Abstract
Purpose
To analyze the effects of increased medial proximal tibial angle (MPTA) on the clinical outcomes and cartilage deterioration in the lateral compartment after a mean follow-up period of 4 years following open-wedge high tibial osteotomy (OWHTO) using propensity score matching (PSM) analysis.
Methods
Among 376 knees treated with OWHTO for medial unicompartmental osteoarthritis with varus deformity, 36 knees with MPTA increase of > 95° and 108 knees with MPTA increase of < 95° at the final follow-up were included. The baseline prognostic factors [age, sex, preoperative hip–knee–ankle (HKA) angle, body mass index, and preoperative knee range of motion] were equalized between the 2 groups using PSM; consequently, 31 pairs of patients were compared. The radiographic and clinical outcomes, including lateral compartment pain, were assessed. For 18 patients in each group, second-look arthroscopy and cartilage status assessment were performed.
Results
The preoperative demographics were similar between the groups. At the final follow-up, the HKA angle and joint line obliquity were significantly higher in the increased MPTA group. No significant differences were observed in the clinical outcomes between the groups. On second-look arthroscopy, significant cartilage deterioration of the lateral compartment was not observed in either group. Pain in the lateral compartment was experienced significantly more frequently in the increased MPTA group (p < 0.01).
Conclusion
Although excessively increased MPTA after HTO had no significant effects on the clinical outcomes and cartilage deterioration in the lateral compartment at the minimum 4-year follow-up, lateral compartment pain was experienced significantly more frequently in the increased MPTA group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In general, OWHTO is commonly associated with an increased medial proximal tibial angle (MPTA; angle between the mechanical axis of the tibia and the articular surface of the medial proximal tibia) or joint line obliquity (JLO; angle formed by the line parallel to the ground and the tangent to the proximal tibia after HTO) postoperatively. Several previous studies have reported on the MPTA and JLO. Hernigou et al. demonstrated that only 5 of 75 knees with valgus correction showed lateral compartment osteoarthritic changes on plane radiography after OWHTO [10]. However, Babis et al. reported that increased JLO after an increase in the MPTA may result in increased shear stress at the knee joint. They further demonstrated that a JLO of < 4° was associated with 100% survival at 5 and 10 years after closing-wedge HTO [3]. In a biomechanical study, Nakayama et al. reported that increased JLO in the proximal tibia, defined by an MPTA > 95°, led to eccentric valgus shear stress on the articular cartilage [17]. Although an increased MPTA or JLO may induce valgus shear stress on the lateral compartment, the effects of increased MPTA on the clinical outcomes and cartilage deterioration in the lateral compartment after OWHTO are still unknown. Moreover, previous studies did not control for preoperative confounding factors that influence postoperative outcomes, such as age, sex, preoperative hip–knee–ankle (HKA) angle, and body mass index (BMI). Therefore, the purpose of this study was to analyze the effects of increased MPTA on the clinical outcomes and cartilage deterioration in the lateral compartment in patients who underwent OWHTO with a mean follow-up of 5 years using propensity score matching (PSM) analysis. The hypothesis was that increased postoperative MPTA would induce cartilage deterioration in the lateral compartment of the knee joint after OWHTO.
Materials and methods
Study design
Between January 2006 and May 2014, 553 patients (553 knees) diagnosed with medial unicompartmental osteoarthritis with varus deformity underwent medial OWHTO performed by two senior surgeons in our hospital. This study was approved by the Institutional Review Board of Chonnam National University Hwasun Hospital (CNUHH-2020–195). Written consent was obtained from all patients. The surgical indications were as follows: symptomatic medial unicompartmental osteoarthritis of the knee, age > 40 years, diagnosis using supine anteroposterior plain radiographs (Kellgren–Lawrence grade ≥ III); > 5° varus of the mechanical axis; < 5° flexion contracture; and a bony correction angle requirement of < 15°, as calculated preoperatively. Ten patients who underwent simultaneous ligament reconstruction were excluded, as were 167 patients who did not visit the hospital in the 4 years after surgery. The 376 knees were divided according to the postoperative MPTA at the final follow-up. The MPTA at final follow-up was > 95° in 65 knees (17.2%) and ≤ 95° in 311 knees (82.7%).
Propensity score matching
For comparison of the two groups, this study equalized the baseline prognostic factors of the two groups using PSM. The propensity score was calculated with the baseline variables using logistic regression analysis. The propensity score was based on the following baseline covariates: age, sex, preoperative HKA angle, BMI, and preoperative knee range of motion (ROM). One-to-one matching was performed using a variable-ratio, parallel, and balanced nearest-neighbor approach. During matching, this study used a caliper width of 0.2 standard deviation (SD) of the propensity score to limit the allowed distance between two matched patients. The PSM yielded 31 pairs of patients. The MPTA at the final follow-up was > 95° in 31 knees (group A) and ≤ 95° in another 31 knees (group B; Fig. 1).
Surgical procedure
Preoperative planning indicated that the postoperative mechanical axis would pass across the knee at the Fujisawa point (a point at 62.5% of the cross-sectional diameter of the tibial plateau) in accordance with Miniaci’s method [7]. Diagnostic arthroscopies were performed before the osteotomy. Cartilage defects or meniscal tears on the medial side were managed with microfracture or debridement according to the surgeon’s judgment. Arthroscopy was followed by a biplanar opening wedge HTO. A longitudinal skin incision was made 7 cm medial to the patellar tendon over the pes anserinus tendons. The posteromedial surface was exposed after soft tissue dissection. The osteotomy plane was marked with the help of guide wires, whose positions were confirmed on an image intensifier. The two guide wires were drilled in parallel from the medial to lateral cortex obliquely, exactly at the level of the tibiofibular joint. A transverse cut was made parallel to the wires, up to a distance of 15 mm medial to the patellar tendon. Then, the second cut was made behind the tibial tuberosity, approximately 120° angulated with the first cut. The osteotomy was opened and fixed with two Aescula plates (Medyssey, Seoul, Korea) or a locking compression plate. Bone grafting was performed when the tibial opening was > 10 mm. For postoperative rehabilitation, range-of-motion exercises were started as soon as possible, and a ROM brace was worn around the knee for 4 weeks. Toe touch partial weight-bearing was allowed for the first 4 weeks after surgery, and subsequently, progressive tolerable weight-bearing was encouraged.
Radiological and clinical evaluations
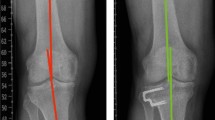
The patients were followed for a minimum of 4 years after the operation. Supine anteroposterior and lateral radiographs and standing anteroposterior hip-to-ankle radiographs were obtained preoperatively and at each follow-up. The MPTA, JLO, and HKA angle on standing anteroposterior hip-to-ankle radiographs (Fig. 2) and the posterior tibial slope on the lateral plain radiograph were measured before surgery and at the latest follow-up. The HKA angle in varus alignment was marked negatively. For clinical evaluation, postoperative ROM, Knee Society Score (pain and function), Western Ontario and McMaster Universities (WOMAC) scoring system, and Hospital for Special Surgery (HSS) score were used. Patients were also checked for pain in the lateral compartment of the knee, defined as pain localized to the lateral aspect of the knee with a visual analog scale score of > 3. An independent blinded orthopedic surgeon who did not participate in the surgeries recorded the preoperative and latest follow-up measurements to assess the clinical and radiological outcomes, except ROM.
a The hip–knee–ankle (HKA) angle was defined as the axis between the femoral mechanical axis and the tibia mechanical axis. b The anatomic medial proximal tibial angle (MPTA) was defined as the medial angle between the tibial anatomic axis and the joint line of the proximal tibia. Joint line obliquity (JLO) was defined as the angle between a line parallel to the ground and the tangent to the femoral condyles, and a positive JLO value denoted lateral inclination of the joint line
Second-look arthroscopy assessments
Second-look arthroscopy was performed during plate removal. All patients were recommended for implant removal. During the procedure, cartilage lesions were macroscopically evaluated after the arthroscopic procedure. The lateral compartment articular surface of the femorotibial joint was evaluated using the arthroscopic grading system of the International Cartilage Repair Society, ICRS [4]. Cases with superficial abrasion and fissures were defined as grade 1; those with cartilage defects where lesions extended down to < 50% of the cartilage depth were defined as grade 2; those with lesions extending down to > 50% but not involving the subchondral bone were defined as grade 3; and those with defects involving the subchondral bone were defined as grade 4. Cartilage regeneration was evaluated on the basis of the regeneration stage at the time of second-look arthroscopy and implant removal (Fig. 3). A total of 18 patients underwent a second-look arthroscopy when the degree of MPTA was > 95°, and another 18 patients underwent a second-look arthroscopy when the degree of MPTA was < 95°. The second-look arthroscopy was performed before the removal of plates and screws at a mean of 12.5 months after the initial OWHTO (range 10–15 months) in group A and 13.1 months after the initial OWHTO (range 11–14 months) in group B (n.s.).
a Plain knee radiograph of a 57-year-old female with a preoperative varus deformity. b Arthroscopic findings of ICRS grade zero in the lateral compartment of Lt knee. c Plain knee radiograph of a 57-year-old female with a postoperative MPTA at 1 year after 1st operation. d 2nd look arthroscopic findings of ICRS grade II in the lateral compartment of Lt knee
Statistical analyses
SPSS version 22 for Windows (IBM, Armonk, NY) was used for the statistical analysis. To test the reliability of the data, the radiological results were measured again after 1 week by a blinded orthopedic surgeon who did not participate in the surgeries. A Pearson correlation coefficient analysis was performed to estimate the reliability and revealed good test–retest reliability (r > 0.8). The normal distribution was checked using the Shapiro–Wilk test for continuous variables. For analysis of demographic data, an independent t-test was used to compare the parametric variables (BMI, preoperative HKA angle, preoperative MPTA, and preoperative posterior tibial slope) between the groups, while the Mann–Whitney U test was used to analyze the nonparametric variables [age, follow-up, clinical results (except lateral compartment pain), postoperative HKA angle, and postoperative MPTA]. A comparison of preoperative and postoperative clinical and radiological results was performed using a paired t-test for parametric variables and the Wilcoxon signed-rank test for nonparametric variables (clinical results and HKA angle). A χ2 test was used to analyze all the categorical variables (sex, ICRS grade, and lateral compartment pain). A p value < 0.05 was considered statistically significant. A prior assessment confirmed the estimated group size on the basis of the presence of lateral knee pain at minimum 4-year follow-up in 25 patients from the 2 groups. A statistical assessment was performed to confirm the sample size. To obtain a power of at least 0.8 with α = 0.05, the above parameters were chosen, and a minimum of 25 patients at a 1:1 ratio in each group was calculated. Concerning compliance rates, this study enrolled as many as 31 patients in groups A and B after PSM. Post hoc analysis was performed to estimate the power of pain in the lateral compartment (power = 0.9).
Results
The PSM yielded 31 pairs of patients. All preoperative demographic data were similar between the two groups. The preoperative knee phenotypes in relation to coronal limb phenotypes were also investigated according to novel classification (Table 1) [11]. The mean preoperative HKA angles deviated from 7.5 ± 3.4 to − 2.5 ± 2.7 in group A and from 9.0 ± 3.7 to − 1.0 ± 3.5 in group B at the final follow-up (p < 0.01). The mean preoperative MPTAs deviated from 86.8 ± 1.9 to 96.1 ± 1.4 in group A and from 85.8 ± 2.6 to 90.8 ± 2.8 in group B at the final follow-up (p < 0.01; Table 2). The HSS score, Knee Society Score (KSS), and WOMAC scores were significantly improved at the final follow-up compared with their preoperative baseline values in both groups. This study found no significant differences in any clinical outcomes between groups A and B (n.s., Table 3). Pain in the lateral compartment of the knee was observed in 14 patients in group A and 3 patients in group B (p < 0.01). Medial joint OA progressed in two knees in group A, and total knee arthroplasty conversion was performed. The second-look arthroscopic assessments of cartilage regeneration using the ICRS grade are summarized in Table 4. There was no statistically significant cartilage deterioration in the lateral femoral condyle (LFC) or lateral tibial condyle (LTC) in either group after OWHTO (n.s.).
Discussion
The main findings of the present study were as follows: (1) at the final follow-up, the HKA angle and JLO were significantly higher in the increased MPTA group than in the normal group; (2) the clinical outcomes were not significantly different between the two groups; (3) no significant difference in cartilage deterioration of the LTC was found between the increased and normal MPTA groups on second-look arthroscopy; and (4) lateral compartment knee joint pain was experienced more frequently in the increased MPTA group than in the normal group.
OWHTO is a popular surgery for patients with symptomatic varus knee OA [8, 13]. However, because this operation directly changes the geometry of the proximal tibia, increased MPTA or JLO can frequently occur [2]. Recently, Feucht et al. reported that slight overcorrection is accepted (MPTA ≤ 95°), such that 172 knees of 303 knees (57%) can be corrected via isolated OWHTO, whereas 99 knees of 303 knees (33%) of patients would still require a double-level osteotomy [6]. Furthermore, this study demonstrated that the MPTA at the final follow-up was > 95° in 65 knees (17.2%) and ≤ 95° in 311 knees (82.7%). In general, a higher postoperative MPTA after OWHTO is dependent on a higher preoperative MPTA, as well as on changes in HKA angle [5]. In this study, there were no significant differences in the preoperative MPTA or HKA angle between the two groups. The mean correction angle in the increased MPTA group (10°) was similar to that in the normal group (10°). However, the HKA angle was significantly higher in the increased MPTA group (valgus, 2.5°) than in the normal group (valgus, 1.5°). Lee et al. reported that JLO was increased to 4.1° and MPTA was increased to 9.0° after OWHTO [15]. Similarly, the present study demonstrated that the mean MPTA angle was increased to 10.7° in group A and 5° in group B, and the mean postoperative JLO was estimated at 5.5° in group A and 0.9° in group B. Consequently, the change in JLO relative to the ground may be smaller than the change in MPTA. These findings suggest that increased MPTA after OWHTO may be compensated by the soft tissue in the knee and the change in the ankle joint line. Akamatsu et al. also suggested a compensatory change in the ankle joint line after OWHO [1].
This study showed apparently improved minimum 4-year follow-up clinical outcomes after OWHTO, regardless of an increased MPTA, as previous evidence showed [9]. Contrary to the authors’ expectation that the increased MPTA group would show inferior clinical outcome based on the report that increased JLO on the proximal tibia led to valgus shear stress on the articular cartilage, there were no significant differences in WOMAC score, KSS, and HSS score between the two groups. Several previous studies also showed that high MPTA or JLO after OWHTO does not correlate with clinical outcomes at short- and mid-term follow-up [9, 12, 15, 18]. However, recent studies have shown conflicting results in terms of whether high MPTA or JLO worsens the clinical outcome after OWHTO. Indeed, Schuster et al. reported in a long-term clinical study that the high MPTA group showed inferior clinical outcomes based on IKDC scores. However, long-term survivorship, defined as conversion to arthroplasty, was the same as that in the normal MPTA group, and other general results are sufficient to confirm a mild effect of increase in MPTA [20]. Akamatsu et al. divided patients into two groups according to an MPTA of 95° as a reference and reported lower knee injury and osteoarthritis outcome scores (KOOSs) in the sports and recreation subscales in the higher MPTA group. They explained that the result was due to the biomechanics arising from the shearing force caused by the lateral inclination of the tibia plateau after OWHTO [1, 17]. Similarly, the most recent evidence from Kubota et al. showed a negative correlation between the JLO after OWHTO and the clinical outcome based on the KOOSs in the pain, sports and recreation, and activities of daily living subscales [14].
The present study investigated whether a higher MPTA increased cartilage deterioration in the lateral compartment on second-look arthroscopy after OWHTO. No significant difference in cartilage regeneration in the LTC was found between the increased (> 95°) and normal (≤ 95°) MPTA groups. Similarly, Kim et al. reported that marked postoperative joint line obliquity had a negative impact on articular cartilage repair after OWHTO according to initial arthroscopy and second-look arthroscopy. However, this study investigated only the medial compartment of the knee joint [12]. In a previous animal study, no significant differences in macroscopic and microscopic structural changes in the lateral meniscus were found between sheep that received varus osteotomy and those that received valgus osteotomy 6 months after HTO [21]. In a long-term follow-up study, Hernigou et al. demonstrated that only five knees with corrected valgus showed lateral compartment osteoarthritic changes on plane radiography after OWHTO [10]. Another study investigated only 16 knees of 159 knees with corrected valgus to anatomical axis as 167° conversion to arthroplasty at final follow-up (17.9 years) [19]. Another study reported cartilage deterioration in the lateral compartment at rates of 16.3% in the LFC and 9.8% in the LTC in the increased MPTA group (> 95°) 1 year after OWHTO [1]. Another study reported that approximately 10% of patients showed deterioration in the lateral compartment cartilage with or without a pre-existing lateral cartilage lesion at short-term follow-up. They concluded that overcorrection of the knee did not accelerate the deterioration of the pre-existing lateral cartilage lesion [16]. However, the results of previous studies were considered to be partly attributable to the timing of the short-term follow-up at 1 year, and it was suggested that the progression of cartilage deterioration in the lateral compartment after OWHTO might become evident in a long-term follow-up study. Although the present study found no changes in cartilage deterioration in the lateral compartment under second-look arthroscopy approximately 1 year after OWHTO, the number of patients with lateral compartment symptoms was significantly higher in the increased MPTA group than in the normal MPTA group at final follow-up (14 vs 3). This result corresponds to Akamatsu’s finding that pain arises from shearing force caused by the lateral inclination of the tibial plateau after OWHTO [1]. In a biomechanical study, Nakayama et al. reported that increased JLO in the proximal tibia, defined by an MPTA > 95°, led to eccentric valgus shear stress on the articular cartilage, which was found to result in cartilage deterioration of the lateral compartment in a long-term follow-up study [17]. Furthermore, an in vivo study in sheep found that overcorrection significantly decreased the proliferative activity of the cells in the red–red zone of the lateral compartment [21]. This study demonstrated that significant overcorrection in the increased group contributed to an increased frequency of lateral compartment pain due to increased shear force. On the basis of these findings, long-term follow-up examinations, such as simple radiography or magnetic resonance imaging, may show cartilage deterioration in the lateral compartment after OWHTO in the future.
This study has several limitations. First, this was a retrospective study with the usual limitations and bias inherent to single-center retrospective studies. However, the use of a PSM analysis increased the sample quality, enabling us to draw solid conclusions. Second, second-look arthroscopy was not performed in all the patients and was not performed at the same time as the last clinical and radiographic follow-up examinations. The authors, therefore, believe that progression of cartilage deterioration in the lateral compartment after OWHTO may become evident in a long-term follow-up study. Third, a correlation between the clinical outcome and the size of the cartilage lesion in the lateral compartment was not observed; further studies are required to determine this association. Despite these limitations, this study showed that the increased MPTA group had significantly more frequent lateral compartment pain than the normal MPTA group. Therefore, surgeons should take care to avoid overcorrection of the MTPA over 95° or consider double-level osteotomy.
Conclusion
Contrary to the hypothesis, this study found no significant difference in terms of clinical outcomes, including cartilage deterioration in the lateral compartment of the knee joint, between the patients who showed a postoperative MPTA > 95° and those who showed a postoperative MPTA ≤ 95° after OWHTO. Regardless of the MPTA increase, OWHTO procedures provide good clinical outcomes and do not cause cartilage deterioration in the lateral compartment at a minimum of 4 years of follow-up. Although lateral compartment pain was more frequent in the increased MPTA group (> 95°), long-term follow-up studies are needed to evaluate the effect of increased MPTA after HTO to determine the correlation between MPTA and clinical outcomes.
Abbreviations
- OWHTO:
-
Open-wedge high tibial osteotomy
- OA:
-
Osteoarthritis
- MPTA:
-
Medial proximal tibial angle
- JLO:
-
Joint line obliquity
- HKA:
-
Hip–knee–ankle
- BMI:
-
Body-mass-index
- PSM:
-
Propensity score matching
- ROM:
-
Range of motion
- SD:
-
Standard deviation
- WOMAC:
-
Western Ontario and McMaster University
- HSS:
-
Hospital for Special Surgery
- ICRS:
-
International Cartilage Repair Society
- TMA:
-
Tibia mechanical angle
- VAR:
-
Varus
- NEU:
-
Neutral
- FMA:
-
Femoral mechanical angle
- VAL:
-
Valgus
- KSS:
-
Knee Society Score
- LFC:
-
Lateral femoral condyle
- LTC:
-
Lateral tibial condyle
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- CONSORT:
-
Consolidated Standards of Reporting Trials
- ADL:
-
Activities of daily living
- MFC:
-
Medial femoral condyle
- MTC:
-
Medial tibial condyle
References
Akamatsu Y, Kumagai K, Kobayashi H, Tsuji M, Saito T (2018) Effect of increased coronal inclination of the tibial plateau after opening-wedge high tibial osteotomy. Arthroscopy 34:2158–2169
Amis AA (2013) Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21:197–205
Babis GC, An KN, Chao EY, Rand JA, Sim FH (2002) Double level osteotomy of the knee: a method to retain joint-line obliquity: clinical results. J Bone Jt Surg Am 84:1380–1388
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Jt Surg Am 85(Suppl 2):58–69
El-Azab HM, Morgenstern M, Ahrens P, Schuster T, Imhof AB, Lorenz SG (2011) Limb alignment after open-wedge high tibial osteotomy and its effect on the clinical outcome. Orthopedics 34:e622–e628
Feucht MJ, Winkler PW, Mehl J, Bode G, Forkel P, Imhoff AB, Lutz PM (2020) Isolated high tibial osteotomy is appropriate in less than two-thirds of varus knees if excessive overcorrection of the medial proximal tibial angle should be avoided. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06166-3
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin N Am 10:585–608
Goshima K, Sawaguchi T, Sakagoshi D, Shigemoto K, Hatsuchi Y, Akahane M (2017) Age does not affect the clinical and radiological outcomes after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 25:918–923
Goshima K, Sawaguchi T, Shigemoto K, Iwai S, Fujita K, Yamamuro Y (2019) Comparison of clinical and radiologic outcomes between normal and overcorrected medial proximal tibial angle groups after open-wedge high tibial osteotomy. Arthroscopy 35:2898–2908
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Jt Surg Am 69:332–354
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Kim CW, Seo SS, Lee CR, Gwak HC, Kim JH, Jung SG (2017) Factors affecting articular cartilage repair after open-wedge high tibial osteotomy. Knee 24:1099–1107
Kohn L, Sauerschnig M, Iskansar S, Lorenz S, Meidinger G, Imhoff AB, Hinterwimmer S (2013) Age does not influence the clinical outcome after high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21:146–151
Kubota M, Kim Y, Sato T, Yamaguchi J, Ohno R, Kaneko K, Ishijima M (2020) The actual knee function was not influenced by joint line obliquity after open-wedge high tibial osteotomy. SICOT J 6:4
Lee KM, Chang CB, Park MS, Kang SB, Kim TK, Chung CY (2015) Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthr Cartil 23:232–238
Moon HS, Choi CH, Jung M, Park SH, Lee DY, Shin JC, Kim SH (2019) The effect of cartilage lesion in the lateral compartment of the knee on the surgical outcome of medial open-wedge high tibial osteotomy. J Knee Surg. https://doi.org/10.1055/s-0039-1697623
Nakayama H, Schröter S, Yamamoto C et al (2018) Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc 26:1873–1878
Oh KJ, Ko YB, Bae JH, Yoon ST, Kim JG (2016) Analysis of knee joint line obliquity after high tibial osteotomy. J Knee Surg 29:649–657
Sasaki E, Akimoto H, Iio K, Fujita Y, Saruga T, Kakizaki H, Ishibashi Y (2020) Long-term survival rate of closing wedge high tibial osteotomy with high valgus correction: a 15-year follow-up study. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06128-9
Schuster P, Gesslein M, Schlumberger M, Mayer P, Mayr R, Oremek D, Frank S, Schulz-Jahrsdorfer M, Richter J (2018) Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and varus malalignment. Am J Sports Med 46(6):1362–1370
Ziegler R, Goebel L, Cucchiarini M, Pape D, Madry H (2014) Effect of open wedge high tibial osteotomy on the lateral tibiofemoral compartment in sheep. Part II: standard and overcorrection do not cause articular cartilage degeneration. Knee Surg Sports Traumatol Arthrosc 22:1666–1677
Acknowledgements
No specific grant was received for this research from funding agencies in the public, commercial, or not-for-profit-sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by GWK, JKK and EKS. Review, editing and supervision by JKS.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The authors declare that there they have non-financial competing interests.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the Ethical Standards of the Institutional and National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Hwasun Chonnam National University Hospital approved this study (CNUHH-2020-195).
Informed consent
Written informed consent for participation in the study was obtained from all patients, including permission to access patient’s records and publish individual clinical details.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, G.W., Kang, J.K., Song, E.K. et al. Increased joint obliquity after open-wedge high tibial osteotomy induces pain in the lateral compartment: a comparative analysis of the minimum 4-year follow-up outcomes using propensity score matching. Knee Surg Sports Traumatol Arthrosc 29, 3495–3502 (2021). https://doi.org/10.1007/s00167-020-06342-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06342-5