Abstract
Purpose
To compare the outcomes of anterior cruciate ligament (ACL) reconstruction with those of combined ACL and anterolateral ligament (ALL) reconstruction in ACL-deficient knees. The objective of this study was to improve knowledge regarding the treatment of ACL-deficient knees with combined ACL and ALL reconstruction. Combined ACL and ALL reconstruction has been hypothesized to result in better clinical and functional outcomes than isolated ACL reconstruction (ACLR).
Methods
One-hundred and seven adult male athletes with ACL tears and high-grade pivot shifts were randomized into two groups. Those in group A (n = 54) underwent ACLR, while those in group B (n = 53) underwent combined ACL and ALL reconstruction. The median age was 26 (18–40) and 24 (18–33) years in groups A and B, respectively, and the median follow-up was 60 (55–65) months. Physical examination findings, instrumented knee laxity tested using a KT-1000 arthrometer, and International Knee Documentation Committee Scale (IKDC) scores were used to evaluate the outcomes.
Results
One-hundred and two patients were available for follow-up: 52 in group A and 50 in group B. Postoperatively, the pivot shift was normal in 43 (82.7%) and 48 (96%) patients in groups A and B, respectively (p < 0.001). The median instrumented knee laxity was 2.5 ± 0.7 (1.2–6.1) mm in patients in group A and 1.2 ± 0.7 (1.2–3.2) mm in patients in group B (p < 0.001). Additionally, 44 (84.6%) patients in group A had normal IKDC scores and 3 (5.8%) had nearly normal scores, while 48 (96.0%) patients in group B had normal IKDC scores and 2 (4%) had nearly normal scores (p < 0.001).
Conclusion
Combined ACL and ALL reconstruction, compared with isolated ACLR resulted in favourable clinical and functional outcomes, as demonstrated by decreased rotational instability and instrumented knee laxity, a lower graft rupture rate and better postoperative IKDC scores.
Level of evidence
1.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament reconstruction (ACLR) is currently one of the most common procedures in sports medicine [31, 43]. Despite advancing knowledge of ACL injury and techniques for ACLR, persistent rotational instability and graft rupture remain concerns following this surgery [1, 3, 15, 33, 34, 37, 43]. These undesirable outcomes have directed sports orthopaedic surgeons to seek alternative procedures. During the past few years, the anatomy and function of the anterolateral ligament (ALL) have been described in detail [4, 13, 21, 41, 42]. The ACL is the primary restraint during the anterior drawer test (ADT) at all flexion angles and during internal rotation at flexion angles less than 35°. The ALL is a secondary stabilizer for the ACL, preventing anterior tibial translation and internal rotation, especially at 30°–90° of knee flexion [23, 25]. Since the ALL has also been found to prevent the knee pivot shift phenomenon, injury to this ligament is thought to be responsible for inadequate restoration of rotational knee stability following ACLR [4, 5, 23, 25, 26, 29, 30, 39]. Additionally, in the ACL-deficient knee, the ALL and Kaplan fibres contribute to restraint during the pivot shift and anterior tibial translation [12]. Internal rotation significantly increases with further sectioning of the ALL and Kaplan fibres at flexion angles of 30°–90° and 60°–90°, respectively [12]. Although some authors stated that the ALL is not strong enough to cause a Segond fracture and that other structures such as the iliotibial band (ITB), Kaplan fibres and anterior oblique band (AOB) of the fibular collateral ligament (FCL) are involved, [12, 24] with the understanding of the anatomy of the ALL, biomechanical and radiological tools have been used to determine that a Segond fracture could be bony avulsion of the ALL [4, 5, 10, 12, 23, 25]. The precise pathogenesis of Segond’s fracture has been the subject of debate because of the complexity of the anterolateral ligamentous anatomy. Recently, Claes et al. have reported that Segond’s fracture is actually a bony avulsion of the ALL [4, 5, 12]. ALL injuries have been found in up to 79% of cases of acute ACL injury [6, 30, 42]. Nevertheless, the indications for and outcomes of performing combined ACL and ALL reconstruction surgery to restore normal knee kinematics in ACL- deficient knees are still being explored [36, 38, 46]. Few clinical studies of combined ACL and ALL reconstruction surgery have been performed [17, 29, 37, 38, 46]. Those studies reported better clinical and functional outcomes and a lower graft rupture rate with combined ACL and ALL reconstruction than with isolated ACLR and as well as no specific complications [37]. In this study, the outcomes of ACLR were compared with those of combined ACL and ALL reconstruction in ACL-deficient knees using a comparative, prospective randomized methodology. Combined ACL and ALL reconstruction in comparison with isolated ACLR was hypothesized to result in better clinical and functional outcomes.
Material and methods
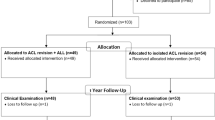
This study was ethically approved by the institutional review board of the Al Razi Orthopaedic Hospital, Ministry of Health, Kuwait and was, therefore, performed in accordance with the ethical standards laid down in the Declaration of Helsinki and amended by the 64th WMA General Assembly, Brazil, 2013. (ID number: RAZI-IRB-2014-08-0001). Oral assent and written consent were obtained from the participants before enrolment in the study. A prospective randomized trial including 107 male athletes with combined ACL and ALL tears was carried out between April 2014 and March 2015. The median follow-up was 60 months, ranging from 55 to 65 months; the median age was 26 (18–40) years and 24 (18–33) years in groups A and B, respectively. The median duration between injury and surgery was 3 months (2.5–3.7) in group A and (2.5–3.8) in group B. Five patients (4.6%) did not complete their follow-up. Out of 102 patients, 42 patients played soccer, 26 played handball, 5 participated in Crossfit, 15 played basketball, 7 played volleyball, 5 played tennis, 1 practised kung-fu, and 1 fenced. In addition to ACL injuries, meniscal injuries were reported in 28 patients (28.4%), 15 (28.8%) in group A and 13 patients (26.0%) in group B, with a total number of 29 injured meniscus 18 medial, and 11 lateral as 1 patient had injured both menisci (Table 1). A preoperative pivot-shift test was carried out under anaesthesia by one surgeon for three positions of rotation: medial, neutral and lateral rotation of the tibia [16, 19, 35]. Nevertheless, the diagnosis of combined ACLs and ALLs tears was based on the findings of three-dimensional magnetic resonance imaging (MRI). Patients with a high-grade pivot shift (III), Segond fracture, a high level of sports activity and those participating in sports involving frequent pivoting were considered to have met the inclusion criteria [5, 17, 25, 37, 38, 46]. Patients with a history of knee surgery, i.e., high tibial osteotomy (HTO), knee dislocation, or preoperative signs of osteoarthritis and those presenting for ACL revision surgery or multiligamentous knee injury, were excluded [26]. Patients were randomized into two treatment groups via simple randomization (flipping a coin) behind closed doors prior to the surgical appointments. Those in group A (n = 54) underwent ACLR, while those in group B (n = 53) underwent combined reconstruction of the ACL and ALL. However, 102 patients were presented for the final analysis (Fig. 1). All surgeries were performed by the same fellowship-trained orthopaedic sports surgeon with the assistance of another orthopaedic surgeon. The postoperative clinical assessments were performed by orthopaedic surgeon who did not participate in the surgeries. The instrumented laxity testing using a KT-1000 arthrometer (MED metric, San Diego, California, USA) [1, 20, 32] was performed by a third surgeon. The functional outcomes of the patients have been assessed using Lysholm knee scoring scale, Tegner activity score and International Knee Documentation Committee Scale (IKDC) score [7].
Surgical technique
Both the gracilis and semitendinosus tendons were harvested. In group A, the gracilis tendon was set aside for possible augmentation if needed, and a standard diagnostic arthroscopy was carried out. The ACL footprints were identified. ACLR was performed by the (all-inside technique) using the semitendinosus tendon. The ACL graft was quadrupled, the graft size ranged from 8 to 11 mm in diameter and 7–7.5 cm in length and was fixed on the tibial and femoral sides using an adjustable suspensory ACL TightRope® RT device (Arthrex, Naples, FL, USA) [44]. Following ACLR (all-inside technique), patients in group B underwent minimally invasive ALL reconstruction. The gracilis graft was doubled; the graft ranged from 4.4 to 5.5 mm in diameter with a total length of 10 cm.The proximal socket of the ALL was made on the lateral femoral condyle just proximal and posterior to the proximal attachment of the lateral collateral ligament [8, 22, 29, 36, 44, 46]. The ALL graft was secured into this socket using a 4.75 mm-diameter bioabsorbable fully threaded knotless anchors (BioComposite SwiveLock®; Arthrex, Naples, FL, USA). The distal attachment of the ALL was marked halfway between the fibular head and Gerdy’s tubercle. After securing the graft in the femoral socket, it was passed underneath the ITB, and the graft was secured into its tibial bone sockets under 0°–15° of flexion. Partial meniscectomy was performed for 15 medial and 8 lateral menisci. The rest of the injuries, however, were repaired using the FasT-Fix technique (Smith and Nephew, Andover, Massachusetts, USA).
Postoperative rehabilitation
Postoperatively, the patients were allowed partial weight bearing as tolerated with crutches. Closed kinetic chain quadriceps exercises were started immediately, while cycling was allowed at the 4th postoperative week. Three months following the surgery, running was allowed. Participation in pivoting sports was not allowed before the 9th postoperative month. Weight-bearing was not allowed in patients who underwent meniscal repair for 4–6 weeks postoperatively and knee flexion was limited to 90°.
Statistical analysis
A statistical power analysis was performed for sample size estimation; the effect size (ES) in this study was 0.55 which was considered to be a medium ES according to Cohen’s (1988) criteria. With alpha = 0.05 and power = 0.8, the projected sample size needed with this ES (G*Power 3.1) was n = 105 ± 2 for this group comparison. The data were analysed using SPSS 17.0 software (SPSS Inc, Chicago, Illinois, USA). Fischer’s exact test was used to study the association between two qualitative variables. Qualitative and quantitative variables were assessed using the Mann–Whitney U test. A p value of < 0.05 was considered the cut-off level for statistical significance.
Results
The clinical outcomes are summarized in Table 2. Although patients in group B showed better postoperative values according to ADT, the results of Lachman’s test were found statistically non significant (n.s). Regarding the postoperative pivot shift, normal results were observed in 43 (82.7%) and 48 (96.0%) patients in group A and group B, respectively (p < 0.001). Moreover, none of the patients in group B had grade II or III pivot shifts, while 5 (9.6%) patients in group A had grade II or III pivot shifts p < 0.001.
Regarding the final result of the treated meniscal injuries all patients were returned to sports activity without any residual complaints.
Table 3 demonstrates the results of the instrumented knee laxity test performed using a KT-1000 arthrometer. Preoperatively, the median translation was 10.2 ± 0.8 (3.8–10.0) mm for group A, and 11.5 ± 0.8 (4.3–10.0) mm for group B (n.s.). Postoperatively, the median translation was 2.5 ± 0.7 (1.2–6.1) mm, and 1.2 ± 0.7 (1.2–3.2) mm for patients in group A and B, respectively (p < 0.001). Five (9.6%) patients in group A had an anterior translation greater than 5 mm, while none of the patients in group B showed such translation p < 0.001. The functional outcomes are presented in Table 4. No statistically significant differences were found in neither the Lysholm knee score nor the Tegner activity score (n.s.) between the two treatment groups postoperatively. Forty-four (84.6%) patients in group A and 48 (96.0%) patients in group B had normal IKDC scores (p < 0.001). Five patients in group A and no patients in group B had IKDC scores of grade C or D. No patients in either groups had immediate postoperative complications that required revision or readmission. Two patients in group B had (type 1) arthrofibrosis that was managed conservatively with an intensive course of physiotherapy, and they achieved full knee range of motion within 4 weeks. Graft failure has been reported in five patients (9.6%) in group A.
Discussion
The most important finding of the present study was that combined ACL and ALL reconstruction can result in favourable clinical and functional outcomes, with no specific complications. This was demonstrated by better postoperative laxity restoration, higher IKDC scores and a lower graft rupture rate. These results were supported by the findings of previously published studies on combined ACL and ALL reconstruction [28,29,30, 36,37,38,39, 46]. In this prospective randomized trial, the outcomes of combined ACL and ALL reconstruction were studied in comparison with those of isolated ACLR in athletes with ACL-deficient knees and high-grade pivot shifts. In the past few decades, many surgical techniques have been developed to improve the functional outcomes of ACLR. Double-bundle reconstruction was found to result in less laxity than single-bundle reconstruction [18, 27]. Despite the excellent outcomes of the available techniques, restoring rotational stability remains a challenge for surgeons [3, 33, 34]. With the addition of lateral extra-articular tenodesis to ACLR, better rotational stability of the knee could be achieved [9, 40, 45]. More recently, attention has been paid to combined ACL and ALL reconstruction [14, 17, 37, 38, 46]. In a case series of 83 patients who underwent combined ACL and ALL reconstruction, significant improvement in clinical and functional outcomes was achieved at a mean follow-up of 32.4 months [38]. The pivot shift test result was normal in 91.6% of these patients and the final IKDC scores were 91.6%. In addition, the mean instrumented anterior knee laxity decreased from 8 to 0.7 mm. At a mean follow-up of 60 months, our results are similar to those of the aforementioned study. In a retrospective study comparing isolated ACLR with combined ACL and ALL reconstruction in patients with chronic ACL tears, the graft rupture rate was reported in 7.3% among the patients treated with isolated ACLR, while there were no cases in the other group [14]. In our study, regarding graft rupture there were five (9.6%) cases in group A and no cases in group B. Similar results were observed in a prospective cohort study that included 502 patients, graft failure rate in the group of patients who underwent combined ALL and ACLR was 2.5–3.1 times less than the rate in the other two ACLR groups (B-PT-B grafts and 4HT grafts) [37]. All these findings support our results and highlight the importance of reconstructing the ALL in appropriate patients with ACL- deficient knees. A prospective randomized trial showed that reconstructing the ALL during ACLR improved the objective and subjective outcomes at a mean follow-up of 27 months [17]. The results of the instrumented knee laxity test were similar to our findings; however, our patients showed significant differences in the pivot shift grade, and IKDC score. Both studies indicate that ALL reconstruction should be considered for specific patients with ruptured ACL. Sectioning the ALL in the ACL-sectioned knee has been found to lead to a mean increases of 3 mm in anterior tibial translation on both anterior stability and simulated pivot-shift testing [2, 30, 39]. Augmented ALL reconstruction with ACLR in a cadaveric setting reduces knee laxity on internal rotation and anterior translation to a level similar to that observed with intact ligaments, except at knee flexion angles between 0° and 20° [28]. When these findings were considered with the improvement in the anterior translation results and the higher percentage of normal results in our patients who underwent combined ACL and ALL reconstruction, the importance of ALL reconstruction cannot be neglected.
A number of limitations do exist in the current study. Unfortunately, due to societal restraints (religious and familial traditions) that can prevent females from participating in competitive sports; very few of females presented with serious related injuries; thus, all our patients were males. Blinding of the patients or surgeons to the surgical technique was not possible unless unnecessary incisions were made in those patients treated with isolated ACLR. The pivot shift test, albeit very useful for the purpose of this study, is subjective and examiner dependent. Although the two sprinter muscles were sacrificed, there were no residual functional deficits or subjective complaints among our patients [11].
Conclusion
Combined ACL and ALL reconstruction, compared with isolated ACLR resulted in favourable clinical and functional outcomes, as demonstrated by decreased rotational instability and instrumented knee laxity, a lower graft rupture rate and better postoperative IKDC scores.
Change history
20 August 2020
A Correction to this paper has been published: https://doi.org/10.1007/s00167-020-06177-0
References
Ayeni OR, Chahal M, Tran MN, Sprague S (2012) Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 20:767–777
Bell KM, Rahnemai-Azar AA, Irarrazaval S et al (2018) In situ force in the anterior cruciate ligament, the lateral collateral ligament, and the anterolateral capsule complex during a simulated pivot shift test. J Orthop Res 36(3):847–853
Chouliaras V, Ristanis S, Moraiti C, Tzimas V, Stergiou N, Georgoulis AD (2009) Anterior cruciate ligament reconstruction with a quadrupled hamstrings tendon autograft does not restore tibial rotation to normative levels during landing from a jump and subsequent pivoting. J Sports Med Phys Fitness 49:64–70
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223:321–328
Claes S, Luyckx T, Vereecke E, Bellemans J (2014) The Segond fracture: a bony injury of the anterolateral ligament of the knee. Arthroscopy 30(11):1475–1482
Claes S, Bartholomeeusen S, Bellemans J (2014) High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg 80(1):45–49
Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM (2011) Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken) 63(Suppl 11):S208–228
Daggett M, Ockuly AC, Cullen M, Busch K, Lutz C, Imbert P, Sonnery-Cottet B (2016) Femoral origin of the anterolateral ligament: an anatomic analysis. Arthroscopy 32(5):835–841
Devitt B, Bell S, Ardern C, Ardern CL et al (2017) The role of lateral extra-articular tenodesis in primary anterior cruciate ligament reconstruction: a systematic review with meta-analysis and best-evidence synthesis. Orthop J Sports Med 5(10):2325967117731767
Ferretti A, Monaco E, Fabbri M, Maestri B, De Carli A (2017) Prevalence and classification of injuries of anterolateral complex in acute anterior cruciate ligament tears. Arthroscopy 33(1):147–154
FU FH, Brown CH Jr, Shelbourne KD, Prodromos C et al (2018) The anterior cruciate ligament: reconstruction and basic science E-book, 2nd edition, chapter 67, P 116.
Geeslin AG, Chahla J, Moatshe G et al (2018) Anterolateral knee extra-articular stabilizers: a robotic sectioning study of the anterolateral ligament and distal Iliotibial Band Kaplan Fibers. Am J Sports Med 46(6):1352–1361
Helito CP, Bonadio MB, Soares TQ, da Mota e Albuquerque RF, Natalino RJ, Pécora JR, Camanho GL, Demange MK (2016) The meniscal insertion of the knee anterolateral ligament. Surg Radiol Anat 38(2):223–228
Helito CP, Camargo DB, Sobrado MF, Bonadio MB, Giglio PN, Pécora JR, Camanho GL, Demange MK (2018) Combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 26(12):3652–3659
Hettrich CM, Dunn WR, Reinke EK et al (2013) The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med 41(7):1534–1540
Huang W, Zhang Y, Yao Z, Ma L (2016) Clinical examination of anterior cruciate ligament rupture: a systematic review and meta-analysis. Acta Orthop Traumatol Turc 50(1):22–31
Ibrahim SA, Shohdy EM, Marwan Y et al (2017) Anatomic reconstruction of the anterior cruciate ligament of the knee with or without reconstruction of the anterolateral ligament: a randomized clinical trial. Am J Sports Med 45(7):1558–1566
Ibrahim SAR, Hamido F, Al Misfer AK, Mahgoob A, Ghafar SA, Alhran H (2009) Anterior cruciate ligament reconstruction using autologous hamstring double bundle graft compared with single bundle procedures. J Bone Joint Surg Br 91(10):1310–1315
Jakob RP, Staubli HU, Deland JT (1987) Grading the pivot shift, objective tests with implications for treatment. J Bone Joint Surg 69-B:69–294
Jonsson T, Althoff B, Peterson L, Renström P (1982) Clinical diagnosis of ruptures of the anterior cruciate ligament: a comparative study of the Lachman test and the anterior drawer sign. Am J Sports Med 10:100–102
Junkin DM Jr (2009) Knee ligament injuries. Orthopaedic knowledge update: sports medicine, 4th edn. American Academy of Orthopaedic Surgeons, Rosemont, pp 135–146
Katakura M, Koga H, Nakamura K, Sekiya I, Muneta T (2017) Effects of different femoral tunnel positions on tension changes in anterolateral ligament reconstruction. Knee Surg Sports Traumatol Arthroc 25(4):1272–1278
Kennedy MI, Claes S, Fuso FA, Williams BT, Goldsmith MT, Turnbull TL, Wijdicks CA, LaPrade RF (2015) The anterolateral ligament: an anatomic, radiographic, and biomechanical analysis. Am J Sports Med 43:1606–1615
Kittl C, El-Daou H, Athwal KK, Gupte CM, Weiler A, Williams A, Amis AA (2016) The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee. Am J Sports Med 44(2):345–354
Kraeutler MJ, Welton KL, Chahla J, LaPrade RF, McCarty EC (2018) Current concepts of the anterolateral ligament of the knee: anatomy, biomechanics, and reconstruction. Am J Sports Med 46(5):1235–1242
Lee DW, Kim JG, Cho SI, Kim DH (2019) Clinical outcomes of isolated revision anterior crucite ligament reconstruction or in combination with anatomic anterolateral ligament reconstruction. Am J Sports Med 47(2):324–333
Meredick RB, Vance KJ, Appleby D, Lubowitz JH (2008) Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med 36(7):1414–1421
Nielsen ET, Olesen KS, Raedt S, Jørgensen B et al (2018) Influence of the anterolateral ligament on knee laxity: a biomechanical cadaveric study measuring knee kinematics in 6 degrees of freedom using dynamic radiostereometric analysis. Orthop J Sports Med 6(8):2325967118789699
Nitri M, Rasmussen MT, Williams BT, Moulton SG, Cruz RS, Dornan GJ, Goldsmith MT, LaPrade RF (2016) An in vitro robotic assessment of the anterolateral ligament, part 2: anterolateral ligament reconstruction combined with anterior cruciate ligament reconstruction. Am J Sports Med 44(3):593–601
Parsons EM, Gee AO, Spiekerman C, Cavanagh PR (2015) The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med 43:669–674
Paschos NK, Howell SM (2017) Anterior cruciate ligament reconstruction: principles of treatment. EFORT Open Rev 1(11):398–408
Pugh L, Mascarenhas R, Arneja S, Chin PY, Leith JM (2009) Current concepts in instrumented knee-laxity testing. Am J Sports Med 37:199–210
Ristanis S, Stergiou N, Patras K, Tsepis E, Moraiti C, Georgoulis AD (2006) Follow-up evaluation 2 years after ACL reconstruction with bone-patellar tendon-bone graft shows that excessive tibial rotation persists. Clin J Sport Med 16:111–116
Ristanis S, Stergiou N, Patras K, Vasiliadis HS, Giakas G, Georgoulis AD (2005) Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy 21:1323–1329
Scholten RJ, Opstelten W, van der Plas CG, Bijl D, Deville WL, Bouter LM (2003) Accuracy of physical diagnostic tests for assessing ruptures of the anterior cruciate ligament: a meta-analysis. J Fam Pract 52(9):689–694
Smith JO, Yasen SK, Lord B, Wilson AJ (2015) Combined anterolateral ligament and anatomic anterior cruciate ligament reconstruction of the knee. Knee Surg Sports Traumatol Arthrosc 23:3151–3156
Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M (2017) Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI Study Group. Am J Sports Med 45(7):1547–1557
Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, Claes (2015) Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med 43(7):1598–1605
Thein R, Boorman-Padgett J, Stone K, Wickiewicz TL, Imhauser CW, Pearle AD (2016) Biomechanical assessment of the anterolateral ligamen of the knee: a secondary restraint in simulated tests of the pivot shift and of anterior stability. J Bone Joint Surg Am 98(11):937–943
Trojani C, Beaufils P, Burdin G et al (2012) Revision ACL reconstruction: influence of a lateral tenodesis. Knee Surg Sports Traumatol Arthrosc 20(8):1565–1570
Van der Watt L, Khan M, Rothrauff BB et al (2015) The structure and function of the anterolateral ligament of the knee: a systematic review. Arthroscopy 31(3):569–82.e3
Van Dyck P, Clockaerts S, Lambrecht V, Wouters K, De Smet E, Gielen JL, Parizel PM (2016) Anterolateral ligament abnormalities in patients with acute anterior cruciate ligament rupture are associated with lateral meniscal and osseous injuries. Eur Radiol 26(10):3383–3391
Wasserstein D, Khoshbin A, Dwyer T, Chahal J, Gandhi R, Mahomed N, Ogilvie-Harris D (2013) Risk factors for recurrent anterior cruciate ligament reconstruction: a population study in Ontario, Canada, with 5-year follow-up. Am J Sports Med 41(9):2099–2107
Wilson AJ, Yasen SK, Nancoo T, Stannard R, Smith JO, Logan JS (2013) Anatomic all-inside anterior cruciate ligament reconstruction using the translateral technique. Arthrosc Tech 2(2):99–104
Zaffagnini S, Signorelli C, Lopomo N, Bonanzinga T, Marcheggiani Muccioli GM, Bignozzi S, Visani A, Marcacci M (2012) Anatomic double-bundle and over-the-top single-bundle with additional extra-articular tenodesis: an in vivo quantitative assessment of knee laxity in two different ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 20:153–159
Zhang H, Qiu M, Zhou A, Zhang J, Jiang D (2016) Anatomic anterolateral ligament reconstruction improves postoperative clinical outcomes combined with anatomic anterior cruciate ligament reconstruction. J Sports Sci Med 15:688–696
Funding
No specific grant from any funding agency in the public, commercial or not for profit sectors.
Author information
Authors and Affiliations
Contributions
FH—The principal investigator. Participated in designing the study, data collection, data interpretation and writing the paper. Performed all the operations. Approved the final version of the manuscript. AAH—Participated in designing the study, data collection, data interpretation, writing the paper and performed all the statistical tests. Approved the final version of the manuscript. YM—Participated in designing the study, data collection, data interpretation, writing the paper and assisting in the operation room. Performed all the statistical tests. Approved the final version of the manuscript. AS—Participated in designing the study, data collection, data interpretation, writing the paper and assisting in the operation room. Approved the final version of the manuscript. TAE—Participated in designing the study, data interpretation and writing the paper. Approved the final version of the manuscript. MGM—Participated in designing the study, data interpretation and writing the paper. Approved the final version of the manuscript. WS—Participated in designing the study, data collection, data interpretation, writing the paper and assisting in the operation room. Approved the final version of the manuscript. AN—Participated in designing the study, data collection, data interpretation, writing the paper and assisting in the operation room. Approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
This research received no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hamido, F., Habiba, A.A., Marwan, Y. et al. Anterolateral ligament reconstruction improves the clinical and functional outcomes of anterior cruciate ligament reconstruction in athletes. Knee Surg Sports Traumatol Arthrosc 29, 1173–1180 (2021). https://doi.org/10.1007/s00167-020-06119-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06119-w