Abstract
Purpose
To determine the incidence of meniscal ramp lesions in an anterior cruciate ligament (ACL) injured knees and to clarify whether ramp lesions are related to chronic ACL deficiency and increased knee instability.
Methods
Consecutive ACL injured patients were evaluated arthroscopically for a ramp lesion via a trans-notch view and evidence of menisco-capsular injury was recorded. Other concomitant injuries to the knee were also noted. Incidence of meniscal ramp lesions, delay before surgery, and anterior–posterior stability was analyzed. All patients underwent bilateral KT-2000 evaluation.
Results
One hundred and three consecutive ACL injured patients with a mean age of 24 years were included in this study. In total, a ramp lesion was found in 10 knees (9.7%) via a trans-notch view. None of these lesions could be identified by the standard view from the anterolateral portal. Other medial meniscal lesions were found in 26 knees (25.2%) by standard arthroscopic viewing. The ramp lesion group had significantly longer delay before surgery with a median of 191 days (p < 0.01) as well as a larger side-to-side difference of KT-2000 measurement (7.3 ± 1.8 mm; p < 0.01), compared with the intact medial meniscus group (53 days and 5.5 ± 1.5 mm, respectively).
Conclusion
Ramp lesions that were identified using a trans-notch view were not visualized with standard arthroscopic views. Increased anterior tibial translation and longer delay before surgery were seen in knees with ramp lesions. Careful inspection of the posteromedial menisco-capsular region is required as hidden menisco-capsular lesions may occur which may result in residual knee instability.
Level of evidence
Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The meniscus plays an important role in shock absorption and biomechanical knee stability [38]. The medial meniscus has a firm attachment to tibial plateau with its roots and meniscotibial ligaments which assists in the control of tibiofemoral laxity at the medial aspect of the knee joint [26, 29, 30, 39]. In anterior cruciate ligament (ACL) deficient knees, the medial meniscus functions as a secondary stabilizer of the knee, restricting anterior tibial translation in response to anterior tibial load [1, 2]. Injuries in the posterior horn of the medial meniscus (PHMM) cause disfunction of this restrictive mechanism and can lead to increased anterior tibial translation in ACL-deficient knees. In the ACL-deficient knee, medial meniscus tears may lead to increased anterior and rotatory instability. These tears often are observed at the posterior and peripheral regions near the posterior joint capsule, especially in chronic cases [12, 20].
Ramp lesions are a tear of the menisco-capsular junction of the PHMM and are commonly associated with ACL deficiency [27]. Because of its posterior location, ramp lesions are commonly overlooked during arthroscopy, if evaluated by standard anterior portal views only. Therefore, these are sometimes referred to as “hidden lesions” by orthopaedic surgeons [32]. Even with magnetic resonance imaging (MRI) examination, ramp lesions are difficult to visualize when compared with medial meniscal body tears [5, 14]. However, it is important to detect meniscal ramp lesions in ACL reconstruction surgery as it has been associated with increased anterior tibial translation and non-physiologic tibial rotation [27, 31]. Accurate detection of meniscal ramp lesions based on correct knowledge of their characteristics would help surgeons to decrease missed injuries and repair these ruptured menisco-capsular junctions with the goal of avoiding residual knee instability and increased stress on the ACL graft [6, 28, 34].
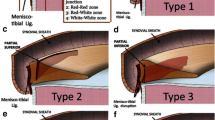
The trans-notch view makes it possible to access the posterior medial compartment relatively easily from the standard anterior portals without creating any additional portals. It allows visualization of the posterior horn, root and posterior menisco-capsular junction (Fig. 1) [33]. Since December 2017, the posteromedial compartment, including the injury of the posterior menisco-capsular junction, has been evaluated prospectively via trans-notch view with every ACL reconstruction surgery in our department.
The purpose of this study was to determine the incidence of meniscal ramp lesions in ACL-injured knees using the trans-notch view and to clarify the characteristics of knees with ramp lesions associated with ACL-deficiency. It was hypothesized that (1) ramp lesions would be commonly observed in ACL injured knees, especially in chronically deficient cases; and (2) they would be associated with increased anterior tibial translation.
Materials and methods
This study was approved by our institutional review board in Kyushu Rosai Hospital (IRB No. 19-17) and all subjects provided informed consent before they were enrolled. One hundred and eleven consecutive ACL injured patients were prospectively recruited from December 2017 to March 2020. Six revision ACL reconstruction cases and two cases with a past history of meniscectomy were excluded. Subsequently, 103 ACL injured knees were included in this study. Fifty-nine were male and 44 were female. The mean age was 24 (range 12–49) years old. During arthroscopic evaluation and before ACL reconstruction, the operative leg was positioned in a leg holder with the knee maintained at 90° of flexion, and the posteromedial compartment was carefully examined by a trans-notch view, as well as by standard views from the anterolateral portal in each case. The arthroscope was passed through the anterolateral portal and inserted between the posterior cruciate ligament (PCL) and the medial wall of the intercondylar notch into the posteromedial compartment and then rotated 90°. When insertion of the arthroscope was not easy, valgus stress was applied to the knee and a blunt obturator was inserted first to feel for its passage. A tear of the menisco-capsular junction of the PHMM was surveyed, separately from other types of medial meniscus lesions such as root tears, horizontal tears, radial tears and vertical tears in white–white or white-red zone. Tear length and depth were estimated using a probe with a scale.
The incidence of meniscal ramp lesions in ACL injured knees was then determined. The incidence of other types of meniscus injuries as identified from standard anterior viewing arthroscopy was evaluated separately. The delay from an initial ACL injury to surgery was also surveyed. Anterior–posterior stability was evaluated pre-operatively with a KT-2000 arthrometer (MED metric Corp, San Diego, California) at 133 N anterior force. The subjective knee function was assessed with the Lysholm scoring scales and KT-2000 measurement was performed at the final follow-up in the ramp lesion group. Results from the KT test and arthroscopy were blinded during data collection and evaluation.
Statistical analysis
The unpaired t test was used to analyze differences of KT-2000 arthrometer measurements between two groups of patients: one with ramp lesions and the other without ramp lesions or any other medial meniscus injuries. The Mann–Whitney U test was used to compare differences in surgical delay from ACL injury to surgery between the two groups. Power analysis was performed on Chi square (significant level = 0.05, power = 0.80, proportion 1 = 10% and proportion 2 = 1%) to indicate sample sizes of 100 could address the questions. The JMP® 9 software program (SAS Institute Inc., Cary, NC) was used for statistical analysis.
Results
Of the 103 cases evaluated, a ramp lesion was found in 10 knees (9.7%). In these 10 knees, menisco-capsular injuries were unable to be visualized with the standard views from anterolateral portal but were identified by the trans-notch view. Other types of medial meniscus lesions were seen in 26 knees (25.2%) and were found using the standard view from anterolateral portal (16 vertical tears, 6 bucket hundle tears, 3 flap tears and 1 radial tear). The delay from injury to surgery was a median of 191 days in the ramp lesion group which was significantly longer than in intact medial meniscus group (median = 53 days, p < 0.01) (Fig. 2a). Mean side-to-side difference of KT-2000 was 7.3 ± 1.8 mm in ramp lesion group and 5.5 ± 1.5 mm in intact medial meniscus group (Fig. 2b), showing larger anterior tibial translation in ramp lesion group (p < 0.01). In other types of medial meniscus lesion cases, the time from injury to surgery was a median of 72 days and mean side-to-side difference of KT-2000 was 6.0 ± 2.0 mm.
a Time from an initial ACL injury to surgery in ramp lesion group and intact medial meniscus group are shown in box and whisker plots. The median values of each group are displayed inside the box as the heavy line. The box is drawn from the first and third quartiles. Whiskers represent the 10th percentile and the 90th percentile. *p < 0.01. b Mean side-to-side difference of KT-2000 in ramp lesion group and intact medial meniscus group are shown
Further characteristics of the 10 cases with ramp lesions and their treatment are presented in Table 1. Overall, long unstable ramp tears were fixed using an all-inside repair device, while short stable tears were left in situ. After an average follow-up of 1.1 years, a mean side-to-side difference of KT-2000 was 0.8 ± 0.7 mm. No catching, locking or giving way sensation was observed in postoperative knees and the last Lysholm score was an average of 97.5 ± 3.5. A case example of a 27 years old male patient with an ACL deficient knee and a ramp lesion is shown in Fig. 3.
A case example of a 27-year-old male patient is shown with a left ACL injury while playing rugby. He previously underwent conservative treatment with functional bracing for 3 months with rehabilitation. He had returned to playing rugby without symptoms but re-injured his left ACL 11 months after his initial injury. a Proton density sagittal MR image shows torn ACL. b T2-weighted sagittal MR image shows high signal intensity change near between the posterior medial meniscus and capsular margin (arrow). c Arthroscopic view from standard antero-lateral portal. No obvious injury to the medial meniscus is seen. d Trans-notch view shows menisco-capsular injury (ramp lesion). The arthroscope was passed between the PCL and the medial wall of the intercondylar notch. e When examined with a probe, the substance of the posterior medial meniscus showed abnormal increased mobility. f The ramp lesion was repaired using a FasT-Fix® (Smith & Nephew Endoscopy) all inside the device. MFC medial femoral codyle, PHMM posterior horn of the medial meniscus, PC posterior capsule, PCL posterior cruciate ligament
Discussion
The most important finding of the present study was that meniscal ramp lesions were found in 9.7% of ACL injured knees upon evaluation with the trans-notch view and were not identified with a careful inspection from the standard anterolateral portal views. Significantly larger anterior–posterior instability was demonstrated in the ACL injured knees with ramp lesions compared to ACL injured knees without meniscal lesions. Ramp lesions were found more frequently in chronic ACL deficient knees with a longer delay from the initial ACL injury to surgical intervention.
Incidence of ramp lesions are reported to be 9% to 24% based on arthroscopic findings in previous studies [5, 8, 9, 19, 21, 31, 33, 42]. One of the reasons for variation in its reported incidence may be relatively low sensitivity of MRI as well as these being missed with standard anterior portal views only. Although some ramp lesions may be detected preoperatively using high-resolution MRI [3, 13], it is not as accurate as a diagnosis for common meniscal body tears [5, 8, 11, 14]. Our group inspected the posteromedial compartment and PHMM directly via trans-notch view as well as the standard views and found an additional 9.7% menisco-capsular injury. This incidence was similar to those (9.3% and 9.6%) reported in previous studies which utilized a trans-notch view [5, 9]. The trans-notch view procedure was technically equivalent to modification of the Gillquist view, but we went through the anterolateral portal and did not penetrate the patellar tendon [10, 18].
The incidence of ramp lesions was higher (16.6–24%) in other studies which created an additional posteromedial portal [19, 21, 31, 33]. The advantage of the trans-notch or Gillquist view is the avoidance of the creation of another portal. The authors believe that if the ramp lesion is substantial, it likely will be able to be perceived with the trans-notch view making the posteromedial portal typically unnecessary. An even higher incidence of ramp lesions (> 30%) was reported in other studies based on MRI findings [4, 17], but not all of those cases with signal changes were confirmed with arthroscopy. Although the incidence of ramp lesions in our study was not as high as the rates reported with an inspection from the posteromedial portal, adding the trans-notch view can help to detect almost 10% of hidden meniscal lesions near the PHMM in those with concomitant ACL injuries that otherwise would be overlooked.
The medial meniscus plays an important role in anterior–posterior stabilization of the knee, especially in the absence of normal ACL function [1, 2, 23]. Loss of this secondary stabilizer in ACL deficient knees can lead to an increase of instability and early onset of osteoarthritis. Even in ACL reconstructed knees, dysfunction of the medial meniscus may increase the ACL graft forces in the early phase of graft healing. This may result in residual knee instability. Recent studies on ramp lesions with concomitant ACL injury reported increased anterior tibial translation or rotatory laxity in vivo [21, 33] and in vitro [34]. Although the medial meniscus is firmly attached to the proximal tibia, disruption of posterior menisco-tibial ligament has been suggested to be associated with increased instability of the posterior horn [27, 36]. Therefore, arthroscopic repair of ramp lesions at the time of ACL reconstruction has been advocated by some researchers [1, 15, 34, 37]. Increased anterior tibial translation was shown in the ramp lesion group in the current study which may result in larger instability in ACL deficient knees. In the current study, meniscal repair was done before the ACL reconstruction if meniscal lesions were long, full-thickness and unstable. As other researchers also have stated, not all ramp lesions may require repair as they are located near the red–red zone with good vascularity. Therefore, shorter and stable tears likely heal conservatively if the knee is stabilized after ACL reconstruction [16, 25, 41]. The authors of the current study agree with this and, therefore, superficial or short tears were not repaired if they were stable upon probing.
The delay from an ACL injury to surgery was significantly longer in the ramp lesion group than in the intact medial meniscus group. This is consistent with recent studies in larger cohorts [19, 33]. In another previous study, posterior menisco-capsular disruption of the medial meniscus was significantly increased in chronic ACL injuries compared with acute injuries, although they did not refer to these as ramp lesions [40]. It was reported in a cadaveric study using a robotic system that the resultant forces on the medial meniscus in response to a combined anterior and axial compressive tibial load were doubled after ACL transection [23]. Although ramp lesion can occur also in acute ACL injury due to high-energy traumas, the increase in the prevalence of medial meniscus injuries with the time from an initial ACL injury may suggest that the instability associated with ACL deficiency is harmful to the medial meniscus [7, 19, 24, 40]. To avoid creation or complications of these meniscal injuries, it is important to diagnose and treat the ACL tear without significant delay after injury. Especially in chronic cases with longer delays before surgery, an occurrence of ramp lesions should be considered during ACL reconstruction and must be evaluated appropriately using a posteromedial portal or a trans-notch view. It is recommended by recent studies that debridement of soft-tissues should be performed to identify possible hidden lesions covered by synovial tissues, using a probe or shaver through a posteromedial portal [6, 9].
One limitation of this study is that the sample size is relatively small. Secondly, the posterior horn of the medial meniscus was inspected via a trans-notch view only and a posteromedial portal was not created. Inspection through the posteromedial portal may perhaps detect more menisco-capsular junction injuries, but this requires more time and is invasive for a screening procedure [22]. The authors consider the trans-notch view as a more efficient way for screening for ramp lesions while creating a posteromedial portal can be considered when a repair of massive tear ramp lesion is required [15]. Third, rotatory stability was not evaluated quantitatively. The pivot-shift test was examined in every case preoperatively but was not quantified [35].
With regard to the clinical relevance, in cases of ACL injuries with substantial instability, or with a longer delay from injury to surgery, consideration of a ramp lesion must occur preoperatively and the posteromedial corner should be inspected intraoperatively. Careful examination for ramp lesions would decrease missed injuries and likely avoid residual instability.
Conclusion
Ramp lesions that were identified using a trans-notch view were not visualized with standard arthroscopic views. Increased anterior tibial translation and longer delay before surgery were seen in knees with ramp lesions. Careful inspection of the posteromedial menisco-capsular region is required as hidden menisco-capsular lesions frequently occur which result in residual knee instability.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- MCL:
-
Medial collateral ligament
- PHMM:
-
Posterior horn of the medial meniscus
- MRI:
-
Magnetic resonance imaging
- PCL:
-
Posterior cruciate ligament
References
Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH (2011) Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligamentdeficient knee significantly influences anterior stability. Am J Sports Med 39:2187–2193
Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SLY (2000) Importance of the medial meniscus in the anterior cruciate ligament deficient knee. J Orthop Res 18:109–115
Arner JW, Herbst E, Burnham JM, Soni A, Naendrup JH, Popchak A, Fu FH, Musahl V (2017) MRI can accurately detect meniscal ramp lesions of the knee. Knee Surg Sports Traumatol Arthrosc 25:3955–3960
Balazs GC, Greditzer HG IV, Wang D, Marom N, Potter HG, Marx RG, Rodeo SA, Williams RJ III (2019) Ramp lesions of the medial meniscus in patients undergoing primary and revision ACL reconstruction: prevalence and risk factors. Orthop J Sports Med 15 7(5):2325967119843509
Bollen SR (2010) Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: a previously unrecognised association. J Bone Jt Surg 92:222–223
Bumberger A, Koller U, Hofbauer M, Tiefenboeck TM, Hajdu S, Windhager R, Waldstein W (2020) Ramp lesions are frequently missed in ACL-deficient knees and should be repaired in case of instability. Knee Surg Sports Traumatol Arthrosc 28:840–854
Church S, Keating JF (2005) Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Jt Surg Br 87:1639–1642
DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, Engebretsen L, LaPrade RF (2017) Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med 45:2233–2237
Di Vico G, Di Donato SL, Balato G, Correra G, D’Addona A, Maffulli N, Rosa D (2018) Correlation between time from injury to surgery and the prevalence of ramp and hidden lesions during anterior cruciate ligament reconstruction: a new diagnostic algorithm. Muscles Ligaments Tendons J 7:491–497
Gillquist J, Hagberg G, Oretorp N (1979) Arthroscopic examination of the posteromedial compartment of the knee joint. Int Orthop 3:13–18
Greif DN, Baraga MG, Rizzo MG, Mohile NV, Silva FD, Fox T, Jose J (2020) MRI appearance of the different meniscal ramp lesion types, with clinical and arthroscopic correlation. Skelet Radiol 49:677–689
Hagino T, Ochiai S, Senga S, Yamashita T, Wako M, Ando T, Haro H (2015) Meniscal tears associated with anterior cruciate ligament injury. Arch Orthop Trauma Surg 135:1701–1706
Hash T (2013) Magnetic resonance imaging of the knee. Sports Health 5:78–107
Hatayama K, Terauchi M, Saito K, Aoki J, Nonaka S, Higuchi H (2018) Magnetic resonance imaging diagnosis of medial meniscal ramp lesions in patients with anterior cruciate ligament injuries. Arthroscopy 34:1631–1637
Hatayama K, Terauchi M, Saito K, Takase R, Higuchi H (2020) Healing status of meniscal ramp lesion affects anterior knee stability after ACL reconstruction. Orthop J Sports Med 8:2325967120917674
Ihara H, Miwa M, Takayanagi K, Nakayama A (1994) Acute torn meniscus combined with acute cruciate ligament injury: second look arthroscopy after 3-month conservative treatment. Clin Orthop Relat Res 307:146–154
Kumar NS, Spencer T, Cote MP, Arciero RA, Edgar C (2018) Is edema at the posterior medial tibial plateau indicative of a ramp lesion? An examination of 307 patients with anterior cruciate ligament reconstruction and medial meniscal tears. Orthop J Sports Med 6:2325967118780089
Lee JY, Chia ZY, Jiang L, Ang B, Chang P (2020) A review of the Gillquist Maneuver: modifications for a safer and easily reproducible approach for knee transintercondylar notch posterior compartment arthroscopy. Arthrosc Tech 9:e435–e438
Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J (2011) Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med 39:832–837
Mariani PP (2011) Posterior horn instability of the medial meniscus a sign of posterior meniscotibial ligament insufficiency. Knee Surg Sports Traumatol Arthrosc 19:1148–1153
Mouton C, Magosch A, Pape D, Hoffmann A, Nuhrenborger C, Seil R (2019) Ramp lesions of the medial meniscus are associated with a higher grade of dynamic rotatory laxity in ACL-injured patients in comparison to patients with an isolated injury. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05579-z
Ogilvie-Harris DJ, Weisleder L (1995) Arthroscopic synovectomy of the knee: is it helpful? J Arthrosc Relat Surg 11:91–95
Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH (2001) The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med 29:226–231
Papastergiou SG, Koukoulias NE, Mikalef P, Ziogas E, Voulgaropoulos H (2007) Meniscal tears in the ACL-deficient knee: correlation between meniscal tears and the timing of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 15:1438–1444
Pierre A, Hulet C, Locker B, Schiltz D, Delbarre JC, Vielpeau C (2001) Outcome of 95 stable meniscal tears left in place after reconstruction of the anterior cruciate ligament. Rev Chir Orthop Reparatrice Appar Mot 87:661–668
Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S (2015) The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc 23:2967–2973
Reider B (2017) Ramped up. Am J Sports Med 45:1001–1003
Robb C, Kempshall P, Getgood A, Standell H, Sprowson A, Thompson P, Spalding T (2015) Meniscal integrity predicts laxity of anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 23:3683–3690
Robinson JR, Bull AM, Thomas RR, Amis AA (2006) The role of the medial collateral ligament and posteromedial capsule in controlling knee laxity. Am J Sports Med 34:1815–1823
Robinson JR, Sanchez-Ballester J, Bull AMJ, de Thomas RW, Amis AA (2004) The posteromedial corner revisited: an anatomical description of the passive restraining structures of the medial aspect of the human knee. J Bone Jt Surg Br 86:674–681
Seil R, Mouton C, Coquay J, Hoffmann A, Nührenbörger C, Pape D, Theisen D (2018) Ramp lesions associated with ACL injuries are more likely to be present in contact injuries and complete ACL tears. Knee Surg Sports Traumatol Arthrosc 26:1080–1085
Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R (2014) Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med 42:921–926
Sonnery-Cottet B, Praz C, Rosenstiel N, Blakeney WG, Ouanezar H, Kandhari V, Vieira TD, Saithna A (2018) Epidemiological evaluation of meniscal ramp lesions in 3214 anterior cruciate ligament-injured knees from the SANTI study group database: a risk factor analysis and study of secondary meniscectomy rates following 769 ramp repairs. Am J Sports Med 46:3189–3197
Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA (2016) Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med 44:400–408
Tashiro Y, Okazaki K, Miura H, Matsuda S, Yasunaga T, Hashizume M, Nakanishi Y, Iwamoto Y (2009) Quantitative assessment of rotatory instability after anterior cruciate ligament reconstruction. Am J Sports Med 37:909–916
Thaunat M, Fayard JM, Guimaraes TM, Jan N, Murphy CG, Sonnery-Cottet B (2016) Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech 5:e871–e875
Thaunat M, Jan N, Fayard JM, Kajetanek C, Murphy CG, Pupim B, Gardon R, Sonnery-Cottet B (2016) Repair of meniscal ramp lesions through a posteromedial portal during anterior cruciate ligament reconstruction: outcome study with a minimum 2-year follow-up. Arthroscopy 32:2269–2277
Walker PS, Erkman MJ (1975) The role of the menisci in force transmission across the knee. Clin Orthop 109:184–192
Warren LF, Marshall JL (1979) The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Jt Surg Am 61:56–62
Woods GW, Chapman DR (1984) Repairable posterior menisco-capsular disruption in anterior cruciate ligament injuries. Am J Sports Med 12:381–385
Yagishita K, Muneta T, Ogiuchi T, Sekiya I, Shinomiya K (2004) Healing potential of meniscal tears without repair in knees with anterior cruciate ligament reconstruction. Am J Sports Med 32:1953–1961
Yeo Y, Ahn JM, Kim H, Kang Y, Lee E, Lee JW, Kang HS (2018) MR evaluation of the meniscal ramp lesion in patients with anterior cruciate ligament tear. Skelet Radiol 47:1683–1689
Author information
Authors and Affiliations
Contributions
YT designed the study, performed surgery, data collection and analysis. He drafted the manuscript. TM also performed surgery, assisted data collection and evaluation. TK assisted designing the study, evaluated the data and co-supervised the clinical aspect of the study. TO assisted data collection, analysis and evaluation. JA advised in a study designed, manuscript preparation, and editing as a native English speaker. FF advised the study design and directed all clinical aspects. He examined the validity of data analysis and supervised the entire research. YI assisted in designing the study and co-supervised the entire research.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
This study was approved by our IRB in Kyushu Rosai Hospital (IRB No. 19–17) and all subjects provided informed consent before they were enrolled.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tashiro, Y., Mori, T., Kawano, T. et al. Meniscal ramp lesions should be considered in anterior cruciate ligament-injured knees, especially with larger instability or longer delay before surgery. Knee Surg Sports Traumatol Arthrosc 28, 3569–3575 (2020). https://doi.org/10.1007/s00167-020-06161-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06161-8