Abstract
Introduction and hypothesis
The aim of this observational study was to investigate the influence of body mass index (BMI) smoking and age on the cure rate, rate of complications and patient satisfaction with mid-urethral sling (MUS) procedures.
Methods
Pre-, peri- and postoperative (8 weeks and 1 year) data were retrieved from the Swedish National Register for Gynecological Surgery of MUS procedures (retropubic procedures, n = 4,539; transobturator procedures, n =1,769) performed between January 2006 and December 2011. Multiple logistic regression analyses were performed between the outcome variables and BMI and smoking, presented as adjusted odds ratios (adjOR) with 95 % confidence interval (CI).
Results
Subjective 1-year cure rate was 87.4 % for all MUS procedures (88.3 % with the retropubic technique and 85.2 % with the transobturator technique (p = 0.002). Preoperative daily urinary leakage and urgency were more common with increasing BMI, but surgery reduced symptoms in all BMI groups. Lower cure rate was seen in women with a BMI >30 (0.49; CI 0.33–0.73), in diabetics (0.50; CI 0.35–0.74) and women aged > 80 years (0.18; CI 0.06–0.51). Perioperative complications were more common in the retropubic group (4.7 % vs 2.3 % in the transobturator group, p=0.001) and in women with BMI < 25. Smoking did not influence any of the outcome variables.
Conclusions
The overall 1-year cure rate for MUS procedures was 87 %, but was negatively influenced by BMI >30, diabetes and age > 80 years. Perioperative complications were more common with the retropubic procedure than with the transobturator technique, and in women with a BMI < 25. Smoking did not impact on any of the studied outcome variables.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence (UI) is a common condition in women, often resulting in reduced quality of life as well as being of considerable economic importance for the health service. The reported prevalence of stress urinary incontinence (SUI) in population studies varies between 10 and 39 % [1]. Different treatment modalities for stress urinary incontinence in women have been advocated, including the use of surgical procedures.
Mid-urethral sling (MUS) procedures have since their introduction in the 1990s become the golden standard for treating SUI [2]. They are minimally invasive, associated with a low morbidity and show good results in the long term [3, 4]. Surgery for UI is common worldwide, and many thousands of operations are performed annually. In this respect, it is therefore important to identify factors that may potentially cause an increased risk of complications or an unsuccessful result. Modifiable lifestyle factors such as obesity and smoking are well-documented risk factors for UI [1, 5], but the evidence regarding their influence on the outcome of incontinence surgery is less well defined.
Incontinence surgery may be more difficult in obese patients; however, only 1 of 6 studies in a review from 2008 showed a difference in early postoperative complications in women undergoing a tension-free vaginal tape (TVT) who had a body mass index (BMI) >40 compared with women with a BMI < 30 [6]. Surgery was stated to be a legitimate and safe treatment of SUI in the obese, and additional studies have reported a risk reduction of bladder perforations in overweight and obese patients [7–9].
There is concern regarding the cure rate in MUS and obese women, although most studies [9, 10] have not reported any difference in cure rate the first year following surgery. However, Hellberg et al. demonstrated a decrease in the long-term cure rate with the TVT procedure from 81.2 % in normal-weight women compared with 52.1 % in the obese group [11].
People who smoke have been reported to have a considerably increased risk of intra- and postoperative complications and perioperative smoking cessation has been shown to be effective in reducing complications, mainly based upon studies performed in general and orthopaedic surgery [12]. Data are scarce in relation to the influence of smoking on the outcome of MUS.
The aim of this study was to investigate the influence of obesity, smoking and age on the complication and cure rates, and patient satisfaction in women who had undergone a mid-urethral sling procedure performed in routine clinical practice.
Materials and methods
Information was collected about patients included in the Swedish National Register for Gynecological Surgery (GynOp) who underwent a MUS procedure (either as a retropubic procedure or as a transobturator procedure) between January 2006 and December 2011. Patients with concomitant prolapse surgery, previous incontinence surgery or with missing data on smoking and BMI were excluded. The register was established in 1997 (www.gynop.org); information regarding incontinence operations has been included in the register since 2006 and 70 % of all hospitals in Sweden have provided information on patients undergoing incontinence surgery. In accordance with the regulations for the management of national quality registers, the patient receives written information about the register prior to surgery and has an opportunity to decline participation.
Data were obtained from questionnaires sent to the patients before surgery, 8 weeks and 1 year after surgery. Preoperatively, the patient completed a form including a health declaration and a description of subjective symptoms. The frequency of urinary leakage was assessed by the patient according to the following: no leakage; almost never; 1–3 times/month; 1–3 times/week or daily leakage. An assessment was also performed by the gynaecological surgeon that included a gynaecological examination, micturition lists, cough test, residual urine measurement, and other relevant clinical data. Based on the history provided and this evaluation, the women were classified as having either SUI or mixed UI (MUI) according to the joint IUGA/ ICS definition [13]. In the health declaration, body height and weight were recorded and used for the calculation of BMI.
The surgeon registered data about perioperative findings on an operation form and a discharge form. As a follow-up, a questionnaire, was sent to the patient 8 weeks and 1 year after surgery, which was subsequently evaluated by the surgeon if there had been any complications and whether the complications were mild or severe.
Validated questionnaires regarding the evaluation of UI were used throughout [14, 15]. The patients’ acceptance of the use of questionnaires to collect information regarding gynaecological surgical procedures reported to GynOp has previously been evaluated; the questionnaires were well accepted by the patients and provided complete post-treatment information [16].
Data extracted included age, BMI, smoking, parity, hormonal status, type of incontinence (SUI, MUI), surgical history, co-morbidities such as heart disease, hypertension, diabetes, neurological diseases and respiratory diseases (asthma and chronic obstructive pulmonary disease), type of surgery, duration of surgery, blood loss, any blood transfusion, antibiotic prophylaxis and hospital stay parameters. Previous studies have reported a difference in complications comparing retropubic MUS with transobturator MUS [17, 18]. The surgical procedures in this study were therefore analysed separately and grouped as a retropubic group and a transobturator group.
Complications were classified in order of appearance: perioperative complications (reported at discharge after surgery), early postoperative complications (from the 8-week questionnaire) and late postoperative complications (from the 1-year questionnaire). Complications included organ lesions, anaesthetic-related complications, bleeding, infection, pain, urinary retention, venous thromboembolism (VTE) and reoperation. The intention for analysing late complications was to detect de novo urgency, failure of cure and dissatisfaction with surgery. Patients were interpreted to have de novo urgency if they had preoperatively answered “no”, “almost never” or “1–3 times/month” to the question “do you have urgency problems”, and 1 year after surgery reported frequent urgency problems, i.e. “daily urgency” or “1–3 times/week”. Information on satisfaction with the procedure and cure rate was obtained from the 1-year questionnaire. The answers from the question “Are you satisfied with the result of the surgery?” were dichotomized into satisfied (very satisfied and satisfied) and not satisfied (“neither satisfied nor unsatisfied”, “unsatisfied” and “very unsatisfied”. The cure rate was derived from patient-reported assessment of urinary leakage. Leakage “1–3 times/week” or “daily leakage” was defined as “no cure” and “cure” was defined when the answer was “no urinary leakage”, “almost no leakage” or “1–3 times/month”. Ethical approval was obtained from the Ethics Committee at Sahlgrenska Academy, Gothenburg University (061-13).
Categorical data were analysed using Pearson’s Chi-squared or Fisher’s exact test. Continuous variables were analysed using Student’s t test. A p value < 0.05 was considered to be statistically significant. A logistic regression model was used to assess risk factors for the different outcome variables, while controlling for potential confounding factors. Crude odds ratio (OR) and the 95 % confidence interval (CI) for possible confounders were calculated. Variables presenting an association with the dependent variables (p value <0.05) were included in a multiple logistic regression analysis. The following variables were included in the regression analyses for complications: age, BMI, smoking status, type of surgical procedure, previous prolapse surgery, hysterectomy and comorbidity. The following additional variables were included in the analyses for cure and the evaluation of the patient’s degree of satisfaction with the operation: parity, peri- and postoperative complications, the assessment of urinary leakage, de novo urgency and postoperative daily urgency. A stepwise approach was conducted in order to, one-by-one, exclude the variables demonstrated to be non-significant in the multiple testing. Adjusted odds ratio (adjOR) and the 95 % CI were calculated.
Prior to conducting a logistic regression analysis, some of the independent variables were transformed. Age was encoded into the intervals ≤40, 41–60, 61–80 and >80 and parity into three groups (women with no birth, one birth, or two or more births). 5 BMI subgroups were defined using the WHO definitions [19]: under-weight <18.5; normal 18.5–24; overweight 25–29; obesity I 30–34 and obesity II >35. Based on information about smoking, the participants were classified as either current smokers, former smokers or non-smokers. All statistical analyses were performed using SPSS version 21.
Results
The patients included in this study had undergone an MUS procedure between January 2006 and December 2011. A total of 6,308 women were included in the study for evaluation. Baseline characteristics and perioperative data in the different surgical groups are shown in Table 1. In the transobturator group, the patients were older, had a higher mean BMI, had an increased prevalence of previous hysterectomies, had more frequently undergone general anaesthesia and had a shorter duration of surgery compared with the retropubic group. No difference between groups was seen in mean blood loss or when blood loss >200 ml was analysed.
Perioperative complications were more than twice as common in the retropubic group compared with the transobturator group (4.7 % vs 2.3 % p = 0.001), mainly because of bladder perforations (Table 2). This was confirmed in the multiple regression analysis, which demonstrated that perioperative complications occurred more commonly with the retropubic procedure than with the transobturator technique (adjOR 2.08; CI 1.48–2.94). Perioperative complications were less common in women aged 41–60 than in women ≤ 40 and in women with a BMI ≥25 compared with women with a BMI < 25 (Table 3).
The response rate for the 8-week follow-up questionnaire was 98 % and 81 % after 1 year postoperatively. At 8 weeks the rate of reported postoperative complications was 13 % in the retropubic group and 14.3 % in the transobturator group (p =0.479). The most frequently recorded postoperative complications were pain, urinary tract infections, bladder and urethral lesions and urinary retention. Reoperation before discharge was necessary in 1.5 % after a retropubic procedure and 1.1 % after a transobturator procedure (p = 0.013) and additional reoperations within 8 weeks were 0.6 % in both surgery groups (Table 2). Postoperative complications were more commonly reported in women ≤40 years of age than in women >40 years. BMI, smoking status and type of surgical procedure did not influence the rate of postoperative complications (Table 3). There were no differences in the rate of infections, thrombotic events, sepsis or complications necessitating intensive care between smokers and non-smokers.
Complication rates and outcome 1 year after surgery stratified according to BMI and smoking status are described in Tables 4 and 5. The rate of de novo urgency 1 year after surgery was 9.8 % in the retropubic group and 11.2 % (p = 0.293) for the transobturator group. 2,550 women had no urgency preoperatively, and 259 of these women reported, in the 1-year questionnaire, urgency symptoms 1–3 times/week or daily. De novo urgency was more frequently reported among smokers and in women with increasing BMI (Tables 4, 5); however, in the multiple regression analysis none of the tested variables were statistically significantly associated with de novo urgency.
The overall cure rate after 1 year for all MUS procedures was 87.4 % (88.3 % in the retropubic group and 85.2 % in the transobturator group, p = 0.002). There was no difference in the cure rate in women up to the age of 80 years, but when aged >80 years the cure rate was decreased. There was also a lower cure rate in women with a BMI ≥30 compared with women with a BMI <30 and in diabetic women compared with non-diabetic women (Table 6); none of the other comorbidities influenced the cure rate.
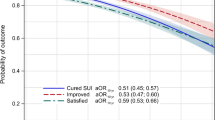
Figure 1 depicts the effect of surgery on urinary leakage and urgency grouped according to BMI. Before surgery, women with a high BMI suffered from more daily urgency symptoms and daily urinary leakage compared with women with a lower BMI. Surgery reduced both symptoms markedly; however, after 1 year there was still a higher remaining rate of daily urgency and daily leakage in women with a higher BMI. The reduction rate for daily UI and daily urgency did not differ between different BMI groups, but since obese women had more frequent symptoms at baseline they had more symptoms after surgery.
In spite of a lower cure rate 1 year after surgery in obese women, there was no significant difference in the level of satisfaction with the results of surgery. Women with postoperative complications (adjOR 0.40; CI 0.31–0.51), daily urinary leakage (adjOR 0.07; CI 0.06–0.09), daily urgency (adjOR 0.20; CI 0.16–0.26) and de novo urgency (adjOR 0.54; CI 0.37–0.79) were more often dissatisfied with the result of the operation 1 year after surgery.
Discussion
As has been reported by other authors [20] the prevalence of daily urinary leakage and daily urgency before surgery in our study was higher with increasing BMI. However, the prevalence of daily urinary leakage and daily urgency before surgery was reduced following surgery in all BMI classes. There was a reduced cure rate in women with a BMI >30 and in diabetic women, although the cure rate was unaffected by other comorbidities such as hypertension, asthma, bronchitis and heart disease. The overall cure rate 1 year after a mid-urethral sling procedure was 87 % and was higher in the retropubic group than in the transobturator group. The cure rate remained unchanged in women up to 80 years of age. Smoking did not influence the outcome of MUS procedures.
There was a lower frequency of perioperative complications, mainly bladder perforations, in women with a higher BMI who underwent a retropubic procedure, which is in agreement with earlier retrospective studies [7–9]. The fatty tissue probably creates a space for the trocar between the retropubic bone and the bladder, thus protecting the bladder. In a slim patient in need of incontinence surgery it may be advisable to choose an transobturator method to avoid bladder perforation; on the other hand, the risk of postoperative hip and thigh pain is reported to be higher with these procedures [21], which was apparent in our study as well (Table 2). There was no association between BMI and postoperative complications. Overall, the rate of complications was low, indicating that MUS procedures are a safe surgical procedure in routine clinical practice, even in obese women. Nor were there any differences in the rate of postoperative complications between surgical groups, even though bladder perforations were more common in the retropubic group. This indicates that there were few long-term effects of this type of complication.
Even if the MUS is safe in obese patients, the outcome is of great importance. Patients with a BMI >30 had lower cure rate 1 year after surgery compared with women of normal weight. However, despite this finding, the women with high BMI still reported that they were satisfied with the results of the surgery (satisfaction with surgery was not affected by a high BMI in the multiple logistic regression). Obesity has previously been reported to be a risk factor for failure and complications after surgery for incontinence and prolapse [22] and the long-term results in obese women have been reported to be continuously worsening. In a study by Hellberg et al., women with BMI >35 had a long-term cure rate of 52.1 % with an average follow-up time of 5.7 years [11]. Consequently, it is wise to encourage the patient to reduce weight before and after surgery. It has been reported that a moderate reduction in weight of 5 % improves urinary incontinence severity and its effects on quality of life [5, 23].
The frequency of de novo urgency (dU) in our study is consistent with that of previous studies [24] and we also found dU to be a risk factor for dissatisfaction with surgery. BMI and smoking were not associated with dU. In this respect it should be noted that smokers and patients with BMI > 30 had a higher degree of urgency preoperatively, which influenced the inclusion of patients in this specific analysis.
Smoking was not found to be a risk factor for complications with this type of surgery. It should be noted that the prevalence of smoking for women in Sweden is below 15 % [25] and in the current study it was 13 %. In the literature the most commonly reported complications among smokers in connection with surgical procedures are related to wound and respiratory complications, to the anaesthesia or to thromboembolic events [26]. The MUS procedure is a minimally invasive type of surgery, the wound is small and there is a short duration of surgery and anaesthesia. In addition, most surgery is performed under local anaesthesia and immobilisation postoperatively is almost non-existent.
Nevertheless, it has been shown that surgery is a golden opportunity to motivate the patient to lifestyle changes such as smoking cessation [27]. Probably, the stress of being exposed to surgery alerts the patient to reconsider her general health status, thus enhancing the likelihood of successful smoking cessation. Although our study showed that a high BMI and smoking had no effects on the rate of complications or satisfaction in minimally invasive incontinence surgery, the importance of discussing lifestyle factors pre-and postoperatively remains. A weight reduction may potentially improve the cure rate in obese patients in this type of surgery.
The strengths of this study were the large unselected patient population and the high response rate achieved with the questionnaires, which adds validity to the results. There are several difficulties regarding the reliability of register data; the forms are evaluated by different surgeons and factors such as complications may be judged heterogeneously. In GynOp there is a ”complication guide” to facilitate the evaluation of complications, which may minimise this bias. We chose to include different types of MUS in this study, in order to be able to evaluate the routine clinical situation. According to the annual reports from GynOp most clinics use only one MUS method, and only in exceptional cases is another method selected. However, in this study there were some indications that the transobturator method was used for older women and women with a higher BMI. A statistically significant difference in subjective cure rate between the surgical groups could be seen, but when adjusting for confounding factors surgical group was not an independent risk factor in the multiple regression analysis. In summary, we found no difference in outcomes between the procedures, apart from perioperative complications.
Conclusions
The overall 1-year cure rate for MUS procedures was 87 %, but this was negatively influenced by BMI >30, diabetes and age >80 years. Patients with a BMI >30 had a lower cure rate and a poorer subjective outcome after incontinence surgery, such as persistent daily urinary leakage and urgency symptoms, but the rate of satisfaction with surgery was not affected by BMI. There was no correlation between BMI and postoperative complications. Patients with a BMI <25 were shown to be at risk of bladder perforation in the retropubic MUS group. Smoking did not influence the outcome of MUS procedures.
References
Milsom I, Altman D, Cartwright R, Lapitan MC, Nelson R, Sillén U, Tikkanen K (2013) Epidemiology of urinary incontinence (UI) and other lower urinary tract symptoms (LUTS), pelvic organ prolapse (POP) and anal incontinence (AI). In: Abrams P, Cardozo L, Khoury S, Wein A (eds) Incontinence. Health Publications, Paris
Morley R, Nethercliffe J (2005) Minimally invasive surgical techniques for stress incontinence surgery. Best Pract Res Clinic Obstet Gynaecol 19(6):925–940. doi:10.1016/j.bpobgyn.2005.08.014
Kuuva N, Nilsson CG (2002) A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand 81(1):72–77
Nilsson CG, Palva K, Aarnio R, Morcos E, Falconer C (2013) Seventeen years’ follow-up of the tension-free vaginal tape procedure for female stress urinary incontinence. Int Urogynecol J 24(8):1265–1269. doi:10.1007/s00192-013-2090-2
Hunskaar S (2008) A systematic review of overweight and obesity as risk factors and targets for clinical intervention for urinary incontinence in women. Neurourol Urodyn 27(8):749–757
Greer WJ, Richter HE, Bartolucci AA, Burgio KL (2008) Obesity and pelvic floor disorders: a systematic review. Obstet Gynecol 112(2 Pt 1):341–349
Stav K, Dwyer PL, Rosamilia A, Schierlitz L, Lim YN, Lee J (2009) Risk factors for trocar injury to the bladder during mid urethral sling procedures. J Urol 182(1):174–179. doi:10.1016/j.juro.2009.02.140
Dunivan GC, Connolly A, Jannelli ML, Wells EC, Geller EJ (2009) Body mass index as a risk factor for cystotomy during suprapubic placement of mid-urethral slings. Int Urogynecol J Pelvic Floor Dysfunct 20(9):1127–1131. doi:10.1007/s00192-009-0915-9
Lovatsis D, Gupta C, Dean E, Lee F (2003) Tension-free vaginal tape procedure is an ideal treatment for obese patients. Am J Obstet Gynecol 189(6):1601–1604, discussion 1604-1605
Killingsworth LB, Wheeler TL 2nd, Burgio KL, Martirosian TE, Redden DT, Richter HE (2009) One-year outcomes of tension-free vaginal tape (TVT) mid-urethral slings in overweight and obese women. Int Urogynecol J Pelvic Floor Dysfunct 20(9):1103–1108
Hellberg D, Holmgren C, Lanner L, Nilsson S (2007) The very obese woman and the very old woman: tension-free vaginal tape for the treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18(4):423–429
Thomsen T, Villebro N, Moller AM (2010) Interventions for preoperative smoking cessation. Cochrane Database Syst Rev (7):CD002294. doi:10.1002/14651858.CD002294.pub3
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Urogynecol J 21:25–26. doi:10.1007/s00192-00009-00976-00199
Kulseng-Hanssen S (2003) The development of a national database of the results of surgery for urinary incontinence in women. BJOG 110(11):975–982
Kulseng-Hanssen S, Borstad E (2003) The development of a questionnaire to measure the severity of symptoms and the quality of life before and after surgery for stress incontinence. BJOG 110(11):983–988
Ladfors MB, Lofgren ME, Gabriel B, Olsson JH (2002) Patient accept questionnaires integrated in clinical routine: a study by the Swedish National Register for Gynecological Surgery. Acta Obstet Gynecol Scand 81(5):437–442
Latthe PM, Singh P, Foon R, Toozs-Hobson P (2010) Two routes of transobturator tape procedures in stress urinary incontinence: a meta-analysis with direct and indirect comparison of randomized trials. BJU Int 106(1):68–76. doi:10.1111/j.1464-410X.2009.09051.x
Richter HE, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT, Kraus SR, Chai TC, Lemack GE, Dandreo KJ, Varner RE, Menefee S, Ghetti C, Brubaker L, Nygaard I, Khandwala S, Rozanski TA, Johnson H, Schaffer J, Stoddard AM, Holley RL, Nager CW, Moalli P, Mueller E, Arisco AM, Corton M, Tennstedt S, Chang TD, Gormley EA, Litman HJ (2010) Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med 362(22):2066–2076. doi:10.1056/NEJMoa0912658
World Health Organization. BMI classification. 2006 (updated 02/02/2011). Available from: apps.who.int/bmi/index.jsp?introPage=intro_3.html
Dwyer PL, Lee ET, Hay DM (1988) Obesity and urinary incontinence in women. BJOG 95(1):91–96
Cadish LA, Hacker MR, Dodge LE, Dramitinos P, Hota LS, Elkadry EA (2010) Association of body mass index with hip and thigh pain following transobturator midurethral sling placement. Am J Obstet Gynecol 203(5):508. doi:10.1016/j.ajog.2010.07.023, e501-505
Haverkorn RM, Williams BJ, Kubricht WS 3rd, Gomelsky A (2011) Is obesity a risk factor for failure and complications after surgery for incontinence and prolapse in women? J Urol 185(3):987–992
Subak LL, Whitcomb E, Shen H, Saxton J, Vittinghoff E, Brown JS (2005) Weight loss: a novel and effective treatment for urinary incontinence. J Urol 174(1):190–195. doi:10.1097/01.ju.0000162056.30326.83
Lee JK, Dwyer PL, Rosamilia A, Lim YN, Polyakov A, Stav K (2013) Which women develop urgency or urgency urinary incontinence following midurethral slings? Int Urogynecol J 24(1):47–54. doi:10.1007/s00192-012-1844-6
Ng M, Freeman MK, Fleming TD, Robinson M, Dwyer-Lindgren L, Thomson B, Wollum A, Sanman E, Wulf S, Lopez AD, Murray CJ, Gakidou E (2014) Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. JAMA 311(2):183–192. doi:10.1001/jama.2013.284692
Sadr Azodi O, Lindstrom D, Adami J, Bellocco R, Linder S, Wladis A (2008) Impact of body mass index and tobacco smoking on outcome after open appendicectomy. Br J Surg 95(6):751–757. doi:10.1002/bjs.6079
Lindstrom D, Sundberg-Petersson I, Adami J, Tonnesen H (2010) Disappointment and drop-out rate after being allocated to control group in a smoking cessation trial. Contemp Clin Trials 31(1):22–26. doi:10.1016/j.cct.2009.09.003
Details of ethics approval
Ethics approval was obtained from the Regional and the National Ethic Review Boards (the Ethics Committee at Sahlgrenska Academy, Gothenburg University, ref no.061-13, 5 June 2013.
Funding
The study was supported by a National LUA/ALF grant no. 11315 and Hjalmar Svenssson’s Research Foundation.
Financial disclaimer/conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bohlin, K.S., Ankardal, M., Pedroletti, C. et al. The influence of the modifiable life-style factors body mass index and smoking on the outcome of mid-urethral sling procedures for female urinary incontinence. Int Urogynecol J 26, 343–351 (2015). https://doi.org/10.1007/s00192-014-2508-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2508-5