Abstract
Purpose
To report on the outcome and complications of minimal invasive medial unicondylar knee arthroplasty (UKA) after failed prior high tibial osteotomy (HTO) as treatment for medial osteoarthritis in the knee. The hypothesis was that good results can be achieved, if no excessive postoperative valgus alignment and abnormal proximal tibial geometry is present.
Methods
All medial UKAs after failed prior HTO (n = 30), performed between 2010 and 2018 were retrospectively reviewed. The patients were followed for revision surgery and survival of the UKA (defined as revision to TKA). Clinical examination using the Knee Society Score (KSS), Oxford Knee Score (OKS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), as well as radiological examination was performed. Radiographs were studied and the influence of the demographic factors and the radiographic measurements on the survival and the clinical outcome was analysed.
Results
After a follow-up of 4.3 ± 2.6 years (2.1–9.9) 27 UKAs were available. The survival rate was 93.0%. Two UKAs were revised to TKA (excessive valgus alignment and tibial loosening with femoropatellar degeneration). Two further patients had revision surgery (hematoma and lateral meniscus tear). Follow-up clinical and radiological examination was performed in 21 cases: KSS 82.9 ± 10.1 (54.0–100.0), KSS (function) 93.3 ± 9.7 (70.0–100.0); OKS 42.7 ± 6.0 (25.0–48.0); WOMAC 7.9 ± 15.6 (0.0–67.1). No significant influence of demographic factors or radiological measurements on the clinical outcome was present.
Conclusion
Prior HTO is not a contraindication for medial UKA, because good-to-excellent results can be achieved in selected patients with medial osteoarthritis and previous HTO, treated with medial UKA, in a midterm follow-up. Excessive mechanical valgus axis should be avoided; therefore, patient selection and accurate evaluation of medial laxity, preoperative mechanical axis, joint line convergence and proximal tibial geometry are important.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The survival and results for TKA following failed HTO are reported to be equal with higher revision rates compared to primary TKA [4, 6, 16, 19, 26]. Another treatment option is medial UKA, but currently prior high tibial osteotomy (HTO) is seen as contraindication for medial UKA with mobile bearing inlay. This is based on the study of Rees et al. [21] in 2001 who found early failure because of progredient lateral degeneration caused by postoperative valgus alignment in patients, treated with medial UKA for medial osteoarthritis and prior HTO. However, the cohort only consisted of 18 cases and no analysis was performed according to pre- and postoperative alignment and radiographic measurements. So, in contrast to these findings, over 10 years later, Valenzuela et al. [27] reported on good results of medial UKA with a fixed bearing inlay after HTO, similar to that of TKA after HTO and primary medial UKA, because overcorrection into excessive valgus alignment was avoided.
Until today, no further studies on medial UKA after HTO are available, especially none with medial UKA and mobile bearing inlay and analysis of radiological and clinical parameters. There is a lack of knowledge if and under what conditions medial UKA is possible after prior HTO. Therefore, the purpose of the current study is to report on a cohort of minimal invasive medial UKA after prior failed HTO for the treatment of medial osteoarthritis in the knee and to analyse radiological and clinical parameters to help surgeons in the decision if medial UKA is possible and what outcome can be expected in selected patients. The hypothesis was, that good clinical results can be achieved, if no excessive postoperative valgus alignment and abnormal proximal tibial geometry (mechanical Medial Proximal Tibial Angle ≥ 94.0° and ≤ 86.0°) is present.
Materials and methods
The study protocol of this retrospective case series was approved by the competent institutional research ethics board. All patients undergoing UKA in the institution of the authors from 2010 to 2018 (n = 1506) were retrospectively screened for prior HTO at the same leg. A number of 30 medial UKAs, performed after prior failed HTO (persistent medial pain with radiological grade 3–4 osteoarthritis in the medial compartment), with a possible minimum follow-up of 2.0 years were identified in 28 consecutive patients. The medical charts and surgical reports were analysed regarding demographic data, documented preoperative range of motion, type and time of prior osteotomy, type and fixation of UKA and inlay size (Table 1). Furthermore, intra- (fracture, iatrogenic ligament injury, implant malpositioning) and postoperative (infection, thromboembolism, bleeding/hematoma, healing problems, restricted motion) complications were detected.
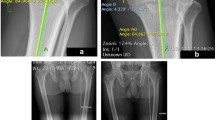
The patients were screened for reoperation and failure of the UKA (defined as revision to TKA). In patients, which were available for examination in the institution clinical and radiological examination was performed. If an appointment could not be made (long distance to the institution), the patients were questioned whether revision surgery was necessary and whether the UKA is still working. Clinical follow-up consisted of Knee Society Score (KSS) (0.0–100.0 points, additionally groups: 100.0–80.0 excellent, 79.0–70.0 good, 69.0–60.0 fair, < 60.0 poor) [11], Oxford Knee Score (OKS) (0.0–48.0 points) [15] and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) (100.0–0.0 points, lower scores indicate better results) [25, 28]. For radiological examination, full weight bearing long leg standing, straight lateral and axial patellar radiographs were taken. Pre- and postoperative radiographs were analysed, with regard to the degree of osteoarthritis according to Kellgren and Lawrence [12], mechanical Femorotibial Angle (mFTA), mechanical Medial Proximal Tibial Angle (mMPTA), mechanical Lateral Distal Femoral Angle (mLDFA), Joint Line Convergence Angle (JLCA) and Proximal Posterior Tibial Slope (PPTS) of the medial plateau, measured according to Amendola [7] (see also Figs. 1, 2) as well as frontal implant position (angle between the femoral and tibial implants and the mechanical axis—a line from the center of the femoral head to the center of the talus, not distinguished between varus or valgus direction). For radiographic measurement the Planning tool mediCAD (Hectec® GmbH, Germany) was used. The radiographs were analysed for progression of osteoarthritis and changes in mFTA, mMPTA, mLDFA and JLCA. The influence of postoperative mFTA on radiological osteoarthritis progression in the lateral compartment was studied.
Full weight bearing long leg standing radiographs (right leg) of one patient preoperative (left) and in the follow-up after implantation of a medial unicompartmental arthroplasty (right) with measurements (mediCAD® (Hectec GmbH, Germany)): mFTA (mFA-mTA) mechanical Femorotibial Angle, mechanical axis of the leg. Angle between a line, drawn from the center of the femoral head to the center of the knee joint and a line, drawn from the center of the ankle joint to the center of the knee joint; mLDFA Mechanical Lateral Distal Femoral Angle. Angle between a line drawn from the center of the femoral head to the center of the knee joint and a line (tangent) drawn from the distal ends of the medial and lateral femoral condyles, measured on the lateral side; JLCA Joint Line Convergence Angle. Angle between a line (tangent), drawn from the distal ends of the medial and lateral femoral condyles and a line (tangent), drawn through the medial and lateral tibial plateau. mMPTA Mechanical Medial Proximal Tibial Angle. Angle between a line, drawn from the center of the ankle joint to the center of the knee joint and a line (tangent), drawn through the medial and lateral tibial plateau, measured on the medial side
Lateral sided radiographs of a right knee preoperative and in the follow-up after implantation of a medial unicompartmental arthroplasty with measurement of Proximal Posterior Tibial Slope (PPTS) of the medial tibial plateau: PPTS: angle between a line orthogonal to the axis of the tibial shaft and a line drawn through the medial tibial plateau, measured to distal
The influence of demographic factors and pre- and postoperative radiographic measurements on the clinical outcome was calculated. Additionally, a post hoc sample size power analysis with an alpha level of 0.05 was performed for every score (gender, power 2.6–20.0%; body mass index (BMI) ≥ 30.0 kg/m2, power 6.2–21.5%; type of prior osteotomy, power 7.7–31.1%; time of less than 5 years between osteotomy and UKA, power 12.2–34.3%; implant fixation, power 2.5–13.8%; inlay size ≥ 5 mm, power 2.4–53.0%; preoperative osteoarthritis ≥ 3 in the patellofemoral (PF) compartment, power 5.6–36.0%; preoperative mMPTA ≥ 94.0°, power 3.2–15.7%; postoperative mMPTA ≥ 94.0° or ≤ 86.0°, power 4.5–11.9%; preoperative mFTA ≥ 2.0° valgus, power 5.4–13.5% and follow-up mFTA ≥ 4.0°, power 4.6–40.7%). For prediction analysis of follow-up mFTA the preoperative mFTA was added to the JLCA (varus angles were subtracted from, and valgus angles were added to JLCA, power 63.9%).
Selection criteria for medial UKA were medial osteoarthritis (grade 3–4 according to Kellgren and Lawrence [12], intact anterior cruciate ligament (ACL) and no flexion contracture or malalignment of more than 15°. Additionally, all patients received magnetic resonance imaging (MRI) to confirm an intact lateral compartment, intact ligament status and to analyse the state of the patellofemoral compartment. The results of the MRI examinations were documented in the medical charts. Not all images of the MRIs were available when performing the study; therefore, further analysis was not possible. As previously reported the state of the patellofemoral compartment does not affect the outcome after medial UKA [24]. So, if not clinically leading with symptoms (anterior knee pain), the state of the patellofemoral compartment was no inclusion criteria (the preoperative radiological status of the patellofemoral compartment is shown in Table 3). All patients were informed, that prior HTO is an exclusion criterion for medial UKA and the possible complications and problems were explained. Because of patient’s request UKA was performed.
Surgical technique for minimal invasive implantation of the Oxford Knee Phase III has previously been described [18, 20]. Medial parapatellar incision was made from the distal pole of the patella to the medial side of the tibial tuberosity. Care was taken to not overstuff the medial compartment and to achieve proper ligament balancing and tension. Fixation of the femoral and tibial components was achieved either with bone cement (n = 13) or later, if good bone quality was present, with cementless fixation (n = 17). In the postoperative rehabilitation immediate full weight bearing with crutches for 2 weeks was allowed. Immediate movement exercises starting from day one after surgery were performed.
Statistical analysis was performed using IBM SPSS Statistics for Windows (version 24, IBM Corp., Armonk, NY, USA). The Chi-square test and Fisher’s exact test were used in evaluation of nominal data. For statistical evaluation of nonparametric data the Mann–Whitney U test was used. A student’s t test was used for parametric data. All reported p values are two-tailed, with an alpha level < 0.05 considered as significant. Unless otherwise stated, descriptive data is presented as mean ± standard deviation (and range).
Results
After a mean follow-up of 4.3 ± 2.6 years (2.1–9.9), 27 of the 30 UKAs were available. The survival rate of this 27 UKAs was 93.0% (n = 25). Two underwent revision to TKA. Other two patients had revision because of hematoma and newly lateral meniscus tear, respectively. Table 2 shows the data of these cases. There were no intraoperative complications and only one postoperative superficial wound infection which could be treated conservatively.
Clinical and radiological examination was possible in 21 cases. Follow-up scores were: KSS 82.9 ± 10.1 (54.0–100.0), KSS excellent 16 cases (76.2%), KSS good 4 cases (19.0%), KSS fair 1 case (4.8%), KSS poor no case, KSS (function) 93.3 ± 9.7 (70.0–100.0); OKS 42.7 ± 6.0 (25.0–48.0); WOMAC 7.9 ± 15.6 (0.0–67.1). The total range of motion improved from 109 ± 12° (90–127) to 121 ± 10° (90–135). The preoperative and follow-up radiological parameters are shown in Table 3. In general, mechanical axis was corrected into valgus direction (1.8 ± 3.4 (− 3.5–7.3)) with reduction of JLCA (2.3 ± 2.4 (− 2.1–6.8)), mMPTA (3.1 ± 2.2 (− 0.6–6.7)), and mLDFA (2.1 ± 2.0 (− 2.0–6.0)). A progression of radiological osteoarthritis in the patellofemoral compartment could be identified in one patient (grade 2–3) and in the lateral compartment in five patients (two grade 0–1, three grade 1–2).
Statistical analysis and influence calculation of the demographic factors and radiographic measurements on the clinical outcome was not reasonably possible, due to the low sample size. As well, analysis of the postoperative mFTA in dependance of preoperative mFTA and JLCA was not reasonably possible.
Discussion
The main finding of the present study is, that medial UKA is possible after prior HTO in selected patients. In a midterm follow-up, good-to-excellent results can be achieved in cases with medial osteoarthritis and prior HTO treated with medial UKA and mobile bearing inlay. However, especially in these patients, accurate preoperative examination regarding radiological alignment, laxity and expected intraarticular correction is important, as there is a risk of early failure because of overcorrection into valgus alignment.
In the present cohort of 27 patients, two patients had early failure of the UKA. In one patient the cause of revision was excessive valgus alignment. This patient showed 4° of valgus alignment, intraarticular medial wear with a JLCA of 4.5° and a proximal tibial geometry of 95.8° of mMPTA in the preoperative radiographs. Thus a valgus overcorrection in this case could have been expected retrospectively. The other patient had failure because of tibial loosening and progredient patellofemoral degeneration. Preoperative radiographs revealed an alignment of 12° varus. To the authors opinion this case was not influenced by the prior osteotomy, performed over 8 years before. The problem of progredient valgus alignment in cases of medial UKA after prior HTO already has been described by Rees et al. [21] in 2001. In their multi center subgroup analysis of 18 patients, treated with medial UKA five (28%) were revised to TKA in a mean follow-up of 5.4 years. In summary three of the five revisions obviously were revised because of valgus alignment. Similar to the findings of the present study one patient had early revision (after 0.92 years) because of excessive valgus of 15°. The other two cases had revision after 4.58 and 5.70 years because of progredient lateral degeneration and pain. The authors, therefore, stated that previous HTO is a contraindication for medial UKA in general. No precise analysis of alignment and radiological measurements was performed in this study. In contrast, Valenzuela et al. [27] reported on good results in their comparative study with radiological and clinical examination and mean follow-up of 6 years. They found similar results between the three groups of UKA after HTO (n = 22), TKA after HTO (n = 19) and primary UKA (n = 22). In the group of UKA after HTO, one revision to TKA because of valgus overcorrection and lateral wear was noted. A radiological analysis of alignment was performed, and no significant differences were found between groups. The mean preoperative mechanical axis was 2.38° varus (8.00° varus–2.00° valgus), whereas in the present study mean preoperative mechanical axis was 0.6° valgus (5.0° varus–6.2° valgus). As a result the postoperative mechanical axis was more varus (0.23 varus (5.00 varus–21.00 valgus)) compared to the present study (2.3 valgus (3.5 varus–9.5 valgus)). Additionally, a fixed bearing UKA was used by Valenzuela et al. So there was no risk of inlay dislocation and some kind of medial laxity could be tolerated to prevent adding too much intraarticular correction to the extraarticular correction of the previous HTO (mechanical axis was corrected under intraoperative fluoroscopic control during UKA implantation [27]), that can result in postoperative mechanical valgus axis and cause progredient lateral degeneration. However, it was highlighted, that previous HTO in general should not be a contraindication for medial UKA.
In the present study 95% (20 from 21 UKAs) showed excellent or good clinical results in the KSS. As well in the KSS (function), WOMAC and OKS after a mean follow-up of 4.3 years with mean Scores of 93.3, 7.9 and 42.7, respectively. Therefore, it can be concluded that comparable results to the findings of Valenzuela et al. [27], were achieved even in a cohort with higher degrees of preoperative valgus axis and with the use of a mobile bearing inlay. According to the present clinical results, the findings are comparable to results of primary medial UKAs [3, 9, 29, 30].
Due to the limited number of cases no reasonable statistical analysis of the impact of epidemiological or radiological factors on the clinical Scores was possible.
In valgus correction osteotomy for the treatment of medial osteoarthritis overcorrection into valgus alignment used to be mandatory; however, nowadays a more individualized approach with less overcorrection is recommended [8, 23]. Therefore, preoperative valgus alignment and abnormal proximal tibial geometry may be present in patients with prior HTO [13]. Furthermore, to decrease the pressure in the medial compartment after medial open wedge HTO, depending on the patient’s medial laxity, a release of the superficial fibers of the medial collateral ligament (MCL) must be performed and as a result an increased medial laxity may be present [2, 5, 17, 22]. Using medial UKA with mobile bearing inlay does not offer the possibility to maintain too much medial laxity because of the risk of inlay dislocation and a thicker inlay may be needed that may result in even more valgus alignment [1, 10, 14]. Although direct influence of postoperative > 4.0° mechanical valgus axis on the outcome of medial UKA in the midterm follow-up could not be confirmed, to the author’s opinion, higher degrees of mechanical valgus axis should be avoided. Due to high variability of medial laxity and, therefore, variability of intraarticular correction during UKA implantation a precise calculation of the postoperative mechanical axis is hardly possible. Based on the present findings the authors recommend precise examination of medial laxity (e.g. additional valgus stress radiographs) and evaluation of mFTA and JLCA in preoperative full weight bearing whole leg standing radiographs to estimate the postoperative mechanical axis. In cases, where excessive postoperative mechanical valgus axis is expected, TKA or, probably in special cases UKA with additional correction osteotomy are further treatment options.
There are several limitations to the present study that have to be acknowledged: First, the retrospective setting. No preoperative Scores are available and like every retrospective study there is a risk for selection bias; however, all consecutive cases that could be identified were included. Second, the low patient number. Factors that may influence the clinical outcome are underpowered and statistical analysis of influence factors is not reasonably possible. But the topic restricts high patient numbers as UKA after HTO is rare as mentioned in previous studies. There are no clinical studies on this topic with more cases included. Furthermore, no study with mobile bearing inlay and radiological analysis is available until today. Third, there is a high variance of follow-up time, and because of the midterm follow-up of in mean 4.3 years, no answer can be given on long-term results. Follow-up of this cohort is ongoing. Fourth, there is no control group of primary UKA or TKA after HTO. However, several studies that report on results of medial UKA are present in the literature for comparison and intention of the present study was not to compare TKA and UKA after HTO, but to report on the outcome, complications and influence factors of UKA as treatment for medial osteoarthritis after prior HTO.
The present study shows, that medial UKA with mobile meniscal bearing is a possible treatment option in selected patients with medial osteoarthritis and prior HTO. If mechanical leg axis, medial laxity and joint line convergence are evaluated exactly, midterm results comparable to primary medial UKA can be achieved. This knowledge helps in the decision for treatment in this group of patients. A statistically significant influence of proximal tibial geometry (mMPTA) and, therefore, joint line orientation on the midterm outcome could not be confirmed, but an influence on the long-term outcome is possible. However, further studies on this topic with higher patient number and longer follow-up are needed. Additionally, when correction osteotomy for medial unicompartmental osteoarthritis is performed, care should be taken to the geometry of the proximal tibia and the distal femur. Excessive overcorrection should be avoided to maintain the possibility for medial UKA if the osteotomy fails.
Conclusion
Prior HTO is not a contraindication for medial UKA, because good-to-excellent results can be achieved in selected patients with medial osteoarthritis and previous HTO, treated with medial UKA, in a midterm follow-up. Excessive mechanical valgus axis should be avoided; therefore, patient selection and accurate evaluation of medial laxity, preoperative mechanical axis, joint line convergence and proximal tibial geometry are important.
References
Bae J-H, Kim JG, Lee S-Y, Lim HC, In Y, Lee S, Ji JH, Lee JH, Kim JM, Kim KI (2020) Epidemiology of bearing dislocations after mobile-bearing unicompartmental knee arthroplasty: multicenter analysis of 67 bearing dislocations. J Arthroplasty 35:265–271
Bagherifard A, Jabalameli M, Mirzaei A, Khodabandeh A, Abedi M, Yahyazadeh H (2020) Retaining the medial collateral ligament in high tibial medial open-wedge osteotomy mostly results in post-operative intra-articular gap reduction. Knee Surg Sports Traumatol Arthrosc 28:1388–1393
Campi S, Pandit HG, Dodd CAF, Murray DW (2017) Cementless fixation in medial unicompartmental knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 25:736–745
Chen X, Yang Z, Li H, Zhu S, Wang Y, Qian W (2020) Higher risk of revision in total knee arthroplasty after high tibial osteotomy: a systematic review and updated meta-analysis. BMC Musculoskelet Disord 21:153
van Egmond N, Hannink G, Janssen D, Vrancken AC, Verdonschot N, van Kampen A (2017) Relaxation of the MCL after an open-wedge high tibial osteotomy results in decreasing contact pressures of the knee over time. Knee Surg Sports Traumatol Arthrosc 25:800–807
El-Galaly A, Nielsen PT, Jensen SL, Kappel A (2018) Prior high tibial osteotomy does not affect the survival of total knee arthroplasties: results from the danish knee arthroplasty registry. J Arthroplasty 33:2131–2135.e1
Faschingbauer M, Sgroi M, Juchems M, Reichel H, Kappe T (2014) Can the tibial slope be measured on lateral knee radiographs? Knee Surg Sports Traumatol Arthrosc 22:3163–3167
Feucht MJ, Minzlaff P, Saier T, Cotic M, Südkamp NP, Niemeyer P, Imhoff AB, Hinterwimmer S (2014) Degree of axis correction in valgus high tibial osteotomy: proposal of an individualised approach. Int Orthop 38:2273–2280
Greco NJ, Lombardi AV, Price AJ, Berend ME, Berend KR (2018) Medial mobile-bearing unicompartmental knee arthroplasty in young patients aged less than or equal to 50 years. J Arthroplasty 33:2435–2439
Heyse TJ, Slane J, Peersman G, Dworschak P, Fuchs-Winkelmann S, Scheys L (2017) Balancing mobile-bearing unicondylar knee arthroplasty in vitro. Knee Surg Sports Traumatol Arthrosc 25:3733–3740
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop 248:13–14
Kohn MD, Sassoon AA, Fernando ND (2016) Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res 474:1886–1893
Lee KM, Chang CB, Park MS, Kang S-B, Kim TK, Chung CY (2015) Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthr Cartil 23:232–238
Lee SY, Bae JH, Kim JG, Jang KM, Shon WY, Kim KW, Lim HC (2014) The influence of surgical factors on dislocation of the meniscal bearing after Oxford medial unicompartmental knee replacement: a case–control study. Bone Jt J 96-B:914–922
Naal FD, Impellizzeri FM, Sieverding M, Loibl M, von Knoch F, Mannion AF, Leunig M, Munzinger U (2009) The 12-item Oxford Knee Score: cross-cultural adaptation into German and assessment of its psychometric properties in patients with osteoarthritis of the knee. Osteoarthr Cartil 17:49–52
Niinimäki T, Eskelinen A, Ohtonen P, Puhto A-P, Mann BS, Leppilahti J (2014) Total knee arthroplasty after high tibial osteotomy: a registry-based case–control study of 1,036 knees. Arch Orthop Trauma Surg 134:73–77
Pape D, Duchow J, Rupp S, Seil R, Kohn D (2006) Partial release of the superficial medial collateral ligament for open-wedge high tibial osteotomy: a human cadaver study evaluating medial joint opening by stress radiography. Knee Surg Sports Traumatol Arthrosc 14:141–148
Price AJ, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW, Oxford Hip, and Knee Group (2001) Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J Arthroplasty 16:970–976
Ramappa M, Anand S, Jennings A (2013) Total knee replacement following high tibial osteotomy versus total knee replacement without high tibial osteotomy: a systematic review and meta analysis. Arch Orthop Trauma Surg 133:1587–1593
Rees JL, Price AJ, Beard DJ, Dodd CAF, Murray DW (2004) Minimally invasive Oxford unicompartmental knee arthroplasty: functional results at 1 year and the effect of surgical inexperience. Knee 11:363–367
Rees JL, Price AJ, Lynskey TG, Svärd UCG, Dodd CAF, Murray DW (2001) Medial unicompartmental arthroplasty after failed high tibial steotomy. J Bone Jt Surg 83-B:1034–1036
Seitz AM, Nelitz M, Ignatius A, Dürselen L (2019) Release of the medial collateral ligament is mandatory in medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 27:2917–2926
Smith JO, Wilson AJ, Thomas NP (2013) Osteotomy around the knee: evolution, principles and results. Knee Surg Sports Traumatol Arthrosc 21:3–22
Song E-K, Park J-K, Park C-H, Kim M-C, Agrawal PR, Seon JK (2016) No difference in anterior knee pain after medial unicompartmental knee arthroplasty in patients with or without patellofemoral osteoarthritis. Knee Surg Sports Traumatol Arthrosc 24:208–213
Stucki G, Meier D, Stucki S, Michel BA, Tyndall AG, Dick W, Theiler R (1996) Evaluation of a German version of WOMAC (Western Ontario and McMaster Universities) Arthrosis Index. Z Rheumatol 55:40–49
Sun X, Wang J, Su Z (2020) A meta-analysis of total knee arthroplasty following high tibial osteotomy versus primary total knee arthroplasty. Arch Orthop Trauma Surg 140:527–535
Valenzuela GA, Jacobson NA, Buzas D, Korecki TD, Valenzuela RG, Teitge RA (2013) Unicompartmental knee replacement after high tibial osteotomy: invalidating a contraindication. Bone Jt J 95-B:1348–1353
Walker LC, Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, Deehan DJ (2018) The WOMAC score can be reliably used to classify patient satisfaction after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:3333–3341
Walker T, Hetto P, Bruckner T, Gotterbarm T, Merle C, Panzram B, Innmann MM, Moradi B (2019) Minimally invasive Oxford unicompartmental knee arthroplasty ensures excellent functional outcome and high survivorship in the long term. Knee Surg Sports Traumatol Arthrosc 27:1658–1664
Zuiderbaan HA, van der List JP, Chawla H, Khamaisy S, Thein R, Pearle AD (2016) Predictors of subjective outcome after medial unicompartmental knee arthroplasty. J Arthroplasty 31:1453–1458
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Investigation performed at Clinic of Joint Replacement, General and Rheumatic Orthopedics, Orthopedic Clinic Markgroeningen, Germany.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schlumberger, M., Oremek, D., Brielmaier, M. et al. Prior high tibial osteotomy is not a contraindication for medial unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 29, 3279–3286 (2021). https://doi.org/10.1007/s00167-020-06149-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06149-4