinicians inserted 1–2 fingers of the non-dominant hand between the fetal head and perineum while inserting the scissor blades. In some cases, clinicians made the cuts when the fetal head was being pushed from behind to simulate real-life circumstances. Owing to variations in the above techniques, the episiotomy incision pad was often stretched beyond its resting dimensions, leading to angular distension as well.
Clinicians were asked to cut with standard straight Mayo scissors and the EPISCISSORS-60 sequentially on different parts of the incision pads. EPISCISSORS-60 has a guide-limb that points towards the anus and is in the vertical plane. The scissor blades constantly maintain a 60° angle from the guide-limb. The flexible nature of the guide accommodates the spherical distension of the head at crowning. Data on the angles achieved with both types of scissors have been submitted for publication elsewhere.
Additional shortened sessions were conducted by the lead clinicians with junior doctors, where feedback forms were not available. The feedback form consisted of questions with Likert scale responses (“not at all”, “a little”, “somewhat” and “a lot”). Specific questions were asked about the improvement in knowledge and understanding of perineal anatomy and changes during labour, the relationship of episiotomy angles and OASIS, manual perineal protection, and risk factors for OASIS. Participants were also asked whether they would recommend the training to a friend/colleague. The questions were selected by subject experts using the Delphi method. All data were entered into Excel sheets and analysed. Fisher’s two-tailed exact test was used to compare the responses between the subgroups.
Participants were classified as follows: student midwives, midwives with <5 years’ experience, 5–10 years’ experience, >10 years’ experience. Doctors were first on call (SHO), second on call (registrar), or consultants. No ethical approval was required for the training sessions.
Results
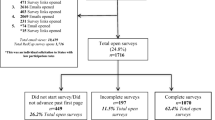
A total of 108 completed feedback forms were received. 11.1 % of the responders were doctors, 12.9 % were student midwives and 75.9 % were practising midwives. Details of responses regarding the improvement in knowledge of PBL, the relationship between episiotomy angle and OASIS, manual perineal protection and OASIS risk factors are provided in Table 1.
All the participants (100 %) would recommend the training programme to a friend or colleague. 76 % of clinicians (range 68–100 %) described “a lot” of improvement from the knowledge provided about PBL and perineal stretching during labour. Student midwives (93 %) and obstetric consultants (100 %) reported gaining most benefit. 78 % of clinicians (range 63–100 %) described “a lot” of improvement from the knowledge provided about episiotomy angle and OASIS during labour. Student midwives (100 %) and obstetric consultants (100 %) reported gaining most benefit. Only 25 % of clinicians (range 16–60 %) found the manual perineal protection component to have contributed “a lot” of knowledge improvement. Again, student midwives (50 %) and obstetric consultants (60 %) reported gaining most benefit. 53 % of clinicians (range 41–80 %) found that they obtained a significant improvement in their knowledge of risk factors for OASIS.
There were no significant differences between the highest and lowest subgroups in any of the questions (p = 0.2 perineal anatomy, p = 0.19 episiotomy angles, p = 0.07 manual perineal protection and p = 0.16 risk factors).
Discussion
To our knowledge, this is the first quality improvement programme devised to promote the prevention of OASIS. The 100 % recommendation rate was an encouraging response to the training content and delivery. We perceive this as evidence of a willingness in providers to change behaviour, and successful clinician engagement.
We believe that the components of the programme will help to prevent avoidable harm to patients by reducing human error. Although there are no robust interventions yet, an awareness of the relationship between short PBL and OASIS will help to provide care that is responsive to individuals’ needs. As such, they meet the criteria for quality improvement.
Of the participants, 92 % felt that the training session improved their knowledge of the impact of PBL and perineal distension “a lot” or “somewhat”. Although there are no proven interventions to reduce the risk of OASIS in women with short PBL, concepts discussed included manual perineal protection, elective episiotomy versus spontaneous tears, an earlier episiotomy versus late episiotomy and/or a more angled episiotomy versus a routinely angled one. An understanding of the higher risk and the importance of measuring PBL was conveyed. Perineal distension occurs 40–50 % in vertical planes, 170 % in transverse planes, and 50–100 % in angular planes. An understanding of these concepts conveyed the difference between the incision angle and suture angle of episiotomies. NICE recommends an episiotomy at an angle of 45–60°. However, they do not specify whether these are incision or suture angles [16]. 92 % felt that the training session improved their knowledge of the relationship between episiotomy angle and OASIS “a lot” or “somewhat”. Most perineal trauma workshops focus on episiotomy repair techniques. The actual angle of the episiotomy required at cutting is not advised, although the RCOG guidance 29 recommends a 60° episiotomy. Clinicians were also able to compare the angles cut on simulation models using straight Mayo scissors and the EPISCISSORS-60. 73 % felt that the training session improved their knowledge of manual perineal protection “a lot” or “somewhat”. A relatively lower number of clinicians found an improvement in their knowledge of manual perineal protection. This may be due to better existing knowledge about this subject. Alternatively, it could be due to a lack of focus in the content of the teaching. This is being addressed for future versions of the training package. 85 % felt that the training session improved their knowledge of risk factors for OASIS “a lot” or “somewhat”. Although some of the risk factors such as birth weight and nulliparity are not modifiable, it is helpful to be aware of them. East et al. [17] also included knowledge and preference for interventions such as manual perineal protection, warm perineal compresses and episiotomy in an Australian survey of midwives and doctors.
A limitation of our study was a lack of baseline data about specific aspects of knowledge contained within the training programme. Another limitation is that we have no evidence of the sustainability of the effects of the intervention, and whether there were changes in clinical practice as a result. These are the subject of an on-going time series analysis. However, the feedback suggests that there might have been very little resistance to change among individual clinicians. This, combined with the organisational willingness to provide clinicians with time off to attend these sessions and to promote the adoption of practical aids provides a good starting point for implementation of the SUPPORT programme. Laine et al. [14] have successfully demonstrated a reduction in OASIS with a care bundle implemented in Norwegian hospitals. Our quality improvement (QI) programme is similar, with additions such as angle of the episiotomy and knowledge about the impact of PBL. The PEARLS survey highlighted the inadequate implementation of evidence into practice in relation to the management of childbirth-related perineal trauma [18]. Hence, there is a need to focus on continuous quality improvement. Löwenstein et al. [19] showed that midwives can be persuaded to change their practice and that workplace protocols should be supported by evidence-based data and need to be re-evaluated periodically.
Conclusion
Quality improvement programmes to reduce the incidence of OASIS would improve the knowledge of clinicians and need to be added to current perineal assessment and repair courses. Based on the feedback received, we recommend the addition of the knowledge content of the SUPPORT programme to other centres providing perineal assessment and repair courses.
References
Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington: IOM; 2001.
Ovretveit J. Does improving quality save money? A review of the evidence of which improvements to quality reduce costs to health service providers. London: Health Foundation; 2009. p. 8.
Ismail KM, Kettle C, Macdonald SE, Tohill S, Thomas PW, Bick D. Perineal Assessment and Repair Longitudinal Study (PEARLS): a matched-pair cluster randomized trial. BMC Med. 2013;11:209. doi:10.1186/1741-7015-11-209.
Mahmud A, Morris E, Johnson S, Ismail KM. Developing core patient-reported outcomes in maternity: PRO-Maternity. BJOG. 2014;121 Suppl 4:15–9. doi:10.1111/1471-0528.12901.
Royal College of Obstetricians and Gynaecologists. Third- and fourth-degree perineal tears, management (Green-top Guideline No. 29). London: RCOG; 2015.
Silf K, Woodhead N, Kelly J, Fryer A, Kettle C, Ismail KMK. Evaluation of accuracy of mediolateral episiotomy incisions using a training model. Midwife. 2014;31:197–200.
Aytan H, Tapisiz OL, Tuncay G, Avsar FA. Severe perineal lacerations in nulliparous women and episiotomy type. Eur J Obstet Gynecol Reprod Biol. 2005;121:46–50.
Dua A, Whitworth M, Dugdale A, Hill S. Perineal length: norms in gravid women in the first stage of labour. Int Urogynecol J. 2009;20:1361–4.
Geller EJ. Perineal body length as a risk factor for ultrasound-diagnosed anal sphincter tear at first delivery. Int Urogynecol J. 2014;25:631–6.
Lai CY, Cheung HW, His Lao TT, Lau TK, Leung TY. Is the policy of restrictive episiotomy generalizable? A prospective observational study. J Matern Fetal Neonatal Med. 2009;22:1116–21.
Rizk DEE, Abadir MN, Thomas LB, Abu-Zidan F. Determinants of the length of episiotomy or spontaneous perineal lacerations during vaginal birth. Int Urogynecol J. 2005;16:395–400.
Tsai PS, Oyama IA, Hiraoka M, Minaglia S, Thomas J, Kaneshiro B. Perineal body length among different racial groups in the first stage of labour. Female Pelvic Med Reconstr Surg. 2012;18:165–7.
Walfisch A, Hallak M, Harley S, Mazor M, Shoham-Vardi I. Association of spontaneous perineal stretching during delivery with perineal lacerations. J Reprod Med. 2005;50:23–8.
Laine K, Skjeldestad FE, Sandvik L, et al. Incidence of obstetric anal sphincter injuries after training to protect the perineum: cohort study. BMJ Open 2012;2:e001649. doi:10.1136/bmjopen-2012-001649.
Naidu M, Kapoor DS, Evans S, Vinayakarao L, Thakar R, Sultan AH. Cutting an episiotomy at 60 degrees: how good are we? Int Urogynecol J. 2015;26:813–6.
National Institute for Health Care and Excellence. Intrapartum care for healthy women and babies; NICE guidelines [CG190]. London: NICE; 2014.
East CE, Lau R, Biro MA. Midwives’ and doctors’ perceptions of their preparation for and practice in managing the perineum in the second stage of labour: a cross-sectional survey. Midwifery. 2015;31:122–31.
Bick DE, Ismail KM, Macdonald S, Thomas P, Tohill S, Kettle C. How good are we at implementing evidence to support the management of birth related perineal trauma? A UK wide survey of midwifery practice. BMC Pregnancy Childbirth. 2012;12:57.
Löwenstein L, Drugan A, Gonen R, Itskovitz-Eldor J, Bardicef M, Jakobi P. Episiotomy: beliefs, practice and the impact of educational intervention. Eur J Obstet Gynecol Reprod Biol. 2005;123:179–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Rahman, N., Vinayakarao, L., Pathak, S. et al. Evaluation of training programme uptake in an attempt to reduce obstetric anal sphincter injuries: the SUPPORT programme. Int Urogynecol J 28, 403–407 (2017). https://doi.org/10.1007/s00192-016-3158-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3158-6