Abstract
Purpose
Magnetic resonance imaging (MRI) findings of subchondral bone marrow edema (SBME) in osteochondral lesions of the talus (OLT) after arthroscopic microfracture are associated with poor clinical outcomes. However, the relationship between SBME volume change and clinical outcomes has not been analyzed. It was hypothesized that clinical outcomes correlated with SBME volume change and extent of cartilage regeneration in patients with OLT.
Methods
64 patients who underwent arthroscopic microfracture for OLT were followed up for more than 2 years. SBME volume change was measured by comparing preoperative and 2-year follow-up MRI. Clinical outcomes were assessed using the visual analogue scale (VAS) and the American orthopedic foot and ankle society ankle-hindfoot scale (AOFAS) at the 2-year and final follow-up. To compare clinical outcomes, patients were categorized into two groups: decreased SBME (DSBME) group (cases without SBME on either MRI or with a decreased SBME volume between the MRIs) and increased SBME (ISBME) group (cases with new SBME on postoperative MRI or with an increased SBME volume between the MRIs). Additionally, the effects of age, sex, body mass index, symptom duration, OLT size, OLT location, containment/uncontainment, preoperative subchondral cysts, pre- and postoperative SBME volumes, and MRI observation of cartilage repair tissue score on clinical outcomes were analyzed.
Results
The DSBME group included 45 patients, whereas the ISBME group included 19. The mean age was 40.1 ± 17.2 years, and mean follow-up period was 35.7 ± 18.3 months. Preoperative SBME volume was significantly higher in the DSBME group, while the ISBME group had higher volumes at the final follow-up. In both groups, the VAS and AOFAS scores significantly improved at the final follow-up (p < 0.001, < 0.001). The VAS scores were significantly lower in the DSBME group at the 2-year and final follow-up (p = 0.004, 0.011), while the AOFAS scores were significantly higher (p = 0.019, 0.028). Other factors including cartilage regeneration did not affect clinical outcomes.
Conclusion
SBME volume change correlated with clinical outcomes after arthroscopic microfracture for OLT. Clinical outcomes were worse in patients with new postoperative SBME and increased postoperative SBME volume. In patients with an unsatisfactory clinical course that show decreased SBME via postoperative MRI, an extended follow-up in a conservative manner could be considered.
Level of evidence
Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteochondral lesions of the talus (OLT) involve the articular cartilage and subchondral bone, causing deep ankle pain, edema, and stiffness and resulting in impaired daily and sports activities. The treatment of symptomatic OLT depends on the severity and location of the lesion [12]. Of the various surgical treatments, arthroscopic microfracture is the most commonly used for smaller lesions owing to its limited invasiveness, technical simplicity, and cost-effectiveness; moreover, excellent clinical outcomes have been reported [13, 14, 31].
Radiological imaging plays a crucial role in the diagnosis and evaluation of OLT [23, 25]. Simple radiography and computed tomography (CT) can be used to visualize bony components [25]. However, these imaging modalities have a limited efficacy for evaluating the conditions of the cartilage and subchondral bones; therefore, magnetic resonance imaging (MRI) is primarily used for these evaluations [23, 25]. In OLT, subchondral bone marrow edema (SBME) is commonly found on MRI scans preoperatively [6]. Following surgery, SBME volume may decrease or disappear altogether. However, several patients have developed new SBME or the volume of the existing SBME has increased. Although it has been reported that SBME observed on MRI scans after arthroscopic microfracture is associated with poor clinical outcomes [10, 29, 30], the relationship between quantitative changes in SBME volume and clinical outcomes has not been examined. A few studies have reported that the extent of cartilage regeneration is associated with clinical outcomes based on MRI findings after arthroscopic microfracture for OLT [18, 20, 30].
Therefore, this study primarily aimed to analyze the relationship between perioperative MRI changes in SBME volume and clinical outcomes of OLT patients after arthroscopic microfracture. Secondarily, this study aimed to investigate the association of clinical outcomes with several patient factors, including the extent of cartilage regeneration. It was hypothesized that the clinical outcomes correlated with the SBME volume change and the extent of cartilage regeneration in patients with OLT. The results of this study are expected to provide further information on how to identify patients with unsatisfactory clinical course after surgery.
Materials and methods
This study was approved by the institutional review board at the Kyung Hee University Hospital (KHUH 2020-02-003). This case–control study was conducted using data of patients diagnosed with symptomatic OLT who underwent arthroscopic microfracture between February 2013 and June 2017 and were followed up for at least 2 years. Arthroscopic microfracture was indicated for patients with a lesion size < 1.5 cm2 on MRI and for whom nonoperative management for a minimum of 3 months had failed. Only the primary lesion was included. Patients with bipolar (tibial and talus) lesions; those who required concomitant lateral ankle ligament repair; and those who had inflammatory arthropathy, severe malalignment, failed surgical repair, or ankle arthritis were excluded. Patient characteristics and clinical information [age, sex, body mass index (BMI), and symptom duration] were evaluated using a retrospective chart review.
Operative techniques and rehabilitation
One surgeon performed all the arthroscopic microfracture procedures. Arthroscopic microfracture was performed under general or spinal anesthesia with a tourniquet. A non-invasive ankle distractor with a sterile ankle distractor foot strap was used. Meticulous debridement and curettage of the unstable cartilage and fibrous tissues were performed. A microfracture hole was created at 3- to 4-mm intervals with 3-mm depths using an arthroscopic awl. If a subchondral cyst was present, the inside of the cyst was debrided. After microfracture of the cyst wall was performed, no additional procedures, such as bone grafting, were performed. The tourniquet was released to determine appropriate bone bleeding and the presence of marrow fat droplets. For 2 weeks after the operation, a splint was used for immobilization. Active range of motion and weight-bearing was initiated at 2 and 4 weeks after the operation, respectively. The weight bearing was gradually increased from the 4th week after the operation, and if it was possible to bear without pain, full weight bearing was allowed. The patients were not regularly referred to a physiotherapist.
MRI assessments
MRI was performed with the ankle in a neutral position using a 3.0 T-MRI scanner (Achieva®; Philips Medical Systems, Best, The Netherlands) preoperatively and at 2 years after surgery. MRIs were conducted in accordance with the OLT treatment protocol of our hospital. MRI scan sequences and parameters were identical in all patients. For the assessment of SBME, fat-suppressed proton density-weighted sequence images were acquired in the sagittal and coronal section planes. Maximal craniocaudal (CC) and maximal anteroposterior (AP) lengths were measured in the sagittal image, and the maximal width (W) was measured in the coronal image (Fig. 1). The volume of SBME was subsequently determined using the following standard equation for the volume of an ellipsoid: V = 4/3π × (CC/2 × AP/2 × W/2) [5]. OLT size was determined by calculating the surface area (A) with the following ellipse formula based on the maximum diameter measured in the sagittal and coronal images of the preoperative MRI scans: A = abπ = coronal length × sagittal length × 0.79 [8]. The extent of cartilage regeneration after arthroscopic microfracture was assessed on MRI scans using the magnetic resonance observation of cartilage repair tissue (MOCART) score [22]. In all cases, MRI scans were reviewed by a board-certified orthopedic surgeon and a senior musculoskeletal radiologist who were blinded to patient information and clinical outcomes (Fig. 1). An orthopedic surgeon and musculoskeletal radiologist performed all measurements. Measurements were recorded as the mean value measured twice at 4-week intervals. To quantify the proportion of variance, an intraclass correlation coefficient (ICC) was evaluated by examining the inter- and intra-observer reliabilities. All numbers were calculated to the first decimal place.
Volume measurement from a fat-suppressed proton density-weighted MRI scan of the osteochondral lesion of the talus. a Sagittal and b coronal views. The maximum craniocaudal (CC) and anteroposterior (AP) lengths were measured within the sagittal section image, and the maximum width (W) was measured within the coronal image
Association between SBME volume change and clinical outcomes
To examine the relationship between the pre- and postoperative SBME volume change and clinical outcomes, cases were categorized into two groups as follows: (1) the decreased SBME group (DSBME group), which included cases with no SBME on both pre- and postoperative MRI scans or those with a decreased SBME volume postoperatively, and (2) the increased SBME group (ISBME group), which included cases with SBME present in postoperative MRI scans but not in preoperative the MRI scan or those with an increase in SBME volume postoperatively. Clinical outcomes were evaluated using the visual analogue scale (VAS) and American orthopedic foot and ankle society ankle-hindfoot scale (AOFAS) 2 years after the microfracture and at the final follow-up.
Statistical analyses
All statistical analyses were performed using IBM statistical package for social sciences 22.0 (version 22.0; SPSS Inc., an IBM Company, Armonk, NY, USA). A paired t-test was conducted to compare clinical outcomes before and after surgery. The Mann–Whitney U test was used to compare postoperative clinical outcomes between the two groups. When a significant difference was found between the two groups, a post hoc analysis was performed. The Spearman correlation coefficient analysis was performed to evaluate the correlation between other factors and clinical outcomes including: (1) age; (2) sex; (3) BMI; (4) symptom duration; (5) OLT size; (6) OLT location; (7) containment or uncontainment; (8) the preoperative presence of subchondral cysts; (9) preoperative SBME volumes; (10) postoperative SBME volumes; and (11) the MOCART score. p < 0.05 was considered statistically significant for all analyses. The strength of the correlation was described using the following absolute values of r: 0–0.19 was regarded as very weak, 0.20–0.39 as weak, 0.40–0.59 as moderate, 0.60–0.79 as strong, and 0.80–1.00 as very strong. An ICC was assessed by examining the inter- and intra-observer reliabilities to quantify the proportion of variance for the SBME volume measurements, OLT size, and the MOCART score. ICCs were interpreted using a previously established protocol and by referring to Koo et al. methodology [17]. An ICC of < 0.5 indicated a poor agreement, 0.50–0.75 indicated a moderate agreement, 0.75–0.90 indicated a good agreement, and > 0.90 indicated an excellent agreement.
Using the G*power program (version 3.1.9.7), post hoc power analyses with significance levels set to an alpha of 0.05 were performed to determine whether the sample had sufficient power to detect significant differences. A power level of more than 80% was considered sufficient, and all variables that were significantly different met this criterion. Thus, the current number of cases (64) yielded a statistically significant power.
Results
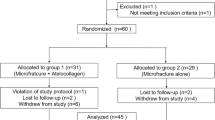
95 cases that underwent microfracture for OLT were identified. Of these 95 cases, five with an OLT size of ≥ 1.5 cm2, five with observed arthritic changes, 17 that had simultaneously undergone an arthroscopic all-inside anterior talofibular ligament repair, and four that did not undergo postoperative MRI, because they were lost to follow-up, were excluded. Thus, a total of 64 patients were included in this study. Patient demographics and clinical data are shown in Table 1.
The mean duration between preoperative MRI and surgery was 26.6 ± 20.5 days (range 1–60 days), and the postoperative MRI was performed, on average, 25.3 ± 2.7 months (range 24–34 months) after surgery. Postoperatively, the mean SBME volume of the total cohort had decreased compared to the preoperative volume (p < 0.001). In four cases, SBME was absent preoperatively but present postoperatively, whereas in 11 cases, SBME was present preoperatively but not postoperatively. The mean MOCART score based on postoperative MRI was 65.1 ± 15.8 points (range 36–105 points). Clinical outcomes significantly improved at the 2-year and final follow-up postoperatively compared to those before surgery. The mean VAS score was 4.4 ± 1.2 preoperatively, 1.1 ± 1.1 at the 2-year follow-up (p < 0.001), and 0.8 ± 1.1 at the final follow-up (p < 0.001). The mean AOFAS score was 71.3 ± 12.2 preoperatively, 93.0 ± 7.4 at the 2-year follow-up (p < 0.001), and 94.2 ± 7.4 at the final follow-up (p < 0.001).
Comparison of clinical outcomes between the DSBME and ISBME groups
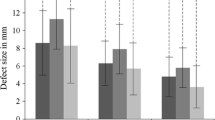
There were no significant differences between the DSBME (n = 45) and ISBME (n = 19) groups in terms of demographic variables, except for sex. The preoperative SBME volume was significantly higher in the DSBME group, and the ISBME group had higher volumes at the final follow-up (Table 1). Improvements in clinical outcomes were significant in both groups. At the 2-year and final follow-ups, the VAS and AOFAS scores of both the DSBME and ISBME groups showed improvement (all p < 0.001). Between-group comparisons of clinical outcomes revealed that at the 2-year and final follow-ups, clinical improvements in the VAS (p = 0.004, p = 0.011, respectively) and AOFAS (p = 0.019, p = 0.028, respectively) scores were significantly greater in the DSBME group than those in the ISBME group (Table 2).
After adjusting for age, sex, BMI, symptom duration, OLT size, OLT location, containment or uncontainment, and the preoperative presence of subchondral cysts for the two groups, multivariate regression models showed that cases with decreased SBME volume had a 1.2 and 0.9-point lower score on the VAS (p = 0.001, p = 0.004) and a 6.7 and 4.2-point higher score on the AOFAS (p = 0.001, p = 0.042) than those with increased SBME volume at the 2-year and final follow-ups, respectively.
Relationship between other factors and clinical outcomes
Age, sex, BMI, symptom duration, OLT size, OLT location, containment or uncontainment, preoperative presence of subchondral cyst, pre- and postoperative SBME volumes, and MOCART score did not significantly affect the VAS score or the AOFAS score (all p, n.s). In particular, neither the pre- nor postoperative SBME volumes correlated with final clinical outcomes. Each item contributing to the MOCART score (filling of defect, integration to border zone, surface of repair tissue, structure of repair tissue, signal intensity of repair tissue, subchondral lamina, subchondral bone and adhesions, and synovitis) did not significantly influenced the VAS or AOFAS scores.
Reliability of BME volume, OLT size, and the MOCART score measurements
Regarding pre- and postoperative SBME volumes, inter-observer reliability was 0.91 and the intra-observer reliabilities were 0.87 and 0.93, indicating good-to-excellent levels of agreement. Regarding the preoperative OLT size, the inter-observer reliability was 0.83 and the intra-observer reliabilities were 0.85 and 0.89. In contrast, the level of agreement of the MOCART score was poor to moderate, with an inter-observer reliability of 0.31 and intra-observer reliabilities of 0.47 and 0.65.
Discussion
The most important finding of the present study was that the clinical improvements in the DSBME group were better than those in the ISBME group. Accordingly, these results strongly supported our hypothesis that SBME volume change after arthroscopic microfracture correlates with OLT clinical outcomes. Secondly, we could not detect a correlation between the extent of cartilage regeneration determined by the MOCART score and clinical outcomes.
Numerous studies have attempted to identify factors related to the outcomes of patients with OLT after arthroscopic microfracture [3, 8, 9, 11, 13, 16, 19, 24]. Clinical outcomes after arthroscopic microfracture for OLT are reportedly associated with the initial OLT size, and poor outcomes are correlated with an initial OLT size of > 1.5 cm2 [3, 8, 9, 24]. Becher et al. [4] showed that BMI had negative effects on clinical outcomes. Shimozono et al. [28] and Choi et al. [7] found that clinical outcomes after arthroscopic microfracture were worse in uncontained OLT lesions than in contained lesions. Moreover, Lee et al. [19] and Jung et al. [16] reported that the presence or absence of subchondral cysts did not influence outcomes after arthroscopic microfracture.
The presence of SBME on MRI scans has been reported as an influential factor in regard to clinical outcomes [10, 29, 30, 34]. Cuttica et al. [10] found that clinical outcomes were poor in the presence of SBME and were worse in patients with moderate or severe SBME signal intensities. Tao et al. [30] concluded that postoperative reduction of SBME could improve clinical outcomes in patients. Shimozono et al. [29] found that the presence of SBME or the SBME grade did not significantly influence clinical outcomes at a 2-year follow-up; however, the clinical outcomes were worse in patients with SBME than in those without at a 4-year follow-up. Additionally, persistent SBME after arthroscopic microfracture was pathological and associated with poor clinical outcomes [2, 29].
Previous reports have mostly indicated that a more severe SBME signal intensity and greater SBME volume on postoperative MRI scans are associated with worse clinical outcomes [10, 29, 30]. However, in the present study, we encountered patients with varying clinical outcomes, despite having similar SBME signal intensities or volumes. In particular, patients with favorable postoperative clinical outcomes, despite having a large postoperative SBME volume, mostly experienced a decrease in SBME volume after surgery, whereas patients with newly observed SBME or postoperative increases in SBME volume had poor clinical outcomes. By comparing clinical outcomes between the groups based on SBME volume at the 2-year and final follow-ups, we confirmed that the DSBME group had significantly better clinical outcomes than the ISBME group. The preoperative SBME volume was significantly different between the two groups. Nevertheless, there was no clinical difference between the two groups. Individually, the SBME volumes on the pre- or postoperative MRIs did not correlate with clinical outcomes through statistical analysis in our study which differed from the findings reported in previous studies [10, 29, 30]. Tao et al. [30] revealed that SBME reduction was associated with improved clinical outcomes, but their analysis was conducted using a different groups of patients at different postoperative time points. We did not use the classification based on the SBME signal intensity by Cuttica et al. [10], because this classification is a subjective grading based on the brightness of the edema signal and thus, was determined to be inappropriate for objective assessment. Clinical outcomes were not affected by patient age, sex, BMI, symptom duration, OLT size and location on MRI scan, containment or uncontainment, or the preoperative presence of subchondral cysts in this study. The preoperative size of OLT, which is associated with clinical outcomes after arthroscopic microfracture [8, 11], did not correlate with clinical outcomes, suspectedly due to the strict inclusion of patients with an OLT size < 1.5 cm2.
The MOCART score is primarily used to evaluate cartilage repair in the knee joint after surgery [1, 21, 22, 33]. Previous studies, however, have reported that the MOCART score does not fully reflect clinical outcomes after arthroscopic microfracture for OLT, unlike that for the knee joint [1, 20, 32]. In this study, the MOCART score did not correlate with postoperative clinical outcomes of OLT and the inter-observer reliability was low. Likewise, Albano et al. [1] reported that inter- and intra-observer agreements for the MOCART score in surgically repaired OLT were not sufficiently reproducible to be applied for postoperative evaluation. Given the low reliability issues with the MOCART score, Schreiner et al. [26] and Shimozono et al. [27] reported on how to compensate for it; however, the literature on this topic is still scarce. Although this study did not correlate MOCART score with clinical results, it was difficult to gain conclusive evidence regarding the correlation between the extent of cartilage regeneration and clinical outcomes due to the aforementioned problems associated with the MOCART score. Additional research is required in this regard. Limitations of this study include its retrospective design, the small study sample, and observation of clinical outcomes during a mid-term follow-up only. Future studies should examine clinical outcomes in a larger number of patients over a longer follow-up period. Additionally, although in this study the SBME volume was measured using MRI conducted at the 2-year follow-up and compared with the SBME volume on preoperative MRI scans, it is necessary to observe the SBME volume change over time by conducting a series of MRI scans at different time points after surgery. More segmented prospective surveys will provide further information on this subject. In addition, while the AOFAS scoring system is widely used, it does not properly reflect the patient’s level of activity and is not fully validated [15]. Thus, occupational characteristics of the patients were not reflected in this study.
Despite these limitations, the strengths of this study are that it is the first study to quantitatively analyze pre- to post-operative SBME volume changes with a medium sized study cohort and the first to demonstrate an association between SBME volume change and clinical outcomes. Clinically, it will be more meaningful to identify a reduction in SBME volume via follow-up MRI rather than the presence of SBME after surgery. When decreased SBME volume is indicated via postoperative follow-up MRI in patients with an unsatisfactory clinical course, an extended follow-up in a conservative manner could be considered.
Conclusion
SBME volume changes correlated with clinical outcomes after arthroscopic microfracture for OLT. Clinical outcomes were worse in patients with new postoperative SBME and increased postoperative SBME volume.
References
Albano D, Martinelli N, Bianchi A, Giacalone A, Sconfienza LM (2017) Evaluation of reproducibility of the MOCART score in patients with osteochondral lesions of the talus repaired using the autologous matrix-induced chondrogenesis technique. Radiol Med 122(12):909–917
Alparslan L, Winalski CS, Boutin RD, Minas T (2001) Postoperative magnetic resonance imaging of articular cartilage repair. Semin Musculoskelet Radiol 5(4):345–363
Amendola A, Panarella L (2009) Osteochondral lesions: medial versus lateral, persistent pain, cartilage restoration options and indications. Foot Ankle Clin 14(2):215–227
Becher C, Driessen A, Hess T, Longo UG, Maffulli N, Thermann H (2010) Microfracture for chondral defects of the talus: maintenance of early results at midterm follow-up. Knee Surg Sports Traumatol Arthrosc 18(5):656–663
Bining HJ, Santos R, Andrews G, Forster BB (2009) Can T2 relaxation values and color maps be used to detect chondral damage utilizing subchondral bone marrow edema as a marker? Skelet Radiol 38(5):459–465
Chan KW, Ferkel RD, Kern B, Chan SS, Applegate GR (2018) Correlation of MRI appearance of autologous chondrocyte implantation in the ankle with clinical outcome. Cartilage 9(1):21–29
Choi WJ, Choi GW, Kim JS, Lee JW (2013) Prognostic significance of the containment and location of osteochondral lesions of the talus: independent adverse outcomes associated with uncontained lesions of the talar shoulder. Am J Sports Med 41(1):126–133
Choi WJ, Park KK, Kim BS, Lee JW (2009) Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med 37(10):1974–1980
Chuckpaiwong B, Berkson EM, Theodore GH (2008) Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy 24(1):106–112
Cuttica DJ, Shockley JA, Hyer CF, Berlet GC (2011) Correlation of MRI edema and clinical outcomes following microfracture of osteochondral lesions of the talus. Foot Ankle Spec 4(5):274–279
Deol PP, Cuttica DJ, Smith WB, Berlet GC (2013) Osteochondral lesions of the talus: size, age, and predictors of outcomes. Foot Ankle Clin 18(1):13–34
Dombrowski ME, Yasui Y, Murawski CD, Fortier LA, Giza E, Haleem AM et al (2018) Conservative management and biological treatment strategies: proceedings of the international consensus meeting on cartilage repair of the ankle. Foot Ankle Int 39(1_suppl):9S–15S
Ferkel RD, Zanotti RM, Komenda GA, Sgaglione NA, Cheng MS, Applegate GR et al (2008) Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med 36(9):1750–1762
Hannon CP, Murawski CD, Fansa AM, Smyth NA, Do H, Kennedy JG (2013) Microfracture for osteochondral lesions of the talus: a systematic review of reporting of outcome data. Am J Sports Med 41(3):689–695
Ibrahim T, Beiri A, Azzabi M, Best AJ, Taylor GJ, Menon DK (2007) Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg 46(2):65–74
Jung HG, Carag JA, Park JY, Kim TH, Moon SG (2011) Role of arthroscopic microfracture for cystic type osteochondral lesions of the talus with radiographic enhanced MRI support. Knee Surg Sports Traumatol Arthrosc 19(5):858–862
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163
Kuni B, Schmitt H, Chloridis D, Ludwig K (2012) Clinical and MRI results after microfracture of osteochondral lesions of the talus. Arch Orthop Trauma Surg 132(12):1765–1771
Lee KB, Park HW, Cho HJ, Seon JK (2015) Comparison of arthroscopic microfracture for osteochondral lesions of the talus with and without subchondral cyst. Am J Sports Med 43(8):1951–1956
Lee KT, Choi YS, Lee YK, Cha SD, Koo HM (2011) Comparison of MRI and arthroscopy in modified MOCART scoring system after autologous chondrocyte implantation for osteochondral lesion of the talus. Orthopedics 34(8):e356–362
Marlovits S, Singer P, Zeller P, Mandl I, Haller J, Trattnig S (2006) Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: determination of interobserver variability and correlation to clinical outcome after 2 years. Eur J Radiol 57(1):16–23
Marlovits S, Striessnig G, Resinger CT, Aldrian SM, Vecsei V, Imhof H et al (2004) Definition of pertinent parameters for the evaluation of articular cartilage repair tissue with high-resolution magnetic resonance imaging. Eur J Radiol 52(3):310–319
Posadzy M, Desimpel J, Vanhoenacker F (2017) Staging of osteochondral lesions of the talus: MRI and cone beam CT. J Belg Soc Radiol 101(Suppl 2):1
Ramponi L, Yasui Y, Murawski CD, Ferkel RD, DiGiovanni CW, Kerkhoffs G et al (2017) Lesion size is a predictor of clinical outcomes after bone marrow stimulation for osteochondral lesions of the talus: a systematic review. Am J Sports Med 45(7):1698–1705
Recht M, White LM, Winalski CS, Miniaci A, Minas T, Parker RD (2003) MR imaging of cartilage repair procedures. Skelet Radiol 32(4):185–200
Schreiner MM, Raudner M, Marlovits S, Bohndorf K, Weber M, Zalaudek M et al (2019) The MOCART (magnetic resonance observation of cartilage repair tissue) 2.0 knee score and atlas. Cartilage. https://doi.org/10.1177/1947603519865308
Shimozono Y, Coale M, Yasui Y, O'Halloran A, Deyer TW, Kennedy JG (2018) Subchondral bone degradation after microfracture for osteochondral lesions of the talus: an MRI analysis. Am J Sports Med 46(3):642–648
Shimozono Y, Donders JCE, Yasui Y, Hurley ET, Deyer TW, Nguyen JT et al (2018) Effect of the containment type on clinical outcomes in osteochondral lesions of the talus treated with autologous osteochondral transplantation. Am J Sports Med 46(9):2096–2102
Shimozono Y, Hurley ET, Yasui Y, Deyer TW, Kennedy JG (2018) The presence and degree of bone marrow edema influence midterm clinical outcomes after microfracture for osteochondral lesions of the talus. Am J Sports Med 46(10):2503–2508
Tao H, Shang X, Lu R, Li H, Hua Y, Feng X et al (2014) Quantitative magnetic resonance imaging (MRI) evaluation of cartilage repair after microfracture (MF) treatment for adult unstable osteochondritis dissecans (OCD) in the ankle: correlations with clinical outcome. Eur Radiol 24(8):1758–1767
Toale J, Shimozono Y, Mulvin C, Dahmen J, Kerkhoffs G, Kennedy JG (2019) Midterm outcomes of bone marrow stimulation for primary osteochondral lesions of the talus: a systematic review. Orthop J Sports Med 7(10):2325967119879127
Weigelt L, Hartmann R, Pfirrmann C, Espinosa N, Wirth SH (2019) Autologous matrix-induced chondrogenesis for osteochondral lesions of the talus: a clinical and radiological 2- to 8-year follow-up study. Am J Sports Med 47(7):1679–1686
Welsch GH, Mamisch TC, Zak L, Blanke M, Olk A, Marlovits S et al (2010) Evaluation of cartilage repair tissue after matrix-associated autologous chondrocyte transplantation using a hyaluronic-based or a collagen-based scaffold with morphological MOCART scoring and biochemical T2 mapping: preliminary results. Am J Sports Med 38(5):934–942
Yasui Y, Ramponi L, Seow D, Hurley ET, Miyamoto W, Shimozono Y et al (2017) Systematic review of bone marrow stimulation for osteochondral lesion of talus - evaluation for level and quality of clinical studies. World J Orthop 8(12):956–963
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This study was approved by the ethical committee of the institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahn, J., Choi, J.G. & Jeong, B.O. Clinical outcomes after arthroscopic microfracture for osteochondral lesions of the talus are better in patients with decreased postoperative subchondral bone marrow edema. Knee Surg Sports Traumatol Arthrosc 29, 1570–1576 (2021). https://doi.org/10.1007/s00167-020-06303-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06303-y