Abstract
Introduction and hypothesis
Jorge and Wexner devised a questionnaire for anal incontinence (AI), known as the Wexner scale (WS). Specific validated questionnaires are essential for the assessment of symptom severity. The objective was to accomplish the cultural adaptation and validation of the Portuguese version of the WS.
Methods
The WS was validated according to the international criteria. A Brazilian version was tested, including the item “I do not understand” at the end of each question. If this answer was reported at a rate higher than 15 %, the item would be considered difficult to understand and would thus be modified. The final version of the WS and the Fecal Incontinence Quality of Life (FIQL) were completed by 50 women. Convergent validity was assessed by comparing the data from the first interview of the WS with the FIQL using Spearman’s test. Reproducibility was assessed by means of a 2-week test–retest procedure using Cronbach’s alpha coefficient.
Results
In the initial version of the questionnaire, we did not obtain a response of “I do not understand” at a rate greater than 15 % and this version was considered definitive. A significant negative relationship (r = −0.63) was found between the FIQL total score and the WS. The answers obtained on the “test–re-est” questionnaires showed a significant correlation according to the intraclass correlation coefficient (ICC). A high level of internal consistency was found, as demonstrated by a Cronbach’s alpha of 0.932.
Conclusion
The Brazilian Portuguese version of the WS is a reliable, consistent, and valid instrument.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anal incontinence (AI) is defined by the International Continence Society as the complaint of involuntary loss of feces or flatus [1]. The inability to control the passage of stool or flatus can produce embarrassment, and the fear of such episodes may limit a person’s activities. The true prevalence of AI is unknown because of the constraints that hinder the approach to this problem [2–4]. Prevalence estimates for fecal or anal incontinence vary widely and range from 2.2 to 25 % [5]. The National Health and Nutrition Examination Survey (NHANES) in the United States (US) estimated that the prevalence of fecal incontinence in the non-institutionalized US population is 8.9 % of women and 7.7 % of men [6]. AI is more frequent among nursing home patients, reaching 50 % of this population [7].
Despite the large impact of AI on quality of life, affected women do not usually complain of incontinence symptoms to their physicians. Even in the setting of a pelvic floor dysfunction clinic, only 17 % of women with AI had discussed the problem with a physician; only 2.4 % of women with AI reported their symptoms before being specifically asked by means of a questionnaire [8].
There is increased scientific interest in developing a reliable and widely used instrument to evaluate AI; however, significant variation exists in the way in which these patients are assessed. There are two types of questionnaires currently in use for the evaluation of AI symptom severity. Generic questionnaires have been designed to screen large populations, but may not detect fine changes within a specific population. Disease-specific questionnaires are used to evaluate patients suffering from specific medical conditions and are therefore more sensitive to specific aspects of the disease. Specific validated questionnaires are essential for the accurate assessment of symptom severity before selecting an appropriate treatment plan [9].
Jorge and Wexner devised a disease-specific questionnaire for AI, and this questionnaire, generally known as the Wexner scale (WS), has been widely used because of its simplicity [10, 11]. In Brazil, the only validated instrument measuring the impact of AI on women’s quality of life is the Fecal Incontinence Quality of Life (FIQL). The FIQL contains 29 questions that are distributed in four domains. Therefore, it is a much more complex instrument than the WS [12]. While there is an instrument for assessing a condition-specific impact on quality of life for Portuguese speaking patients with AI, there is not yet a validated instrument for assessing condition severity. We intend to use this adapted instrument to screen for patients with AI, and will then administer FIQL to those with the condition.
Although AI is an extremely embarrassing subject for the patient, the WS is a very simple tool that can be used to address this issue. Considering the need for research in this area, we set out to accomplish the cultural adaptation and validation of the Portuguese version of WS.
Materials and methods
We asked the authors for permission to culturally adapt and validate the WS. The study was approved by the ethics committee of the Federal University of Minas Gerais. All of the patients filled out the written informed consent statement and agreed to take part in the study.
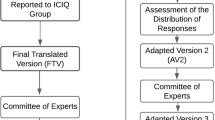
The WS instrument was translated and validated according to the international criteria proposed by Guillemin et al. [13]. Experienced native Portuguese speakers and professional translators provided the first two independent translations and then developed a single reconciled version after a harmonization meeting with the study coordinator. This first Portuguese version was back-translated by two other different linguistic experts, and the results were compared with the original US English-language instrument. No discrepancies were found between the original and back-translated versions of the questionnaire. Then, at a meeting of colon and rectum surgeons, urogynecologists and physiotherapists, a common draft of the Brazilian version was produced. One item required revision: the item, “pads” was replaced with “protector” because of the belief that male Brazilian patients would better understand the latter term.
All the patients were selected in the Urogynecology outpatient clinic of the Clinical Hospital of the Universidade Federal Minas de Gerais (Belo Horizonte, Brazil). We routinely ask all patients if they have symptoms of anal incontinence as pelvic floor dysfunctions co-occur. If the answer was yes, they were invited to participate in the study. Because many women in our sample could not read or write, all the participants were interviewed by a researcher. During the first visit, socio-demographic data, including gender, age, race, education level, marital status, and economic status were recorded. All patients were examined by a urogynecologist, and clinical data were registered.
The first version of the questionnaire was tested on 20 patients with AI. To perform this test, we included the item, “I do not understand,” at the end of each question of the scale. If this answer was reported at a rate higher than 15 %, we considered the item difficult to understand by that population, and it would thus be modified until achieving the final version of the scale in Portuguese [14].
The questionnaire consisted of five questions: three about AI (gas, liquid, and solid), a coping mechanism (pad wear), and a lifestyle question (alteration). The same scoring system described in the original questionnaire was used, and respondents were instructed to rate the frequency of stool loss, frequency of use of a coping mechanism, and the frequency of lifestyle alteration through the use of quantifiers (0 = never, 1 = rarely, 2 = sometimes, 3 = usually, 4 = always). The score was developed by summing the numerical values associated with the quantifiers. This procedure provided a single AI severity score and higher scores indicate the severity of AI. The total score on the instrument ranged from 0 (no incontinence) to 20 (complete incontinence).). We then applied the adapted WS to 50 women who were suffering from AI. They answer the final version of the WS and the FIQL.
To measure the test–retest reliability of the adapted version of the WS, a “2-week test–retest analysis” was performed. Women were asked to answer the adapted WS again 2 weeks later by telephone. Forty-nine women completed the 2-week retest. The responses from the two completed questionnaires were then analyzed.
Psychometric testing of the adapted WS was conducted using standardized procedures. Construct validity is an assessment of whether the instrument exhibits appropriate relationships with other variables or measures. In other words, it assesses whether the instrument correlates or agrees with other tests or measures of the same construct (convergent validity) and has little or no correlation or agreement with measures of different constructs (discriminant or divergent validity) [15]. In our study, convergent validity was assessed by comparing the data from the first interview of the WS with the FIQL using Spearman’s correlation test.
Reproducibility (test–retest reliability) was assessed over a 2-week interval. Test–retest reliability was evaluated using the intraclass correlation coefficient (ICC). This is a preferred measure of the strength of association for determining the stability of scores over time because it corrects for a lack of independence between the measurement intervals. The ICC ranges between 0 and 1, and the minimal acceptable level for group comparisons is 0.7 [16–18]. Internal consistency evaluates the extent to which the items on a scale are related to one another. We used Cronbach’s alpha coefficient (values of >0.70 demonstrate adequate internal consistency) [15]. Statistical analyses were performed using the Statistical Package for Social Sciences (v21.0; SPSS, Chicago, IL, USA).
Results
Sample characteristics
Seventy women were recruited to participate in this cross-sectional observational study between November 2012 and June 2013. Twenty of these women were enrolled in the translation and adaptation process, and 50 participated in the validation process. The sociodemographic data are shown in Table 1. Most of these women had concomitant urinary incontinence (84.3 %). According to the patients’ self-reported symptoms, 23.3 % had stress urinary incontinence, 20 % had urge incontinence, and 51.7 % had mixed incontinence. In the study population, only 34 % had already sought treatment for AI, and 28 % reported that a doctor had already spontaneously asked them about the symptoms of AI.
In the initial version of the questionnaire, which was tested on 20 patients, we did not obtain a response of “I do not understand” to any of the questions at a rate greater than 15 %. Thus, this version was considered definitive, and the test phase of the psychometric properties was initiated.
Psychometric testing
In the analysis of convergent validity, a significant negative relationship (r = −0.63) was found between the FIQL total score (Fig. 1) and the Portuguese-translation of the WS. Higher values of the WS score generally correlated with lower values of the FIQL questionnaire score, thus demonstrating an inverse proportional relationship. The scores of WS and FIQL are shown in Table 2.
In the test–retest phase, only one patient did not complete the second questionnaire (2 %). Reproducibility, which was assessed using the ICC after an period of 15 days, was 0.932.
The median values for scores 1 and 2 were statistically equal (p = 0.35). A high level of internal consistency was found, as demonstrated by a Cronbach’s alpha of 0.932. When each item of the questionnaire was evaluated separately, a high level of internal consistency was also demonstrated (Table 3), thus showing adequate internal reliability.
Discussion
The present study validated the linguistic and psychometric properties of the Portuguese version of the WS in Brazil. The Portuguese language, with 200 million native speakers, is the sixth most widely spoken first language in the world [19]. For this reason, and to permit the comparison of the studies performed in our country, we decided to translate and culturally adapt this important questionnaire into Brazilian Portuguese. The results of this study demonstrated that the Portuguese version of the WS has high internal consistency and test–retest reliability.
There is a scarcity of objective and specific methods in the literature for measuring the severity and the impact of AI on the quality of life. Ideally, such an evaluation should be performed quantitatively and in a reproducible manner. The instrument used must be easy to apply and understand, and there should be adequate time to administer it. The WS was chosen because it is a specific instrument that is written in easy-to-understand language. The WS addresses severity more specifically than quality of life, but it has one question about changes in lifestyle that is related to quality of life. Furthermore, the WS is widely accepted by the scientific community. Rusavy et al. conducted an international survey of the AI severity scoring systems and evaluation tools used by specialists. The primary objective of the survey was to determine which scoring systems were used most frequently by obstetricians, gynecologists, urogynecologists, colorectal surgeons, proctologists, general surgeons, physiotherapists, theoretical scientists, and gastroenterologists in North America, Europe, and Asia. The most commonly used tool was the Wexner scale, which was used by 49.1 % of the respondents [11].
The translation and validation procedure did not differ greatly from those used in other countries. One of the alterations that we required was the use of an interviewer to fill out forms for the patients. Although the WS was developed to be a self-administered questionnaire, the low sociocultural level of our patients did not allow for self-reporting. The second adaptation was the administration of the retest via telephone, which differs from a face-to-face interview, approximately 15 days after the first visit. Telephone administration of the WS was chosen because it is a reliable and accurate method that can be used to facilitate clinical and epidemiological research by decreasing costs and improving access to participants. This mode of administration helps to overcome some of the limitations associated with written follow-up, including the willingness to return for an interview, the lack of transportation, illness, or embarrassment regarding face-to-face contact with an interviewer [20]. Telephone-administered questionnaires have been used in several different types of health surveys, and many have demonstrated the validity of these methods of data collection within health care [20, 21].
Women with urogynecological problems are likely to have concomitant AI and urinary incontinence [22]. In our study, these conditions occurred in 84.3 % of the patients. Therefore, evaluating women with pelvic floor disorders must include urinary and anal function. However, manometric evaluation of all such patients is not justified and is not always easily accomplished, even when it is required. Symptom scores and other quality of life instruments could be used to screen patients who should proceed with more invasive and expensive testing.
Furthermore, in the study population, only 34 % had already sought treatment for AI, and 28 % reported that a doctor had already spontaneously asked them about symptoms of AI. In population-based surveys, when people with AI are asked whether they have discussed this problem with their healthcare provider, only a third respond that they have done so. This level of response is also found in acute care hospitals, nursing homes, and community settings. A possible reason for the failure to recognize and report AI is the belief of many healthcare providers that AI is a normal part of aging: a UK nursing home survey found that the trained staff cited advanced age as the main cause of incontinence [5]. The WS has the strength of ease in scoring and is widely used because of its simplicity. Thus, it may be a simple but no less effective way of approaching an embarrassing issue.
One limitation of our study was the order of the questionnaire administration methods. Because we did not test whether the order of administration of face-to-face interview/telephone interview affected the results, we cannot recommend different orders before validation. A second limitation is the lack of evidence of sensitivity to change, which should also be the objective of future studies. The last limitation is the fact that 7.2 % of the patients were illiterate; thus, the WS was read to them. We tried to just read and not to interpret the questions for them, but this could be considered a bias in favor of successful results.
In conclusion, the Brazilian Portuguese translated version of the Wexner scale is a reliable, consistent, and valid instrument for assessing symptom severity and the impact on quality of life among women with AI.
References
Haylen BT, de Ridder D, Freeman RM et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29(1):4–20
Andromanakos NP, Filippou DK, Pinis SI, Kostakis AI (2013) Anorectal incontinence: a challenge in diagnostic and therapeutic approach. Eur J Gastroenterol Hepatol 25(11):1247–1256
Bellicini N, Molloy PJ, Caushaj P, Kozlowski P (2008) Fecal incontinence: a review. Dig Dis Sci 53(1):41–46
Nevler A (2014) The epidemiology of anal incontinence and symptom severity scoring. Gastroenterol Rep (Oxf) 2(2):79–84
Norton C, Whitehead WE, Bliss DZ, Harari D, Lang J; Conservative Management of Fecal Incontinence in Adults Committee of the International Consultation on Incontinence (2010) Management of fecal incontinence in adults. Neurourol Urodyn 29(1):199–206
Whitehead WE, Borrud L, Goode PS et al (2009) Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology 137(2):512–517
Melville JL, Fan MY, Newton K, Fenner D (2005) Fecal incontinence in US women: a population-based study. Am J Obstet Gynecol 193(6):2071–2076
Gordon D, Groutz A, Goldman G et al (1999) Anal incontinence: prevalence among female patients attending a urogynecologic clinic. Neurourol Urodyn 18(3):199–204
Cam C, Selcuk S, Asoglu MR et al (2011) Validation of the Wexner scale in women with fecal incontinence in a Turkish population. Int Urogynecol J 22(11):1375–1379
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36(1):77–97
Rusavy Z, Jansova M, Kalis V (2014) Anal incontinence severity assessment tools used worldwide. Int J Gynaecol Obstet 126(2):146–150
Yusuf SA, Jorge JM, Habr-Gama A, Kiss DR, Gama Rodrigues J (2004) Evaluation of quality of life in anal incontinence: validation of the questionnaire FIQL (fecal incontinence quality of life). Arq Gastroenterol 41(3):202–208
Guillemin F, Bombardier C, Beaton D (1993) Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 46(12):1417–1432
Ferraz MB, Oliveira LM, Araujo PM, Atra E, Tugwell P (1990) Crosscultural reliability of the physical ability dimension of the health assessment questionnaire. J Rheumatol 17(6):813–817
Barber MD (2007) Questionnaires for women with pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 18(4):461–465
Patrick DL, Martin ML, Bushnell DM, Marquis P, Andrejasich CM, Buesching DP (1999) Cultural adaptation of a quality-of-life measure for urinary incontinence. Eur Urol 36(5):427–435
Cronbach LJ (1951) Coefficient alpha and the internal structure of tests. Psychometrika 16:297–334
Deyo RA, Diehr P, Patrick DL (1991) Reproducibility and responsiveness of health status measures. Statistics and strategies for evaluation. Control Clin Trials 12 [4 Suppl]:142S–158S
Tamanini JT, Almeida FG, Girotti ME, Riccetto CL, Palma PC, Rios LA (2008) The Portuguese validation of the International Consultation on Incontinence Questionnaire-Vaginal Symptoms (ICIQ-VS) for Brazilian women with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 19(10):1385–1391
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193(1):103–113
Geller EJ, Barbee ER, Wu JM, Loomis MJ, Visco AG (2007) Validation of telephone administration of 2 condition-specific quality-of-life questionnaires. Am J Obstet Gynecol 197(6):632.e1–632.e4
Meschia M, Buonaguidi A, Pifarotti P, Somigliana E, Spennacchio M, Amicarelli F (2002) Prevalence of anal incontinence in women with symptoms of urinary incontinence and genital prolapse. Obstet Gynecol 100(4):719–723
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Funding
Minas Gerais Foundation of Support Research (FAPEMIG).
Rights and permissions
About this article
Cite this article
Fonseca, A.M., Meinberg, M.F., Lucas, D.V. et al. Cultural adaptation and validation of the Wexner scale in patients with anal incontinence in a Brazilian population. Int Urogynecol J 27, 959–963 (2016). https://doi.org/10.1007/s00192-015-2927-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2927-y