Abstract
Purpose
The purpose of this systematic review and meta-analysis is to evaluate the joint awareness after unicompartmental knee arthroplasty (UKA) and total knee arthroplasty (TKA). It was hypothesized that patients with UKA could better forget about their artificial joint in comparison to TKA.
Methods
A search of major literature databases and bibliographic details revealed 105 studies evaluating forgotten joint score in UKA and TKA. Seven studies found eligible for this review were assessed for risk of bias and quality of evidence using the Newcastle–Ottawa Scale. The forgotten joint score (FJS-12) was assessed at 6 months, 1 year, and 2 years.
Results
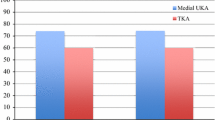
The mean FJS-12 at 2 years was 82.35 in the UKA group and 74.05 in the TKA group. Forest plot analysis of five studies (n = 930 patients) revealed a mean difference of 7.65 (95% CI: 3.72, 11.57, p = 0.0001; I2 = 89% with p < 0.0001) in FJS-12 at 2 years. Further sensitivity analysis lowered I2 heterogeneity to 31% after exclusion of the study by Blevin et al. (MD 5.88, 95%CI: 3.10, 8.66, p < 0.0001). A similar trend of differences in FJS-12 between the groups was observed at 6 months (MD 32.49, 95% CI: 17.55, 47.43, p < 0.0001) and at 1 year (MD 25.62, 95% CI: 4.26, 46.98, p = 0.02).
Conclusions
UKA patients can better forget about their artificial joint compared to TKA patients.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite advancements in implant design, surgical technique, and patient care, nearly 30% of patients believe that their expectations were not fulfilled after total knee arthroplasty (TKA) [9, 36, 41, 46]. Unicondylar knee arthroplasty (UKA), in comparison, has better patient satisfaction. It has demonstrated superior functional outcome, faster recovery, and reduced risk of peri-operative complications [3, 10, 12, 14, 31, 54]. Despite this, 25–47% of medial compartment arthritis patients who are eligible for UKA get treated with TKA [22, 53]. The higher revision risk is the crucial factor in driving surgeons towards TKA more often [13]. Recent studies have shown that the increased failure rate of UKA is associated with low-volume centers and surgeons performing a lower number of such procedures [18, 30, 37]. UKA has also been found to be more cost-effective than TKA despite having a high revision risk [26, 29, 39].
An important aspect of patient satisfaction is joint awareness [5, 14, 28, 51]. All patients expect that they will forget about the artificial joint after surgery. Accordingly, the “forgotten joint score” (FJS-12) was widely accepted as an important patient-reported outcome measure to assess the awareness of the patient towards their knee joint after the arthroplasty procedure [1, 5, 21, 35, 44, 48]. FJS-12 has low ceiling effects, and it can detect even minute differences among highly functioning individuals after knee arthroplasty [5, 15]. UKA patients have a lesser degree of knee joint pathology in the preoperative period, and these candidates are likely to be more active following their surgery [15]. Accordingly, FJS-12 can be considered as an appropriate patient-reported outcome measure in these highly active patients. Few studies reported a better FJS-12 of the artificial joint in UKA patients compared to TKA [7, 14, 17, 28, 40, 56]. However, Thienpont et al. observed no significant difference in the FJS-12 between both types of knee arthroplasties after 2 years [47]. It seems that the level of joint awareness following UKA and TKA is not well defined. Therefore, this systematic review and meta-analysis was conducted to evaluate the level of awareness of the artificial joint among patients following UKA and TKA. It was hypothesized that patients who underwent UKA had higher FJS-12 than those who underwent TKA.
Materials and methods
This systematic review/meta-analysis was performed following the guidelines of preferred reporting items for systematic reviews and meta-analyses (PRISMA) [25] (Fig. 1). It was registered in PROSPERO before data extraction and analysis (Regd no.: CRD42020198747).
A literature search was performed on 19th September 2020 by two authors (SKT, PV) to identify studies on FJS-12 evaluation in UKA and TKA. The electronic databases of PubMed/Medline, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) were searched using the keywords “Forgotten joint score”, “forget”, “total knee arthroplasty”, “total knee replacement”, “TKA”, “TKR”, “unicondylar knee arthroplasty”, “unicompartmental knee arthroplasty”, “UKA”, and “UKR”. The search was restricted to the English language and human beings [Supplementary Data, Annexure 1]. The titles and abstracts of the retrieved articles were assessed for possible inclusion in the review. Whenever there was any doubt or uncertainty, the full article was retrieved and assessed thoroughly. The bibliographic lists of the relevant articles and reviews were also searched for further potential eligibility. Any discrepancies in study selection were resolved by a discussion between the authors. A third author (TG) was consulted in the event of disagreement (Fig. 1).
The inclusion criteria for this systematic review were: (1) the study design must be a randomized controlled trial (RCT) or an observational study; (2) the study must evaluate the patient-reported outcome using FJS-12 with at least one follow-up after 6 months; (3) the study must have reported the FJS-12 in both UKA and TKA patients aged > 18 years; and (4) the study must have evaluated only medial UKA.
Studies were excluded if they had the following criteria: (1) studies that recruited morbidly obese patients with BMI > 40 kg/m2; and (2) studies that considered revision arthroplasty, infective knee, inflammatory arthritis, hemophilia, neurological disorder, or simultaneous TKA or UKA.
The FJS-12 is a 12-item questionnaire developed to evaluate the awareness of the artificial joint among arthroplasty patients during their daily activities. The FJS-12 score ranges from 0 to 100, with 0 being the worst score and 100 being the best. A higher score means the patient is better able to forget about the artificial joint in daily life. So, the higher the score, the better the outcome is [5].
Data extraction was done using a data extraction form, and two authors (SKT and PV) independently extracted data from eligible studies (author, year of publication, study design, intervention, follow-up, FJS-12 outcome at different time intervals). Any disagreement was resolved through discussion with a third author (TG).
The primary endpoint of this study was FJS-12 at two years after TKA or UKA. For the quantitative synthesis of data, studies that reported FJS-12 outcome beyond 2 years were considered as 2-year point outcome data. The FJS-12 at 6 months and 1 year was also assessed in both the groups.
The methodological quality and risk of bias of the studies were assessed independently by two authors (SKT and PV) using the Newcastle–Ottawa scale (NOS) [52] (Table 1). The NOS uses a star system with a maximum of nine stars to evaluate a study in three domains (8 items): the selection of the study groups, the comparability of the groups, and the ascertainment of the outcome of interest. Each item was allocated one star for low risk and zero stars for high risk. Studies that received a score of nine stars were considered to have low risk of bias, seven or eight stars to have a moderate risk of bias, and six or fewer stars to have a high risk of bias [52]. Any disagreements were resolved by discussion between the two authors. If no agreement could be reached, the opinion of a third author (TG) was sought.
Data were analyzed using Review Manager (RevMan) V.5.1 [42]. Data were pooled and expressed as mean difference (MD) with 95% confidence interval (CI) for the continuous data. As the outcomes in all studies were uniformly evaluated using the FJS-12 outcome tool, the mean difference was assessed. A p value of < 0.05 was considered statistically significant. The heterogeneity among the studies was assessed by Cochrane’s Q (χ2 p < 0.10) and quantified by I2. An I2 of > 50% and a p value of < 0.10 was considered as a threshold of significant heterogeneity [23, 55]. To address the high degree of heterogeneity, a random-effects model was applied in this meta-analysis [45]. Sensitivity analyses were also performed to evaluate the stability and heterogeneity of the results [23, 45, 55].
Results
A total of 105 studies were retrieved after electronic and manual searches, of which seven studies were found to be eligible for review [7, 14, 17, 28, 40, 47, 56] (Fig. 1). The study designs of four studies were prospective cohort, and three studies were retrospective comparative study. The inclusion and exclusion criteria were well defined in all the studies. The risk of bias, as evaluated using NOS, revealed low bias in one study and moderate bias in six studies.
A total of 1172 participants were included in these seven studies. There were 554 UKA patients and 618 TKA patients. Age, gender, BMI, and preoperative function score of both UKA and TKA patients in the included studies were properly matched in four studies [14, 17, 28, 40]. The gender distribution data of 100 out of 101 patients in each group were available in the study of Fabre-Aubrepsy et al. [17]. In the remaining three studies, there were significant differences in age, sex, and/or BMI [7, 47, 56]; nevertheless, the differences were small and clinically insignificant (Table 2). The indications for UKA in all studies were appropriate.
All UKA and TKA prostheses in the included studies were cemented implant except the uncemented UKA prostheses used by Peersman et al. (n = 57) [40]. Three studies (n = 245 patients) used MAKO robotic system for UKA [7, 14, 56]. The remaining four studies with 309 patients of UKA were operated with a conventional open technique [17, 28, 40, 47]. All studies reported manual TKA surgeries except a few patients of Blevin et al. [7], who were operated on with computer navigation. The details of patella resurfacing were mentioned in only three studies [28, 47, 56]. In 177 TKA surgeries, the patella was resurfaced. The implants used for both UKA and TKA were from numerous manufacturers (Table 2).
Five studies (n = 930) evaluated the FJS-12 at the end of 2 years [7, 14, 28, 40, 56] (Table 3). The average FJS-12 at 2 years in the UKA group was 82.32, and 74.05 in the TKA group. Forest plot analysis of the difference in FJS-12 between the UKA and TKA groups was statistically significant (MD 7.65, 95% CI: 3.72, 11.57, p = 0.001; I2 = 89%) (Fig. 2). As there was significant heterogeneity among studies, sensitivity analyses were performed. The study by Blevin et al. [7] was significantly affecting the mean difference (MD). The heterogeneity lowered significantly (I2 of 31%, p = 0.22) when this study was excluded (Table 4).
Only two studies reported the FJS-12 at 6 months (n = 239) [14, 40] (Table 3). The mean difference in FJS-12 between UKA (n = 87) and TKA (n = 152) at 6 months was statistically significant (MD 32.49, 95% CI: 17.55, 47.43, p < 0.0001) (Fig. 3). Even at the end of 1 year (reported in two studies, n = 229), TKA patients were more aware of their joint compared to UKA (MD 25.62, 95% CI: 4.26, 46.98, p = 0.02; I2 = 92%) (Fig. 4). However, there was significant heterogeneity among these studies.
Discussion
The main finding of this systematic review and meta-analysis was that UKA patients were less aware of their artificial joint compared to TKA patients in their day-to-day lives. Their forgetting about the artificial knee joint was noted consistently at different follow-up periods ranging from 6 months to 2 years.
Several preoperative variables, such as age, sex, BMI, and the functional score of the patients, can influence the joint awareness [6, 33, 34, 47, 50, 56]. Behrend et al. reported better FJS-12 among older patients who had less demand for daily activities [6, 50]. These patients usually have a complex general health problem that overshadows the minor joint-related ailment. The same study noted excellent outcomes in male patients around 63 years old with lower BMI. Similarly, Peterson et al. and Kennedy et al. also reported better patient-reported outcomes among men [27, 41]. As the women of this age group usually live alone without a partner, they delay the TKA surgery till they have greater joint pain and dysfunction; this was attributed as the primary cause for the more unsatisfactory outcomes in females [19, 38]. Regarding the impact of BMI on joint awareness, Behrend et al. observed a significantly inferior FJS-12 in the younger obese female patients following TKA [6]. Many systematic reviews also found an inferior outcome, higher complication rate, increased cost, and lower survivorship in obese patients after TKA; however, the findings were relevant to BMI of > 40 kg/m2 [16, 43]. None of the studies recruited in this meta-analysis had evaluated this category of patients; hence, selection bias was avoided. The preoperative functional scores in UKA candidates are higher because of lesser preoperative knee pathology and, accordingly, one would expect a better postoperative score. Many previous studies did not control these preoperative variables and encountered a selection bias [32, 34, 50]. Most of the included studies of this review matched their patients in the preoperative period; hence, this minimized the selection bias. Blevin et al. [7] matched their patients in the ratio of 1:1 for age ± 5 years, gender, and BMI ± 3. On analysis of the results, they noted a statistically significant difference in the mean age. However, the mean difference of 2.6 years was clinically irrelevant. Zuiderbaan et al. [56] reported a mean BMI difference of 1.7 kg/m2 between the UKA and TKA groups, but this difference was clinically not significant.
The surgical technique, surgeon’s experience, and prostheses designs are other variables likely to affect the outcome. However, it was not possible to control such confounders in this meta-analysis [54]. We believed that all surgeries were performed in the best possible way with utmost care to execute optimal clinical, functional, and radiological outcome for the patients. There were three studies in this meta-analysis where the UKA surgeries were performed with the assistance of a robot [7, 14, 56]; all the other UKA and TKA surgeries were performed manually. Although robotic-assisted UKA may improve the accuracy of the postoperative alignment and may have better survivorship than manual UKA in the early postoperative period, randomized controlled trials failed to demonstrate a better functional score and patient-reported outcome score in the robotic group in comparison to patients who were manually operated on [8, 20].
Wilson et al. reported better combined patient-reported outcome (PROM) scores in UKA than TKA in a meta-analysis of RCTs, cohort studies, and national joint registries [54]. Thirty-seven postoperative combined PROM scores were evaluated from 29 studies; however, FJS-12 was not evaluated. They found equivocal pain component between the groups. The function scores as evaluated from the national joint registries and cohort studies were significantly better in UKA, but a similar trend was not observed in the analysis of RCTs [54]. Arirachakaran et al. did not find any difference in the knee scores and range of motion (ROM) between UKA and TKA in a meta-analysis of RCTs [3]. They reported an increased (five times) revision rate and lesser early postoperative complications (60% less likely than TKA) in UKA. Several other studies and reviews reported better ROM and cost-effectiveness in UKA than TKA [12, 26, 27, 29, 31, 39, 54]. The advantages of UKA, as reported in these reviews were shorter hospital stay, earlier recovery, reduced complication, and an earlier return to work. The traditional PROM scores, as evaluated in these meta-analyses, show ceiling effect and fail to detect minimal differences among the top scorers or highly active arthroplasty patients [2, 4, 54]. UKA patients are likely to be more active following surgery, and FJS-12 is an appropriate PROM as it has minimal ceiling effects [28, 56].
Behrend, who proposed the FJS-12, reported the mean FJS-12 of 82.5 in healthy individuals who were far below the maximum score of 100 [5]. This observation clarified that the FJS-12 could meticulously distinguish the highly functioning group. Dai et al. reported marked improvement in joint awareness during the first year of UKA [15]; it improved slightly after 2 and 3 years. They observed the lowest FJS-12 at 1 month and the highest at 3 years. The evaluation of FJS-12 at 2 years in this meta-analysis probably accurately revealed the perception of the patients towards the artificial joint. The trend of significantly better FJS-12 in UKA patients was demonstrated at 6 months, 1 year, and 2 years in this meta-analysis. Another notable observation was the marked improvement of FJS-12 in both groups over time. The joint awareness differences in both groups were maximum at 6 months (MD 32.49), and decreased at 1 year (MD 25.62), with a minimal difference at 2 years (MD 7.65). Hiyama et al. reported that the changes in joint awareness with time follow the course of pain and quadriceps strength [24]. FJS-12 is significantly affected by pain in the initial few months following TKA, but quadriceps strength is the main determinant of joint awareness over the long run, especially between 6 and 12 months after surgery [24]. Carlson et al. reported the onset of the plateau of joint awareness at 1 year in a larger cohort of patients [11]. Lesser surgical morbidity, preservation of quadriceps muscle during surgery, and minimal preoperative quadriceps dysfunction because of lesser disease pathology explain the early achievement of a higher FJS-12 in the UKA patients. The TKA patients’ need prolonged time for quadriceps recovery; hence, there was a big difference in FJS-12 at 6 and 12 months, but the difference was minimal at the end of 2 years.
The exact reasons for a more natural feeling of the joint in UKA compared to TKA have not been evaluated. However, minimal bone cut and soft tissue dissections with preservations of cruciate ligaments and quadriceps probably retain the proprioceptive fibers [7, 14, 17, 28, 40, 47, 56]. UKA restores the native pre-degeneration mechanical alignment of the lower limb after surgery; hence, the perception of the natural feeling of the joint persists [49].
There were certain limitations to this meta-analysis. Small sample size, limited studies on this topic, and non-availability of high-quality articles were major shortcomings. The high heterogeneity among the studies was probably because of the differences in patient selection, implant selection, surgical techniques (robotic vs. manual), and the rehabilitation protocol. Also, the psychological aspect of the patients towards the artificial knee joint may vary from patient to patient based on their ethnicity. Among all the studies in this review, a relatively lower FJS-12 score was reported by Kim et al. in the Asian patients [28]. Finally, the joint awareness over the long run in both groups of patients could not be evaluated because of a lack of data. Despite these limitations, the outcome of this meta-analysis has strong clinical relevance. It is well known that patient satisfaction is closely related to joint awareness [1, 14, 28, 51], and there was no firm conclusion about the impact of the type of knee arthroplasty on this specific outcome until now. This meta-analysis revealed a better FJS-12 in the UKA patients than the TKA patients. Based on these findings, it can be recommended that UKA should be widely adopted for medial compartment osteoarthritis of the knee.
Conclusion
To conclude, the joint awareness of UKA patients is less than of TKA. However, the results are limited by the inadequacy of high-quality studies. Well-designed randomized controlled trials with larger sample sizes and longer follow-up periods are needed to interpret the findings with more certainty.
References
Adriani M, Malahias MA, Gu A, Kahlenberg CA, Ast MP, Sculco PK (2020) Determining the validity, reliability, and utility of the forgotten joint score: a systematic review. J Arthroplasty 35(4):1137–1144
Alviar MJ, Olver J, Brand C, Hale T, Khan F (2011) Do patient-reported outcome measures used in assessing outcomes in rehabilitation after hip and knee arthroplasty capture issues relevant to patients? Results of a systematic review and ICF linking process. J Rehabil Med 43(5):374–381
Arirachakaran A, Choowit P, Putananon C, Muangsiri S, Kongtharvonskul J (2015) Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and metaanalysis of randomized controlled trial. Eur J Orthop Surg Traumatol 25(5):799–806
Baker PN, Petheram T, Jameson SS, Avery PJ, Reed MR, Gregg PJ et al (2012) Comparison of patient-reported outcome measures following total and unicondylar knee replacement. J Bone Joint Surg Br 94(7):919–927
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27(3):430-436.e1
Behrend H, Zdravkovic V, Giesinger J, Giesinger K (2016) Factors predicting the forgotten joint score after total knee arthroplasty. J Arthroplasty 31(9):1927–1932
Blevins JL, Carroll KM, Burger JA, Pearle AD, Bostrom MP, Haas SB et al (2020) Postoperative outcomes of total knee arthroplasty compared to unicompartmental knee arthroplasty: a matched comparison. Knee 27(2):565–571
Blyth MJG, Anthony I, Rowe P, Banger MS, MacLean A, Jones B (2017) Robotic arm-assisted versus conventional unicompartmental knee arthroplasty: exploratory secondary analysis of a randomized controlled trial. Bone Joint Res 6(11):631–639
Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP (2001) Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty 16(6):740–747
Burn E, Sanchez-Santos MT, Pandit HG, Hamilton TW, Liddle AD, Murray DW et al (2018) Ten-year patient-reported outcomes following total and minimally invasive unicompartmental knee arthroplasty: a propensity score-matched cohort analysis. Knee Surg Sports Traumatol Arthrosc 26(5):1455–1464
Carlson VR, Post ZD, Orozco FR, Davis DM, Lutz RW, Ong AC (2018) When does the knee feel normal again: a cross-sectional study assessing the forgotten joint score in patients after total knee arthroplasty. J Arthroplasty 33(3):700–703
Casper DS, Fleischman AN, Papas PV, Grossman J, Scuderi GR, Lonner JH (2019) Unicompartmental knee arthroplasty provides significantly greater improvement in function than total knee arthroplasty despite equivalent satisfaction for isolated medial compartment osteoarthritis. J Arthroplasty 34(8):1611–1616
Chawla H, van der List JP, Christ AB, Sobrero MR, Zuiderbaan HA, Pearle AD (2017) Annual revision rates of partial versus total knee arthroplasty: a comparative meta-analysis. Knee 24:179–190
Clement ND, Bell A, Simpson P, Macpherson G, Patton JT, Hamilton DF (2020) Robotic-assisted unicompartmental knee arthroplasty has a greater early functional outcome when compared to manual total knee arthroplasty for isolated medial compartment arthritis. Bone Joint Res 9(1):15–22
Dai YK, Lin W, Yang GM, Lu JF, Wang F (2020) Joint awareness after unicompartmental knee arthroplasty evaluated with the forgotten joint score. Orthop Surg 12(1):218–223
D’Apuzzo MR, Novicoff WM, Browne JA (2015) The John Insall Award: morbid obesity independently impacts complications, mortality, and resource use after TKA. Clin Orthop Relat Res 473(1):57–63
Fabre-Aubrespy M, Ollivier M, Pesenti S, Parratte S, Argenson JN (2016) Unicompartmental knee arthroplasty in patients older than 75 results in better clinical outcomes and similar survivorship compared to total knee arthroplasty A matched controlled study. J Arthroplasty 31(12):2668–2671
Forster-Horváth C, Artz N, Hassaballa MA, Robinson JR, Porteous AJ, Murray JR et al (2016) Survivorship and clinical outcome of the minimally invasive Uniglide medial fixed bearing, all-polyethylene tibia, unicompartmental knee arthroplasty at a mean follow-up of 7.3years. Knee 23:981–986
Gandhi R, Razak F, Davey JR, Rampersaud YR, Mahomed NN (2010) Effect of sex and living arrangement on the timing and outcome of joint replacement surgery. Can J Surg 53(1):37–41
Gilmour A, MacLean AD, Rowe PJ, Banger MS, Donnelly I, Jones BG et al (2018) Robotic-arm-assisted vs conventional unicompartmental knee arthroplasty. The 2-year clinical outcomes of a randomized controlled trial. J Arthroplasty 33(7S):S109–S115
Goyal T, Sethy SS, Paul S, Choudhury AK, Das SL (2020) Good validity and reliability of forgotten joint score-12 in total knee arthroplasty in Hindi language for Indian population. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06124-z
Hamilton TW, Pandit HG, Jenkins C, Mellon SJ, Dodd CAF, Murray DW (2017) Evidence-based indications for mobile-bearing unicompartmental knee arthroplasty in a consecutive cohort of thousand knees. J Arthroplasty 32:1779–1785
Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews of interventions Version 5.0.0. The Cochrane Collaboration. www.cochrane-handbook.org. Accessed 19 Sept 2020
Hiyama Y, Wada O, Nakakita S, Mizuno K (2016) Joint awareness after total knee arthroplasty is affected by pain and quadriceps strength. Orthop Traumatol Surg Res 102(4):435–439
Hutton B, Wolfe D, Moher D, Shamseer L (2017) Reporting guidance considerations from a statistical perspective: overview of tools to enhance the rigour of reporting of randomized trials and systematic reviews. Evid Based Ment Health 20:46–52
Kazarian GS, Lonner JH, Maltenfort MG, Ghomrawi HMK, Chen AF (2018) Cost-effectiveness of surgical and nonsurgical treatments for unicompartmental knee arthritis: a markov model. J Bone Joint Surg Am 100(19):1653–1660
Kennedy DM, Hanna SE, Stratford PW, Wessel J, Gollish JD (2006) Preoperative function and gender predict pattern of functional recovery after hip and knee arthroplasty. J Arthroplasty 21(4):559–566
Kim MS, Koh IJ, Choi YJ, Lee JY, In Y (2017) Differences in patient-reported outcomes between unicompartmental and total knee arthroplasties: a propensity score-matched analysis. J Arthroplasty 32(5):1453–1459
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD (2018) Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc 26(6):1811–1822
Liddle AD, Pandit H, Judge A, Murray DW (2015a) Optimal usage of unicompartmental knee arthroplasty: a study of 41,986 cases from the National Joint Registry for England and Wales. Bone Joint J 97-B:1506–1511
Liddle AD, Pandit H, Judge A, Murray DW (2015b) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint J 97-B(6):793–801
Lygre SH, Espehaug B, Havelin LI, Furnes O (2010) Vollset SE (2010) Pain and function in patients after primary unicompartmental and total knee arthroplasty. J Bone Joint Surg Am 92(18):2890–2897
Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW (2012) Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res 470(1):84–90
Mackie A, Muthumayandi K, Shirley M, Deehan D, Gerrand C (2015) Association between body mass index change and outcome in the first year after total knee arthroplasty. J Arthroplasty 30(2):206–209
Matsumoto M, Baba T, Homma Y, Kobayashi H, Ochi H, Yuasa T et al (2015) Validation study of the forgotten joint score-12 as a universal patient-reported outcome measure. Eur J Orthop Surg Traumatol 25(7):1141–1145
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW (2015) The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Joint J 97-B:1493–1500
Parsley BS, Bertolusso R, Harrington M, Brekke A, Noble PC (2010) Influence of gender on age of treatment with TKA and functional outcome. Clin Orthop Relat Res 468(7):1759–1764
Peersman G, Jak W, Vandenlangenbergh T, Jans C, Cartier P, Fennema P (2014) Cost-effectiveness of unicondylar versus total knee arthroplasty: a Markov model analysis. Knee 21(Suppl 1):S37–S42
Peersman G, Verhaegen J, Favier B (2019) The forgotten joint score in total and unicompartmental knee arthroplasty: a prospective cohort study. Int Orthop 43(12):2739–2745
Petterson SC, Raisis L, Bodenstab A, Snyder-Mackler L (2007) Disease-specific gender differences among total knee arthroplasty candidates. J Bone Joint Surg Am 89(11):2327–2333
Review Manager (RevMan) [Computer program] Version 5.3 (2014) The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen. Accessed 19 Sept 2020
Rodriguez-Merchan EC (2015) Review article: outcome of total knee arthroplasty in obese patients. J Orthop Surg (Hong Kong) 23(1):107–110
Sansone V, Fennema P, Applefield RC, Marchina S, Ronco R, Pascale W et al (2020) Translation, cross-cultural adaptation, and validation of the Italian language forgotten joint score-12 (FJS-12) as an outcome measure for total knee arthroplasty in an Italian population. BMC Musculoskelet Disord 21(1):23
Schmidt FL, Oh IS, Hayes TL (2009) Fixed- versus random-effects models in metaanalysis: model properties and an empirical comparison of differences in results. Br J Math Stat Psychol 62:97–128
Suda AJ, Seeger JB, Bitsch RG, Krueger M, Clarius M (2010) Are patients’ expectations of hip and knee arthroplasty fulfilled? A prospective study of 130 patients. Orthopedics 33(2):76–80
Thienpont E, Opsomer G, Koninckx A, Houssiau F (2014) Joint awareness in different types of knee arthroplasty evaluated with the forgotten joint score. J Arthroplasty 29(1):48–51
Thomsen MG, Latifi R, Kallemose T, Barfod KW, Husted H, Troelsen A (2016) Good validity and reliability of the forgotten joint score in evaluating the outcome of total knee arthroplasty. Acta Orthop 87(3):280–285
Vasso M, Del Regno C, D’Amelio A, Viggiano D, Corona K, Schiavone Panni A (2015) Minor varus alignment provides better results than neutral alignment in medial UKA. Knee 22(2):117–121
Von Keudell A, Sodha S, Collins J, Minas T, Fitz W, Gomoll AH (2014) Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee 21(1):180–184
Wang Z, Deng W, Shao H, Zhou Y, Li H (2020) Forgotten joint score thresholds for forgotten joint status and patient satisfaction after unicompartmental knee arthroplasty in Chinese patients. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.05.010 ((S0883-5403(20)30499-X))
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al (2020) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in metaanalyses. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 19 Sept 2020
Willis-Owen CA, Brust K, Alsop H, Miraldo M, Cobb JP (2009) Unicondylar knee arthroplasty in the UK National Health Service: an analysis of candidacy, outcome and cost efficacy. Knee 16:473–478
Wilson HA, Middleton R, Abram SGF, Smith S, Alvand A, Jackson WF et al (2019) Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and metaanalysis. Br Med J 364:1352
Zlowodzki M, Poolman RW, Kerkhoffs GM, Tornetta P, Bhandari M (2007) International Evidence-Based Orthopedic Surgery Working Group. How to interpret a metaanalysis and judge its value as a guide for clinical practice. Acta Orthop 78(5):598–609
Zuiderbaan HA, van der List JP, Khamaisy S, Nawabi DH, Thein R, Ishmael C et al (2017) Unicompartmental knee arthroplasty versus total knee arthroplasty: which type of artificial joint do patients forget? Knee Surg Sports Traumatol Arthrosc 25(3):681–686
Funding
There was no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no potential conflicts of interest for the research, authorship, or publication of this article.
Ethical approval
This systematic review has been registered in PROSPERO (Regd no.: CRD42020198747). Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tripathy, S.K., Varghese, P., Srinivasan, A. et al. Joint awareness after unicompartmental knee arthroplasty and total knee arthroplasty: a systematic review and meta-analysis of cohort studies. Knee Surg Sports Traumatol Arthrosc 29, 3478–3487 (2021). https://doi.org/10.1007/s00167-020-06327-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06327-4