Abstract
Purpose
To determine the differences in anatomic parameters between ipsilateral dislocated knees and contralateral non-dislocated knees in patients with unilateral patellar dislocation and to identify any variations in ipsilateral knees contributing to contralateral anatomic abnormalities.
Methods
A total of 82 patients with unilateral patellar dislocation from 2016 to 2019 were retrospectively evaluated. Bilateral anatomic factors, including the tibial tubercle to trochlear groove (TT-TG) distance, lower limb rotational deformities, trochlear dysplasia, patella tilt, and patellar height, were assessed by CT.
Results
The study included 46 patients (32 females and 14 males, mean age ± SD 20.5 ± 6.8). The interobserver reliability of each parameter showed excellent agreement. The ipsilateral TT-TG distance (P = 0.004), patella tilt (P = 0.001), and patellar height (P = 0.01) were greater in the ipsilateral knees than in the contralateral knees. The lateral trochlea inclination (LTI) in the contralateral knees was larger than that in the ipsilateral knees (P = 0.022). There was a significant difference in the distribution of trochlear dysplasia of Dejour between the ipsilateral knees (dislocated side) and the contralateral knees (P = 0.036). However, bilateral femoral and/or tibial torsion, and bilateral knee joint rotation did not differ significantly. Binary logistic regression showed that only ipsilateral LTI revealed significant ORs of 8.83 (P = 0.016) and 7.64 (P = 0.018) with regard to contralateral abnormal tibial torsion and LTI, respectively.
Conclusion
In patients with unilateral patellar dislocation, the ipsilateral TT-TG distance, patella tilt, and patellar height values were larger in the ipsilateral knees than in the contralateral knees, and trochlear dysplasia was more severe in the ipsilateral joints. The risks of contralateral pathological tibial torsion and LTI were 8.8- and 7.6-fold higher, respectively, in patients with abnormal ipsilateral LTI.
Level of evidence
Level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Unilateral and bilateral patellar dislocation (PD) can occur, with unilateral patellar dislocation (UPD) accounting for a large proportion of dislocations [10]. Several factors contributing to patellar instability have been identified, including demographic and anatomic factors. Patellofemoral stability is mainly affected by skeletal morphology [35]. Trochlear dysplasia, patella alta, the TT-TG distance, patella tilt, femoral anteversion, tibial torsion, and knee joint rotation are well-accepted anatomic risk factors for patellar instability [6, 19, 29]. Tibial tuberosity osteotomy, trochleoplasty, femur corrective osteotomy, and medial patellofemoral ligament reconstruction (MPFLR) are considered appropriate operations when PD is accompanied by specific patellofemoral developmental abnormalities [9, 11, 12, 40]. However, the extent to which surgical correction should be performed is still a matter of debate clinically.
Shadpour et al. [8] showed that anatomic abnormalities existed in contralateral asymptomatic patellofemoral joints in patients with UPD. Gravesen et al. [13] found that the risk of a subsequent contralateral PD in patients with UPD was 5.8%, which indicated the influence of an underlying pathomorphology in contralateral knees. Furthermore, the research of Christensen et al. [6] suggested that there was a 5.4% incidence of contralateral PD at 20 years after the onset of ipsilateral PD. This finding suggested that contralateral anatomic parameters may differ from those in ipsilateral knees, leading to a low risk of contralateral PD and a large proportion of UPD cases. Therefore, being aware of the inter-limb differences in anatomical variables is important for determining the morphology of both patellofemoral joints in patients with UPD.
Trochlear dysplasia and patella alta have been verified to be the main causes of PD [14]. Moreover, patella alta and trochlear dysplasia in the affected knee are considered predictive factors for subsequent contralateral PD after the first dislocation [6]. The reasons why patella alta and trochlear dysplasia can predict contralateral PD are unclear, and analysis from an anatomic perspective may be required. Inter-limb differences in anatomic parameters are not well known.
Given the insufficient knowledge in the current literature, the purpose of this study was to determine the differences in anatomic parameters between ipsilateral dislocated knees and contralateral non-dislocated knees in patients with UPD and to identify any variations in ipsilateral knees contributing to contralateral anatomic abnormalities.
Materials and methods
This study was approved by the institutional review board of the First Affiliated Hospital of Chongqing Medical University, China (IRB NO. 2019–228). And the informed consent requirement was waived. A total of 82 patients diagnosed with PD from 2016 to 2019 were initially identified in the Electronic Medical Record System, and the CT images and lateral radiographs of both knees were retrospectively retrieved from the picture archiving and communication system (PACS). The inclusion criteria were as follows: the patient had been diagnosed with UPD, which had been verified by two coauthors; the patient had undergone CT scans of bilateral hips, knees, and ankles simultaneously; and the patient had lateral radiographs of both knees. Patients with bilateral PD, and insufficient radiological data to carry out all the measurements, or a history of trauma or previous operation that may influence the reliability of the measurements of either of the lower limbs were excluded from this study.
Among all the patients, 23 patients who had insufficient radiographic data, 11 patients who suffered from bilateral PD, one patient who had a history of tibial transverse fracture, and one patient who previously underwent an operation on a lower limb (MPFLR in another hospital) were excluded. Consequently, 46 patients were included in this study and regularly followed up.
Computed tomography technique
Images were obtained by a CT scanner (Siemens Somatom Perspective, Germany) in our hospital within seven days after the first dislocation, ranging from the anterior superior iliac spine to the toes. Inspections were conducted in the supine position with the knees in full extension bilaterally and the foot positioned in 90° flexion. The scanning parameters were as follows: tube voltage, 130 kVp; tube current 110–140 mAs; scanning layer thickness and layer spacing, both 1 mm; and matrix, 512 × 512 pixels. The field of view (FOV) varied with the individual characteristics of the patients, ranging from 220 to 450 mm.
Radiological assessment
A total of 46 patients were available for complete radiological analyses with bilateral CT of the lower limbs and lateral radiographs of the knee joints. Two knee specialists retrospectively evaluated the radiological data and medical history of all the patients and identified the patients with UPD. The CT images and radiographs were analyzed by two experienced orthopedists in a blinded and randomized fashion using the PACS workstation, and the TT-TG distance, femoral torsion, tibial torsion, knee joint rotation, patella tilt, patellar height, lateral trochlea inclination (LTI), trochlear depth, and trochlear dysplasia of Dejour were assessed. Discussions regarding distinct discrepancies in parameters, particularly in trochlear dysplasia of Dejour, were conducted among no less than two coauthors until a consensus was reached. In accordance with previous literature [7, 36], the anatomic parameters were measured via the currently used software on CT images, which provided measurement accurate to one decimal point for both the angle measurements (femoral torsion, tibial torsion, knee joint rotation, and patella tilt) and the length measurements (TT-TG distance, trochlear depth) in this study. The intraclass correlation coefficients (ICC) of the parameter were > 0.75, which showed excellent agreement.
Measurements
Brady et al. [3, 4] showed that there were no significant differences (regardless of which reference point was chosen) among the methods introduced in the current literature when the TT-TG distance was measured on CT images. The most superficial aspect of the bony tibial tubercle at the insertion of the patellar tendon and the most proximal view where the groove could be identified were considered as the reference axial images to measure the TT-TG distance. It was defined as the distance between the tibial tubercle and femoral trochlear groove (Fig. 1) [15].
Tibial tubercle to trochlear groove distance. a Axial CT image, depicting the posterior condylar reference line (PCRL) and its perpendicular line through the deepest portion of the trochlear groove (TL or TGL, trochlear groove line). b Axial CT image at the insertion of the tibial tendon into tibial tuberosity (TT). c Superimposing A and B, the line perpendicular to PCRL, paralleling to TGL was drawn through the superficial aspect of TT (TTL, tibial tubercle line), the distance between TTL and TGL is defined as TT-TG distance
Seitlinger et al. [30] described a new method to evaluate femoral torsion and considered an alternative method for the selection of the target segment for osteotomy. Four lines drawn in four different segments of the femur, were used to derive five femoral torsion parameters (total femoral torsion, neck torsion, mid torsion, distal torsion, and shaft torsion) (Fig. 2). Total femoral torsion > 20° was defined as abnormal, but the pathological value of each segmental rotational parameter was unclear.
Four segments of the femur are selected. a The slice in which the entire femoral head and neck are displayed, the line was drawn through the center of the femoral head and neck. b The line was drawn through the center of the femur and the midpoint of the lesser trochanter. c The line was tangent to the posterior aspect of the femur on the slice just above the attachment of the gastrocnemius. d The Line was tangent to the dorsal femoral condyles
Patella tilt was defined as the angle between the dorsal femoral condylar line (a line tangent to the bilateral posterior condyle) and patellar width line (the transverse axis of the patella) (Fig. 3) [16]. Tibial torsion was assessed by measuring the angle between the dorsal tibia condylar line and a line through the midpoints of the medial and lateral malleoli) [15]. Knee joint rotation was defined as the angle between the dorsal femoral condylar line and the proximal tibial condylar line (a line tangent to the bilateral posterior condyles) [20].
The criteria used for the Dejour classification of trochlear dysplasia are the same as those described in the literature for axial CT scans: type A corresponds to a shallow trochlea; type B corresponds to a flat or convex trochlea; type C corresponds to asymmetry of the trochlear facets with a convex medial trochlear wall; and type D corresponds to asymmetry of the trochlear facets with cliff patterns. The most proximal axial image showing the entire width of the trochlea was selected. Lippacher et al. [21] found that a 2-grade analysis showed excellent agreement and considered Dejour type A and type B-D to be low-grade and high-grade trochlear dysplasia, respectively.
Nelitz et al. [23] indicated that quantitative measurements of the femoral trochlea were of limited value for the assessment of trochlear dysplasia. The zone of interest for trochleoplasty [28] is located a few slices above the posterior femoral condyle and marks the entry of the trochlea. Anatomic parameters measured in this zone may better reflect trochlear dysplasia. It is difficult to identify the lateral trochlear facet near the entry of the trochlea, especially in patients with high-grade trochlear dysplasia. On the other hand, Paiva et al. [24] suggested that LTI was the single most important objective criterion for the evaluation of trochlear dysplasia. Trochlear depth is also a reliable parameter reflecting trochlear dysplasia. Different techniques have been used to measure LTI. On the basis of the current literature, LTI was defined as the angle between the line tangent to the lateral aspect of the femoral trochlea and the dorsal femoral condylar line; the trochlear depth was defined as the depth of the groove, which was derived from the medial and lateral femoral trochlea facets (Fig. 4).
LTI and trochlear depth Point A, B, and C are the highest point of the lateral trochlear facet, the deepest point of the trochlea, and the highest point of the medial trochlear facet respectively. a, b, and c is the vertical distance between point A, B, C, and femur posterior condylar line (PCRL), respectively. Lateral trochlear facet inclination is the angle between AB and PCRL; trochlea depth is calculated by a formula: [(a + c)/2-b]
Patellar height was calculated by the Insall-Salvati index, which is considered the most reliable measurement that reflects patellar height [34]. The ratio of the length of the patellar tendon to the maximum length of the patella (measured from the distal pole to the proximal pole of the patella) on a lateral plain radiograph is called the Insall-Salvati index, with values higher than 1.2 indicating patella alta.
Statistical analysis
The average values of the variables measured by both observers were used for all analyses. Statistical analysis was conducted by a co-author independently using SPSS software (version 21.0; IBM Corp). Paired t tests and Mann–Whitney U tests were conducted to assess the differences, and binary logistic regression was used to verify the specific correlations between the two sides. Statistical significance was set at P < 0.05. The ICC and weighted kappa coefficient were used to assess the interobserver reliability of each parameter, with values more than 0.75 indicating excellent agreement.
G-Power software (version 3.1) was used to perform power analysis. For a large effect size, regarding the difference in the TT-TG distance between the two lower limbs, the results indicated that at least 42 patients were needed in our study (α, 0.05; power, 0.9).
Results
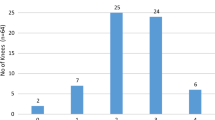
The study included 46 patients with UPD (32 females and 14 males, mean age ± SD 20.5 ± 6.8) (Table 1). At the final follow-up, no patients suffered from contralateral PD. The ICC, weighted kappa coefficient, and 95% confidence interval (95% CI) of each parameter are displayed in Table 2, all of which showed excellent agreement. The differences between the bilateral anatomic parameters are shown in Table 3. The ipsilateral TT-TG distance (P = 0.004), patella tilt (P = 0.001), and patellar height (P = 0.01) were larger in the ipsilateral knees than in the contralateral knees. The LTI in the contralateral knees was larger than that in the ipsilateral knees (P = 0.022). The Dejour classification of contralateral femoral trochlear dysplasia was not as severe as that of ipsilateral dysplasia (P = 0.036). The differences between two sides in femoral anteversion, tibial torsion, knee joint rotation, and trochlear depth were not statistically significant (n.s).
The specific correlations between the ipsilateral parameters and contralateral anatomic abnormalities assessed via binary logistic regression are shown in Table 4. When abnormalities in the contralateral anatomic parameters were regarded as dependent variables and the ipsilateral anatomic parameters of interest were regarded as independent variables, only ipsilateral LTI revealed significant ORs of 8.83 (P = 0.016, 95% CI (1.49, 52.24)) and 7.64 (P = 0.018, 95% CI (1.42, 41.19)) with regard to contralateral abnormal tibial torsion and LTI, respectively. The TT-TG distance, patella alta, patella tilt, and Dejour classification of trochlear dysplasia in the ipsilateral knees were independent of contralateral morphological abnormalities (n.s).
Discussion
In this study, the inter-limb differences and correlations of anatomic parameters of interest were studied. The most important finding of the present study was that the degrees of abnormality of ipsilateral anatomic parameters (TT-TG distance, patella tilt, patellar height, LTI, and trochlear dysplasia) were severe compared to those in the contralateral knees in patients with UPD; and the risks of contralateral pathological tibial torsion and LTI were 8.8- and 7.6-fold higher, respectively, in patients with abnormal ipsilateral LTI.
Trochlear dysplasia is the main risk factor for PD, and LTI is the single most important objective criterion for the evaluation of trochlear dysplasia [21, 23]. Anatomically, we found that, in patients with abnormal ipsilateral LTI, the risk of contralateral pathological tibial torsion and LTI were 8.8 and 7.6-fold higher, respectively, demonstrating that ipsilateral trochlear dysplasia may contribute to contralateral patellofemoral morphological abnormalities. However, additional studies are needed to determine whether the findings in this study explain the results reported by Parikh et al., which showed that the presence of ipsilateral trochlear dysplasia had an OR of 8.7 for subsequent contralateral patellar instability [25].
The risk of subsequent contralateral PD for patients with UPD has been reported to be 5.4% to 5.8% in previous studies [6, 13]. There is a paucity in literature concerning bilateral PD, and most existing studies are case reports [18, 26, 33]. In 1995, Marcacci et al. [22] reported that the rate of bilateral recurrent PD was 36/125 (28.8%). Balcarek et al. [1] reported that the rate of bilateral recurrent patellar instability was 12/61 (19.67%). In this study, the rate of bilateral PD was 11/82 (13.41%). The risk of subsequent contralateral patellar dislocation and/or instability can remain low when dangerous actions of the knee joints are avoided, a protective device is worn over the knee, and the quadriceps muscles are strengthened after the first PD. In addition, the mean follow-up time of the patients enrolled in this study was far less than 10 years. Some of the patients may develop contralateral PD in the future, thereby leading to potential bias of the results.
However, the contralateral anatomic morphology could also play a role in subsequent PD, and this relationship is not fully understood. In this study, the results showed that contralateral trochlear dysplasia was not as severe as ipsilateral patellofemoral dysplasia. Moreover, the TT-TG distance, patellar height, and patella tilt in the contralateral knees were smaller than those in the ipsilateral knees, which indicated that the contralateral patellofemoral joints were more stable than were the ipsilateral joints. When there are abnormalities in the anatomic parameters on the affected side that required surgical osteotomy correction, restoration of the anatomy to the normal range is needed or consistent with the non-dislocated contralateral patellofemoral joints was sufficient. Additional research is needed to confirm this idea.
Patella alta is an important risk factor for PD, so patella entry into the sulcus requires a larger knee flexion angle, which is considered to occur with an Insall-Salvati index value > 1.2 [29]. Parikh et al. [25] reported that ipsilateral patella alta was a risk factor for contralateral PD in patients with UPD. In this study, patellar height was not shown to be directly associated with contralateral anatomic abnormalities, which suggested that ipsilateral patellar height may not be a reasonable risk parameter for contralateral PD.
The TT-TG distance is an alternative to the Q angle, and indirectly reflects tibial tubercle lateralization, and increases the stress on the lateral patellofemoral joints [31]. Values of ≥ 20 mm on CT images are considered pathological. Because the TT-TG distance varies according to the angle of knee flexion, femoral tibial malrotation, and the presence of trochlear dysplasia, the tibial tubercle-Roman arch (TT-RA) distance, and the tibial tubercle-to-posterior cruciate ligament (TT-PCL) distance were proposed to be alternative measurements that reliably and reproducibly reflect tibial tubercle lateralization [37, 38]. Carlson et al. [5] proposed that the TT-TG distance was higher in patients with anterior knee pain than in controls. Patients with contralateral symptomatic knees were not excluded from this study, such as those with anterior knee pain, which may have led to an increase in the contralateral TT-TG distance. And ipsilateral TT-TG distance was not statistically correlated with contralateral abnormalities, which is in accordance with the results reported by Christensen showing that the TT-TG distance cannot predict contralateral PD.
Femoral anteversion could cause an imbalance in forces around the patellofemoral joints, contributing to patellar instability [30]. Moreover, increased internal femoral torsion has been verified to contribute to a lateralizing effect on the patella [17]. Takagi et al. [32] found that increased external tibial rotation and femoral anteversion were associated with recurrent PD. In a recent study [39], it was demonstrated that high femoral anteversion was associated with a dysplastic trochlear morphology. In this study, the difference between limbs in femoral anteversion and tibial torsion were not significant. The reason why the patella tilt was larger in the ipsilateral knees than in the contralateral knees could be that the patella tilt was larger in the patients with MPFL rupture after PD. We assumed that increased external patella tilt was the result of MPFL injury rather than a risk factor for PD.
However, our study had several limitations. Some risk factors were not included in this study, such as demographic risk factors and the mechanism of injury [25]. Moreover, the mutual effects and correlations among different segmental femoral rotational parameters were not researched thoroughly. A dynamic analysis focusing on the relationship between limbs in measurements as knee joint flexion angle changing was not conducted. Only the Insall-Salvati ratio for patellar height was calculated, and it is not clear whether the Caton-Deschamps index or the patellofemoral index would have provided the same results. In this study, the rate of bilateral PD was not as high as that reported in previous literature, and bias may have resulted from the inclusion of patients who may suffer from contralateral PD in the future. Additional follow-ups are necessary. Since this study was based on CT measurements and contralateral MRI scans of the knee joints were not performed, LTI measurements on the first 1–3 MRI slices near the entrance of the femoral trochlea could not be obtained. Future research regarding this issue is needed. Recent studies [2, 27] have shown that an elevated TT-TG distance and a high rate of recurrent PD are more likely to be detected in skeletally immature patients. Patients with skeletal maturity and immaturity were not completely separated in this study. Subsequent research should focus on whether the correlations between limbs in anatomic parameters in this study change with age or the angle of knee flexion.
Conclusion
In patients with unilateral patellar dislocation, the ipsilateral TT-TG distance, patella tilt, and patellar height values were larger in the ipsilateral knees than in the contralateral knees, and trochlear dysplasia was more severe in the ipsilateral joints. The risks of contralateral pathological tibial torsion and LTI were 8.8- and 7.6-fold higher, respectively, in patients with abnormal ipsilateral LTI.
References
Balcarek P, Oberthür S, Hopfensitz S, Frosch S, Walde TA, Wachowski MM et al (2014) Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc 22:2308–2314
Bayhan IA, Kirat A, Alpay Y, Ozkul B, Kargin D (2018) Tibial tubercle-trochlear groove distance and angle are higher in children with patellar instability. Knee Surg Sports Traumatol Arthrosc 26:3566–3571
Brady JM, Rosencrans AS, Shubin Stein BE (2018) Use of TT-PCL versus TT-TG. Curr Rev Musculoskelet Med 11:261–265
Brady JM, Sullivan JP, Nguyen J, Mintz D, Green DW, Strickland S et al (2017) The tibial tubercle-to-trochlear groove distance is reliable in the setting of trochlear dysplasia, and superior to the tibial tubercle-to-posterior cruciate ligament distance when evaluating coronal malalignment in patellofemoral instability. Arthroscopy 33:2026–2034
Carlson VR, Boden BP, Shen A, Jackson JN, Yao L, Sheehan FT (2017) The tibial tubercle-trochlear groove distance is greater in patients with patellofemoral pain: implications for the origin of pain and clinical interventions. Am J Sports Med 45:1110–1116
Christensen TC, Sanders TL, Pareek A, Mohan R, Dahm DL, Krych AJ (2017) Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med 45:2105–2110
Dagneaux L, Bin Abd Razak HR, Laumonerie P, Faizhan A, LiArno S, Wellings P et al (2021) Bony asymmetry in patellofemoral morphology and risk factors of instability are mostly clinically negligible. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06413-7
Demehri S, Thawait GK, Williams AA, Kompel A, Elias JJ, Carrino JA et al (2014) Imaging characteristics of contralateral asymptomatic patellofemoral joints in patients with unilateral instability. Radiology 273:821–830
Erickson BJ, Nguyen J, Gasik K, Gruber S, Brady J, Shubin Stein BE (2019) Isolated medial patellofemoral ligament reconstruction for patellar instability regardless of tibial tubercle-trochlear groove distance and patellar height: outcomes at 1 and 2 years. Am J Sports Med 47:1331–1337
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA et al (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Franciozi CE, Ambra LF, Albertoni LJ, Debieux P, Rezende FC, Oliveira MA et al (2017) Increased femoral anteversion influence over surgically treated recurrent patellar instability patients. Arthroscopy 33:633–640
Franciozi CE, Ambra LF, Albertoni LJB, Debieux P, Granata GSM Jr, Kubota MS et al (2019) Anteromedial tibial tubercle osteotomy improves results of medial patellofemoral ligament reconstruction for recurrent patellar instability in patients with tibial tuberosity-trochlear groove distance of 17 to 20 mm. Arthroscopy 35:566–574
Gravesen KS, Kallemose T, Blønd L, Troelsen A, Barfod KW (2018) High incidence of acute and recurrent patellar dislocations: a retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg Sports Traumatol Arthrosc 26:1204–1209
Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA (2019) Factors associated with an increased risk of recurrence after a first-time patellar dislocation: a systematic review and meta-analysis. Am J Sports Med 48:2552–2562
Kaiser P, Konschake M, Loth F, Plaikner M, Attal R, Liebensteiner M et al (2020) Derotational femoral osteotomy changes patella tilt, patella engagement and tibial tuberosity trochlear groove distance. Knee Surg Sports Traumatol Arthrosc 28:926–933
Kaiser P, Loth F, Attal R, Kummann M, Schuster P, Riechelmann F et al (2020) Static patella tilt and axial engagement in knee extension are mainly influenced by knee torsion, the tibial tubercle-trochlear groove distance (TTTG), and trochlear dysplasia but not by femoral or tibial torsion. Knee Surg Sports Traumatol Arthrosc 28:952–959
Kaiser P, Schmoelz W, Schoettle P, Zwierzina M, Heinrichs C, Attal R (2017) Increased internal femoral torsion can be regarded as a risk factor for patellar instability - A biomechanical study. Clin Biomech (Bristol, Avon) 47:103–109
Kuroda Y, Matsushita T, Matsumoto T, Kawakami Y, Kurosaka M, Kuroda R (2014) Bilateral medial patellofemoral ligament reconstruction in high-level athletes. Knee Surg Sports Traumatol Arthrosc 22:2465–2469
Levy BJ, Tanaka MJ, Fulkerson JP (2020) Current concepts regarding patellofemoral trochlear dysplasia. Am J Sports Med. https://doi.org/10.1177/0363546520958423363546520958423
Lin KM, James EW, Aitchison AH, Schlichte LM, Wang G, Green DW (2021) Increased tibiofemoral rotation on MRI with increasing clinical severity of patellar instability. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06382-x
Lippacher S, Dejour D, Elsharkawi M, Dornacher D, Ring C, Dreyhaupt J et al (2012) Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med 40:837–843
Marcacci M, Zaffagnini S, Iacono F, Visani A, Petitto A, Neri NP (1995) Results in the treatment of recurrent dislocation of the patella after 30 years’ follow-up. Knee Surg Sports Traumatol Arthrosc 3:163–166
Nelitz M, Lippacher S, Reichel H, Dornacher D (2014) Evaluation of trochlear dysplasia using MRI: correlation between the classification system of Dejour and objective parameters of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 22:120–127
Paiva M, Blønd L, Hölmich P, Steensen RN, Diederichs G, Feller JA et al (2018) Quality assessment of radiological measurements of trochlear dysplasia; a literature review. Knee Surg Sports Traumatol Arthrosc 26:746–755
Parikh SN, Lykissas MG, Gkiatas I (2018) Predicting risk of recurrent patellar dislocation. Curr Rev Musculoskelet Med 11:253–260
Rebolledo BJ, Nam D, Cross MB, Green DW, Sculco TP (2012) Familial association of femoral trochlear dysplasia with recurrent bilateral patellar dislocation. Orthopedics 35:e574-579
Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ (2018) High rate of recurrent patellar dislocation in skeletally immature patients: a long-term population-based study. Knee Surg Sports Traumatol Arthrosc 26:1037–1043
Schöttle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J (2005) Trochleaplasty for patellar instability due to trochlear dysplasia: a minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop 76:693–698
Seitlinger G, Ladenhauf HN, Wierer G (2018) What is the chance that a patella dislocation will happen a second time: update on the natural history of a first time patella dislocation in the adolescent. Curr Opin Pediatr 30:65–70
Seitlinger G, Moroder P, Scheurecker G, Hofmann S, Grelsamer RP (2016) The Contribution of Different Femur Segments to Overall Femoral Torsion. Am J Sports Med 44:1796–1800
Stephen JM, Lumpaopong P, Dodds AL, Williams A, Amis AA (2015) The effect of tibial tuberosity medialization and lateralization on patellofemoral joint kinematics, contact mechanics, and stability. Am J Sports Med 43:186–194
Takagi S, Sato T, Watanabe S, Tanifuji O, Mochizuki T, Omori G et al (2018) Alignment in the transverse plane, but not sagittal or coronal plane, affects the risk of recurrent patella dislocation. Knee Surg Sports Traumatol Arthrosc 26:2891–2898
Tokgöz MA, Çavuşoğlu AT, Ayanoğlu T, Elma T, Vural A (2017) Neglected bilateral congenital dislocation of the patella. Eklem Hastalik Cerrahisi 28:128–131
Verhulst FV, van Sambeeck JDP, Olthuis GS, van der Ree J, Koëter S (2020) Patellar height measurements: Insall-Salvati ratio is most reliable method. Knee Surg Sports Traumatol Arthrosc 28:869–875
Xiong R, Chen C, Yin L, Gong X, Luo J, Wang F et al (2018) How Do Axial Scan Orientation Deviations Affect the Measurements of Knee Anatomical Parameters Associated with Patellofemoral Instability? A Simulated Computed Tomography Study. J Knee Surg 31:425–432
Xu Z, Zhang H, Chen J, Mohamed SI, Zhou A (2020) Femoral anteversion is related to tibial tubercle-trochlear groove distance in patients with patellar dislocation. Arthroscopy 36:1114–1120
Xu Z, Zhang H, Fu B, Mohamed SI, Zhang J, Zhou A (2020) Tibial tubercle-roman arch distance: a new measurement of patellar dislocation and indication of tibial tubercle osteotomy. Orthop J Sports Med 8:2325967120914872
Xu Z, Zhang H, Yan W, Qiu M, Zhang J, Zhou A (2021) Validating the role of tibial tubercle-posterior cruciate ligament distance and tibial tubercle-trochlear groove distance measured by magnetic resonance imaging in patients with patellar dislocation: a diagnostic study. Arthroscopy 37:234–242
Yang G, Dai Y, Dong C, Kang H, Niu J, Lin W, et al. (2020) Distal femoral morphological dysplasia is correlated with increased femoral torsion in patients with trochlear dysplasia and patellar instability. Bone Joint J 102-b:868–873
Zhang Z, Zhang H, Song G, Wang X, Zhang J, Zheng T et al (2020) A high-grade J sign is more likely to yield higher postoperative patellar laxity and residual maltracking in patients with recurrent patellar dislocation treated with derotational distal femoral osteotomy. Am J Sports Med 48:117–127
Acknowledgements
None.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by PZ, LY and ZX. The first draft of the manuscript was written by JC, and modified by XH. HZ and AZ provided theoretical supports and retrospectively verify the diagnosis of unilateral patellar dislocation of all patients. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no financial interests.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University. (Number: 2019–228).
Consent to participate
The informed consent was waived by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University in view of the retrospective nature of the study.
Availability of data and material
The data used to support the findings of this study are available from the corresponding author upon request.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, J., Huang, X., Xu, Z. et al. Ipsilateral patellofemoral morphological abnormalities are more severe than those of contralateral joints in patients with unilateral patellar dislocation. Knee Surg Sports Traumatol Arthrosc 29, 2709–2716 (2021). https://doi.org/10.1007/s00167-021-06539-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06539-2