Abstract
Purpose
To evaluate the surgical outcomes of arthroscopic removal of intraosseous deposits in patients with intraosseous calcific tendinitis of the rotator cuff.
Methods
This study involved a retrospective review of 96 patients operated on from 2004 to 2019. Patients were divided into two groups according to the location of calcific deposits. Group I had pure tendinous involvement (n = 71), and Group II had tendinous and intraosseous involvement (n = 25). The mean follow-up time was 6.4 ± 3.9 years. There were 71 patients (46 women, 25 men) in Group I, and the mean age was 49.3 ± 8.2 years (range 30–65 years). In group II, there were 25 patients (18 women, 7 men); the mean age was 47.3 ± 11.2 years (range 28–70 years).
Results
The mean preoperative VAS pain score was 8.8 ± 1.4 in Group I compared to 9.5 ± 0.5 in group II (p = 0.017). The median preoperative Constant and Oxford scores were 42 (20–65) and 22 (8–34) in Group I and 25.5 (22–46) and 10 (8–16) in group II, respectively (p < 0.001). There was no difference in postoperative pain scores (Group I: 0.7 ± 1.6 and group II: 0.5 ± 0.6, p = 0.926), Constant scores [Group I: 100 (80–100) and group II: 100 (90–100), (n.s).] and Oxford scores [Group I: 48 (28–48) and group II: 46.5 (4–48), (n.s.)] between the two groups. The number of preoperative injections was higher in Group II (p = 0.05). There was no correlation between the size of the soft tissue calcific deposit and the preoperative pain, Constant, and Oxford scores (n.s.).
Conclusion
Arthroscopic debridement of calcific tendinitis with intraosseous involvement is a safe and effective treatment method similar to that of pure tendinous involvement.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rotator cuff calcific tendinitis is an inflammatory process associated with severe pain and disability of the shoulder. While inflammation is generally limited to the tendon, it may seldom extend to the adjacent bone, further complicating the problem. This osseous involvement may manifest itself as intraosseous calcific deposits, cortical destruction, bone marrow edema, or osteolytic lesions in the humeral head at the insertion site of the affected tendon [29]. Clinical detection of osseous involvement is crucial not only to plan treatment but also to prevent overtreatment due to misdiagnoses such as possible bone tumors and infection [18, 21, 30].
It has been 10 years since the first series on arthroscopic treatment of calcifying tendinitis of the rotator cuff with osseous involvement was reported [30]. Although series on tendinous calcific tendinitis have been published after this study, the majority of papers demonstrating osseous extension are case reports. [4, 17, 25, 26, 31]. Thereafter, no new series has been published on this rare entity to the best of our knowledge. Additionally, there is a knowledge gap regarding the clinical importance of intraosseous involvement. It is not clear whether these two pathologies differ clinically and require different treatments or surgical indications.
In the current study, it was aimed to evaluate the surgical outcome of the arthroscopic removal of intraosseous deposits from individuals with intraosseous calcific tendinitis with a greater number of patients and a longer mean follow-up time. We hypothesized that patients with osseous involvement would have higher preoperative pain, lower preoperative functional scores, would present with more extensive tendon defects after debridement, would require more complex repair than patients with pure tendinous involvement and would benefit from arthroscopic debridement as much as patients with pure tendinous involvement in the postoperative long-term follow-up.
Materials and methods
The study protocol was approved by the Institutional Review Board of Koc University, Istanbul, Turkey (ID number 2019.208.IRB1.031).
A chart review of patients who underwent surgery due to calcific tendinitis of the rotator cuff between March 2004 and May 2019 was performed. One hundred eighteen shoulders of 116 patients were identified for further analyses.
Inclusion and exclusion criteria are given in Fig. 1. After excluding 1 deceased patient, 3 patients who did not want to participate in the study, 8 patients who were lost to follow-up, and 8 patients with a short follow-up, 98 shoulders of 96 patients were available for an evaluation. Of these 96 patients, 64 (66.6%) were women and 32 (33.4%) were men, with a median age of 48 years (range 28–70 years). The right shoulder was affected in 63 patients; the left shoulder, in 33 patients; and both shoulders, in 2 patients.
Patients were divided into two groups according to the location of calcific deposits. There were 72 shoulders of 71 patients (46 women, 25 men) in Group I, with pure tendinous involvement; the mean age was 49.3 ± 8.2 years (range 30–65 years). Calcifications were localized at the supraspinatus in 34 shoulders of 33 patients, the infraspinatus in 22 patients, the subscapularis in 12 patients, and the teres minor in 4 patients. The mean time between the onset of symptoms and surgery was 9.7 ± 10.4 months (range 3–72 months). In Group II, with tendinous and osseous involvement, there were 26 shoulders of 25 patients (18 women, 7 men); the mean age was 47.3 ± 11.2 years (range 28–70 years). The mean time between the onset of symptoms and surgery was 7.2 ± 4.5 months (range 3–18 months) (Fig. 2).
Surgery was indicated in patients with refractory persistent pain despite 3 months of conservative treatment. In the preoperative physical examination and radiological evaluations, none of the patients had a loss of range of motion and concomitant full-thickness rotator cuff tears or symptomatic acromioclavicular or glenohumeral osteoarthritis. The median preoperative symptomatic duration was 9 months (range 3–72 months). The patients received different nonoperative treatments, including nonsteroidal anti-inflammatory drugs, at least one subacromial injection, and physical therapy exercises during the preoperative symptomatic period. The outcome scores were also compared according to the type of repair of the tendinous defect after removing the deposit, namely, the side-to-side suture or single/double-row repair technique.
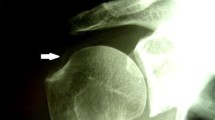
Radiographic evaluation
Preoperative radiographs and magnetic resonance imaging (MRI) results were assessed. In the preoperative evaluation process, the size of calcific deposits was measured using the longest axis on radiographs. The size of the intraosseous lesion was not measured. Radiographs were also taken on the first postoperative day to ensure that no remnants were left and at the last follow-up to rule out recurrence. Intraosseous calcification was defined with MRI as bone edema or cortical erosion adjacent to a soft tissue deposit or in the humeral head [1, 6, 9, 14].
Surgical technique
All patients were operated on arthroscopically by the same surgeon in a beach-chair position under general anesthesia and interscalene block. After intraarticular examination, the interval (biceps tendon) was marked using a No: 0 polydioxanone suture (PDS) before scoping the subacromial area. The deposit was localized with a 20-gauge spinal needle percutaneously under arthroscopic visualization. Excision was completed with a shaver, curette, and synovial resector. Fluoroscopy was used to verify complete removal. The rotator cuff defect was repaired with side-to-side suturing when there was no footprint involvement (n = 37), with the single-row technique when the defect was located at the footprint and was below 2 cm (n = 23), or with a double-row transosseous equivalent technique when the defect was located at the footprint and was larger than 2 cm (n = 38) [8]. Acromioplasty was performed in patients with single- or double-row rotator cuff repair (n = 61), and coracoacromial ligament release without acromioplasty was performed in patients with side-to-side repairs (n = 37). In four patients in Group II, with a mean defect size of 13.8 ± 8.2 mm, additional interventions were required to manage the defect. An oversized metallic anchor (Arthrex Co., Ltd., Naples, Florida, USA) was used in two patients, and a cancellous allograft (10 cm3 and 30 cm3) was required in two patients to fill the gap. All shoulders were placed in an arm sling with an abduction pillow after surgery. All patients were included in a standardized hospital or home-based rehabilitation program after surgery. The rehabilitation regimen consisted of a protection phase with an arm sling allowing tabletop activities in the first 4 weeks. Range of motion exercises started at 4–6 weeks, and advanced strengthening exercises started after 8–10 weeks. For at least 6 months after surgery, full return to sports and strenuous labor was restricted [7].
Follow-up evaluation
The overall mean follow-up time was 6.8 ± 3.7 years; the mean follow-up times for Group I and Group II were 6.9 ± 3.7 years and 6.7 ± 3.7 years, respectively. Clinical and radiographic follow-up was performed. Preoperative and postoperative clinical functional scores were determined with Constant and Oxford shoulder scoring [10, 11]. A ten-point visual analog scale (VAS) was used to assess pain. Functional clinical scoring was performed before and after the operation. Follow-up was performed blindly without knowing whether intraosseous involvement was present.
Statistical analysis
Statistical analysis was performed using SPSS 21.0 (IBM Corp., Armonk, NY, USA). The variables were investigated using visual and analytical methods to determine whether they were normally distributed. Demographic data and patient characteristics were reported using descriptive statistics (mean and standard deviation or median and interquartile range or percentages). The Mann–Whitney U test was used to compare differences between nonnormally distributed variables. While investigating the associations between nonnormally distributed and/or ordinal variables, the correlation coefficients and their significance were calculated using the Spearman test. The chi-square test was used to compare the proportions in different treatment groups. Post hoc power analysis was calculated where a sample size of 96 patients would provide 94.8% power with a 5% significance level on any differences between the study groups. A 5% type-I error level was used to infer statistical significance.
Results
The demographic data of the patients are summarized in Table 1.
The two groups were homogeneously distributed in terms of age, sex, and follow-up time (n.s.). Preoperative pain scores were higher in Group II (p = 0.017). Preoperative Constant (p < 0.001) and Oxford scores (p < 0.001) were higher in Group I. There was no difference in postoperative pain scores (n.s.) or Constant (n.s.) and Oxford (n.s.) scores between the two groups. There was no difference between the two groups in terms of the time between the onset of symptoms and the time of surgery (n.s.). The number of preoperative injections was higher in Group II (p = 0.05).
The mean size of soft tissue calcification was similar between the groups (n.s.). There was no correlation between the size of the soft tissue calcific deposit and preoperative pain scores, Constant scores, or Oxford scores of the patients (n.s.) (Table 2).
While 23 of the shoulders in Group II had tendinous calcification and multiple lobules, the remaining 3 were radiolucent and heterogeneous. On preoperative MRI, there was intraosseous calcification in the greater tuberosity with adjacent bone edema in 21 (80.7%) shoulders, cortical bone erosion in 24 (92.3%) shoulders, and diffuse bone edema in the humeral head in 10 (38.4%) shoulders of Group II patients.
Calcific deposits were completely cleared in all but four patients. These four patients were in the pure tendinous involvement group, and one required side-to-side repair. The postoperative pain, constant and Oxford scores of these four patients were 0 (0–1), 100 (90–100), 46, and 5 (28–48), respectively. In shoulders with multitendon involvement, repairs requiring an anchor (single- or double-row) were more frequent than those in shoulders with single tendon involvement (p = 0.044). The preoperative number of injections (p = 0.022) was lower and preoperative Constant scores (p = 0.019) were higher in the side-to-side repair group than in the group receiving single- or double-row repair with the anchor (Fig. 3).
Discussion
The most important finding of this study is that the preoperative pain and functional scores of patients exhibiting rotator cuff calcific tendinitis with intraosseous involvement were worse than those of the pure tendinous involvement group, but after arthroscopic debridement and repair, clinical outcomes were similar in both groups. To our knowledge, this is the largest cohort analyzing the clinical and radiological results of arthroscopic treatment of rotator cuff calcific tendinitis with intraosseous involvement.
Since the primary diagnosis of all patients was calcific tendinitis, the differential diagnosis of those with osseous involvement was also facilitated. Tendinous calcific tendinitis of the rotator cuff was first reported by Hayes et al. [16], and osseous involvement was reported as a case report [14, 20, 30]. Apart from the series that we previously published in 2009 with five patients, Klontsaz et al. reported a series of ten patients with intraosseous extension. They reported results of ultrasound-guided percutaneous irrigation [20]. To our knowledge, patient series with osseous involvement are very limited in the literature. This is the largest patient cohort reporting results of intraosseous involvement compared with intratendinous involvement.
In the previous study, there was no difference between the two groups in terms of preoperative pain and functional (Constant) scores or the number of preoperative injections (n.s). The mean size of soft tissue calcification was larger in the intraosseous involvement group. There was no correlation between the size of the calcific deposit and the preoperative pain and Constant scores of the patients [30]. In the current study, preoperative pain (p = 0.017) was higher, Constant scores (p < 0.001) were lower, and preoperative injection numbers (p = 0.05) were higher in the intraosseous involvement group. The mean size of soft tissue calcification was similar between the groups (n.s.). The main reasons for this difference may be associated with the higher number of patients and longer follow-up. While the previous series comprised 5 patients of intraosseous involvement among 30 patients with a mean 38-month follow-up, in the current study, the mean follow-up time was doubled, and the cohort included 25 patients of intraosseous involvement among 96 patients (98 shoulders).
There is no consensus in the literature on the standard approach to be used in the surgical treatment of calcific tendinitis. There is no consensus on whether all deposits should be removed, whether the tendon defects should be repaired, how those tendon defects should be repaired (side-to-side sutures, single row or double row), and what would be the method or the approach to intraosseous involvement [5]. Ark et al., in their study of 23 patients, detected residual calcific deposits radiographically in 12 patients; however, pain relief was achieved in all of them, and the authors reported that repair of the defects was not necessary [2]. On the other hand, Jerosch et al. argued that the deposits should be completely removed, while defects occurring after removal did not necessarily need to be repaired [19]. Porcellini et al., however, in their study with 63 patients with rotator cuff calcific tendinitis treated with arthroscopy, recommended that the calcific deposits be completely removed and the defect be repaired, and they believed that the dimensions of the residual calcifications and Constant scores were inversely related [28]. In the current series, in 94 of 98 (95.9%) shoulders, complete removal of the calcific deposits was achieved, and a significant change in postoperative pain and functional scores was detected. We recommend the complete removal of bursal side deposits and the repair of tendon defects with appropriate methods.
Klontzas et al. investigated the functional scores of rotator cuff calcific tendinitis with osseous involvement treated with USG-guided percutaneous irrigation, and they suggested that intraosseous involvement should be handled as a distinctive form of the disease in contrast to pure tendinous involvement [20]. In addition, Maier et al. reported that the differences in the intra- and interobserver reliabilities of the different classification systems using radiographs and CT scans were statistically insignificant [24]. Intraosseous involvement should be classified as a separate pattern. New classification systems can be developed with a full understanding of the mechanism of calcific tendinitis pathogenesis with various molecular and gene mRNA sequencing analysis studies. Moreover, the new classification system can also be developed by considering the scapular and acromial morphology, which can also play a role in the pathogenesis of rotator cuff calcific tendinitis [3].
The necessity of removing the intraosseous deposit in the surgical treatment of calcific tendinitis is still under debate [12, 13, 22, 23, 27]. Although the results in the previous series were generally successful, they show a range of satisfaction rates. Porcellini et al. established a strong correlation and recommended the entire removal of residual calcium deposits causing persistent pain. They found that arthroscopic removal of deposits and debridement of the residual lesion improved Constant scores in calcific tendinitis patients with and without osseous extension [28]. However, Klontzas et al. found that the outcomes were significantly less favorable in the intraosseous extension group. Klontzas observed no changes for the intraosseous group in terms of mean improvement scores after ultrasound-guided percutaneous irrigation treatment during a 1-year follow-up [20]. In contrast, a significant improvement in outcomes after surgical debridement was determined. These differences may occur due to the treatment method selected. Arthroscopic removal of intraosseous and intratendinous deposits in patients with intraosseous involvement appears to be as safe and effective as arthroscopic removal of intratendinous deposits in patients of only tendinous involvement.
Certain measures have been taken to interpret the data accurately and avoid the ceiling effect. This was done by choosing the Constant score, a validated scoring system that has often been used in similar studies. The Constant score was also preferred as the evaluation method that was used in the previous published series to determine the functional score. The postoperative median Constant score was 100, similar to the current study. In addition, Oxford scoring, which is a widely preferred and validated scale among shoulder scoring systems, was also used to determine functional results. Oxford scores also show that postoperative functional scores are at the upper limit. Similar results of postoperative pain scoring were also obtained. We, therefore, believe that we successfully used the combination of previously validated and supported surveys to prevent ceiling effects.
This study should be evaluated considering its limitations. It was not possible to record the size of the intraosseous deposit or the bone defect after debridement. Larger involvement may be associated with worse clinical outcomes, whereas smaller affected areas may be similar to those with tendinous involvement. A reliable method is required to measure preoperative intraosseous involvement. Another limitation is the use of subjective scores in evaluating functional results. For the functional assessment of functional results, the Constant score was used most often for the monitoring of shoulder patients, and the VAS employed for pain assessment. In addition to the Constant score, the Oxford shoulder score was also used in the functional evaluation, unlike the previous study [30], and results similar to the Constant score results were obtained with the Oxford score.
More work is required to understand the differences in intraosseous and intratendinous involvement regarding the underlying pathophysiology and clinical outcomes. We believe that this study will contribute to the current knowledge regarding these pathologies and possible outcomes, particularly intraosseous calcific tendinitis. Our results support the surgical treatment of calcific deposits recalcitrant to conservative methods, regardless of the involvement pattern.
Conclusions
Arthroscopic debridement of calcific tendinitis with intraosseous involvement is a safe and effective treatment method similar to that of pure tendinous involvement.
References
Albano D, Coppola A, Gitto S, Rapisarda S, Messina C, Sconfienza LM (2021) Imaging of calcific tendinopathy around the shoulder: usual and unusual presentations and common pitfalls. Radiol Med 126(4):608–619
Ark JW, Flock TJ, Flatow EL, Bigliani LU (1992) Arthroscopic treatment of calcific tendinitis in the shoulder. Arthroscopy 8:183–188
Balke M, Banerjee M, Vogler T, Akoto R, Bouillon B, Liem D (2014) Acromial morphology in patients with calcific tendinitis of the shoulder. Knee Surg Sports Traumatol Arthrosc 22(2):415–421
Balke M, Bielefeld R, Schmidt C, Dedy N, Liem D (2012) Calcifying tendinitis of the shoulder: midterm results after arthroscopic treatment. Am J Sports Med 40(3):657–661
Beckmann NM, Tran MQ, Cai C (2019) Incidence of rotator cuff tears in the setting of calcific tendinopathy on MRI: a case controlled comparison. Skeletal Radiol 48:245–250
Brinkman JC, Zaw TM, Fox MG, Wilcox JG, Hattrup SJ, Chhabra A, Neville MR, Hartigan DE (2020) Calcific tendonitis of the shoulder: protector or predictor of cuff pathology? A magnetic resonance imaging-based study. Arthroscopy 36(4):983–990
Buyukdogan K, Aslan L, Koyuncu Ö, Eren İ, Birsel O, Fox MA et al (2021) Long term outcomes after arthroscopic transosseous equivalent repair: clinical and MRI results of rotator cuff tears at a minimum follow-up of 10 years. J Shoulder Elb Surg. https://doi.org/10.1016/j.jse.2021.04.034
Buyukdogan K, Koyuncu O, Eren I, Birsel O, Fox MA, Demirhan M (2019) Arthroscopic knotless separate layer transosseous equivalent repair of delaminated rotator cuff tears. Arthrosc Tech 8:1193–1200
Chianca V, Albano D, Messina C, Midiri F, Mauri G, Aliprandi A et al (2018) Rotator cuff calcific tendinopathy: from diagnosis to treatment. Acta Biomed 89:186–196
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Dawson J, Rogers K, Fitzpatrick R, Carr A (2009) The Oxford shoulder score revisited. Arch Orthop Trauma Surg 129:119–123
Drummond Junior M, Ayinon C, Rodosky M, Vyas D, Lesniak B, Lin A (2021) Predictive factors for failure of conservative management in the treatment of calcific tendinitis of the shoulder. JSES Int 5(3):469–473
Dumoulin N, Cormier G, Varin S, Coiffier G, Albert JD, Le Goff B et al (2021) Factors associated with clinical improvement and the disappearance of calcifications after ultrasound-guided percutaneous lavage of rotator cuff calcific tendinopathy: a post hoc analysis of a randomized controlled trial. Am J Sports Med 49(4):883–891
Flemming DJ, Murphey MD, Shekitka KM, Temple HT, Jelinek JJ, Kransdorf MJ (2003) Osseous involvement in calcific tendinitis: a retrospective review of 50 cases. Am J Roentgenol 181:965–972
Gwalani R, Thombare P, Verma M, Ahuja G, Patkar D (2020) MRI findings in intraosseous extension of calcific supraspinatus tendonitis. Radiol Case Rep 15(7):975–977
Hayes CW, Rosenthal DI, PlataMJ HTM (1987) Calcific tendinitis in unusual sites associated with cortical bone erosion. Am J Roentgenol 149:967–970
Hutchinson JL, Gusberti D, Saab G (2019) Changing appearance of intraosseous calcific tendinitis in the shoulder with time: a case report. Radiol Case Rep 14(10):1267–1271
Jain TP, Damiani M (2020) Calcific tendinosis of rotator cuff with intraosseous extension. J Med Imaging Radiat Oncol 64(2):250–251
Jerosch J, Strauss JM, Schmiel S (1998) Arthroscopic treatment of calcific tendonitis of the shoulder. J Shoulder Elb Surg 7:30–37
Klontzas ME, Vassalou EE, Karantanas AH (2017) Calcific tendinopathy of the shoulder with intraosseous extension: outcomes of ultrasound-guided percutaneous irrigation. Skelet Radiol 46:201–208
Lanza E, Banfi G, Serafini G, Lacelli F, Orlandi D, Bandirali M et al (2015) Ultrasound-guided percutaneous irrigation in rotator cuff calcific tendinopathy: what is the evidence? A systematic review with proposals for future reporting. Eur Radiol 25:2176–2183
Louwerens JKG, Sierevelt IN, Kramer ET, Boonstra R, van den Bekerom MPJ, van Royen BJ et al (2020) Comparing ultrasound-guided needling combined with a subacromial corticosteroid injection versus high-energy extracorporeal shockwave therapy for calcific tendinitis of the rotator cuff: a randomized controlled trial. Arthroscopy 36(7):1823–1833
Louwerens JK, Veltman ES, van Noort A, van den Bekerom MP (2016) The effectiveness of high-energy extracorporeal shockwave therapy versus ultrasound-guided needling versus arthroscopic surgery in the management of chronic calcific rotator cuff tendinopathy: a systematic review. Arthroscopy 32(1):165–175
Maier M, Schmidt-Ramsin J, Glaser C, Kunz A, Kuchenhoff H, Tischer T (2008) Intra- and interobserver reliability of classification scores in calcific tendinitis using plain radiographs and CT scans. Acta Orthop Belg 74:590–595
Marinetti A, Sessa M, Falzone A, Della Sala SW (2018) Intraosseous migration of tendinous calcifications: two case reports. Skelet Radiol 47(1):131–136
Miranda I, Sánchez-Alepuz E, Díaz-Martínez JV, Collado-Sánchez A, Peregrín-Nevado I (2020) Calcific tendinopathy of the shoulder with intraosseous extension: experience with arthroscopic treatment and review of the literature. Rev Esp Cir Ortop Traumatol (Engl Ed) 64(1):13–21
Oudelaar BW, Huis In’t Veld R, Schepers-Bok R, Ooms EM, Nelissen RGHH, Vochteloo AJH (2020) Prognostic factors for the outcome of needle aspiration of calcific deposits for rotator cuff calcific tendinitis. Eur Radiol 30(7):4082–4090
Porcellini G, Paladini P, Campi F, Paganelli B (2004) Arthroscopic treatment of calcifying tendinitis of the shoulder: clinical and ultrasonographic follow-up findings at two to five years. J Shoulder Elb Surg 13:503–508
Sansone V, Maiorano E, Galluzzo A, Pascale V (2018) Calcific tendinopathy of the shoulder: clinical perspectives into the mechanisms, pathogenesis, and treatment. Orthop Res Rev 10:63–72
Seyahi A, Demirhan M (2009) Arthroscopic removal of intraosseous and intratendinous deposits in calcifying tendinitis of the rotator cuff. Arthroscopy 25:590–596
Zampa V, Aringhieri G, Rossi P, Capanna R, Caramella D (2021) Humeral greater tuberosity osteolysis as a complication of intraosseous calcification migration: natural history depicted by imaging. Acta Biomed. https://doi.org/10.23750/abm.v92iS1.8370
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Ethical approval was obtained from the institutional review board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Caliskan, E., Eren, I., Aslan, L. et al. Intraosseous calcific tendinitis of the rotator cuff yields similar outcomes to those of intratendinous lesions despite worse preoperative scores. Knee Surg Sports Traumatol Arthrosc 30, 2485–2491 (2022). https://doi.org/10.1007/s00167-022-06870-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06870-2