Abstract
Purpose
To investigate changes in meniscal extrusion during knee flexion before and after pullout fixation for medial meniscus posterior root tear (MMPRT) and determine whether these changes correlate with articular cartilage degeneration and short-term clinical outcomes.
Methods
Twenty-two patients (mean age 58.4 ± 8.2 years) diagnosed with type II MMPRT underwent open magnetic resonance imaging preoperatively, 3 months after transtibial fixation and at 12 months after surgery, when second-look arthroscopy was also performed. The medial meniscus medial extrusion (MMME) and the medial meniscus posterior extrusion (MMPE) were measured at knee 10° and 90° flexion at which medial meniscus (MM) posterior translation was also calculated. Articular cartilage degeneration was assessed using International Cartilage Research Society grade at primary surgery and second-look arthroscopy. Clinical evaluations included Knee Injury and Osteoarthritis Outcome Score, International Knee Documentation Committee subjective knee evaluation form, Lysholm score, Tegner activity level scale, and pain visual analogue scale.
Results
MMPE at 10° knee flexion was higher 12 months postoperatively than preoperatively (4.8 ± 1.5 vs. 3.5 ± 1.2, p = 0.01). MMPE at 90° knee flexion and MM posterior translation were smaller 12 months postoperatively than preoperatively (3.5 ± 1.1 vs. 4.6 ± 1.3, 7.2 ± 1.7 vs. 8.9 ± 2.0, p < 0.01). Articular cartilage degeneration of medial femoral condyle correlated with MMME in knee extension (r = 0.5, p = 0.04). All clinical scores significantly improved 12 months postoperatively. However, correlations of all clinical scores against decreased MMPE and increased MMME were not detected.
Conclusions
MMPRT transtibial fixation suppressed the progression of MMPE and cartilage degeneration and progressed MMME minimally in knee flexion position at 1 year. However, in the knee extension position, MMME progressed and correlated with cartilage degeneration of medial femoral condyle. MMPRT transtibial fixation contributes to the dynamic stability of the MM in the knee flexion position.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Many studies have shown that medial meniscus posterior root tears (MMPRTs) are associated with osteoarthritis; 31% of patients with MMPRT undergo subsequent total knee arthroplasty at a mean duration of 30 months after conservative treatment [19]. The medial meniscus (MM) is rigidly attached to the tibia and is, therefore, less mobile, making it more vulnerable to traumatic injuries and degenerative changes than the lateral meniscus [13, 21]. Therefore, loss of hoop strain caused by MMPRT leads to a physiological state equivalent to total meniscectomy and can accelerate the process of degenerative arthritis with meniscal extrusion [1, 4, 7]. To reproduce the hoop tension, several meniscus repair techniques such as transtibial fixation, suture anchor-dependent repair, direct all-inside repair, and posterior reattachment of the MM posterior root have been developed for arthroscopic treatment of MMPRT [4, 6, 16, 21]. Although there is currently a lack of consensus regarding the superior technique, transtibial fixation is increasingly being used in clinical practice because of its lower technical challenges and ability to restore anatomic attachment of the MM posterior root [8, 21]. A meta-analysis on the outcomes of MM posterior root repair in transtibial fixation [4] demonstrated good midterm results after surgery but revealed that MM medial extrusion (MMME) persisted after surgery. Therefore, there is still concern in terms of progression of osteoarthritis or prevention of osteoarthritis following root repair for MMPRT. Therefore, performing MMPRT fixation in elderly patients remains potentially controversial. LaPrade et al. described that MM posterior root repair is indicated in active patients following acute or chronic MMPRT with no significant knee osteoarthritis, joint space narrowing, and malalignment [21]. Chung et al. described that midterm clinical outcomes after transtibial fixation are not age dependent [5]. Despite the progression of MMME, the reason for good clinical results after surgery remains unclear. Therefore, it is necessary to further elucidate the pathological condition, including surgical indications for MM posterior root repair.
MMPRT with a degenerating meniscus is reported in middle-aged or older people due to their lifestyle and behaviours, including frequent squatting and sitting on the floor with folded legs [2]. These behaviours may lead to an increased risk of posterior meniscal segment impingement and injury due to MM posterior root degeneration may occur at low knee flexion angles when performing activities such as descending stairs, stepping, and walking downhill [3, 11]. Additionally, most meniscal tears, including radial tears occurring within 9 mm from the root attachment, are classified as type II in middle-aged and older individuals [17, 21]. Magnetic resonance imaging (MRI) analysis found that MMPRT caused pathological posterior extrusion of the MM at 90° knee flexion [23, 24]. Therefore, the purpose of this study was to investigate pre- and post-operative changes of MMME and MM posterior extrusion (MMPE) in MMPRT patients using open MRI in knee extension and flexion positions and to determine whether these extrusions correlated with cartilage damage and short-term clinical outcomes. We hypothesised that transtibial fixation in MMPRT patients does not suppress the progression of MMME and cartilage degeneration during knee extension but is useful for suppressing the progression of MMPE and cartilage degeneration in knee flexion position.
Even in elderly patients with low healing ability, transtibial fixation of MMPRT can be clinically relevant if improvements in meniscal extrusion and suppression of cartilage degeneration are observed in the knee flexion position. In addition, it might be clinically useful to estimate clinical consequences and treatment strategies for MMPRT for elderly patients.
Materials and methods
This retrospective study was approved by the Institutional Review Board at Okayama University (ID number of the approval: 1857) and informed consent was provided by all patients. All medical records were reviewed retrospectively to obtain patients’ demographic and clinical characteristics from a database at our institution. The medical records of 51 consecutive patients receiving transtibial fixation between March 1, 2016 and October 31, 2017, were reviewed. All patients had an episode of sudden posteromedial painful popping, continuous knee pain, and prolonged pooling of joint fluid [3]. MMPRTs were classified according to the description by LaPrade [20] into five tear types at surgery: type I tears were partially stable meniscal tears within 9 mm from the centre of the root attachment (n = 1), type II tears were complete radial tears within 9 mm from the centre of the root attachment (n = 46), type III tears were bucket-handle tears with meniscal root detachment (n = 0), type IV tears were complex oblique meniscal tears extending into the root attachment (n = 4), and type V tears were avulsion fractures of the meniscal root attachment (n = 0) [20]. The exclusion criteria were (a) more than 70 years old and body mass index (BMI) greater than 30 kg/m2, included varus alignment > 5º, severe cartilage lesion [International Cartilage Research Society (ICRS) grade III or IV], and Kellgren–Lawrence (K–L) grade > II in radiographs. (b) Other than type II MMPRT. Among these 51 patients, 46 were diagnosed with type II MMPRT, under arthroscopic findings. Among the remaining five patients, one was diagnosed with type I MMPRT and four were diagnosed with type IV MMPRT. These five patients were excluded. Among the included 46 patients, 22 underwent open MRI preoperatively, as well as 3 and 12 months after surgery. Second-look arthroscopic evaluation was performed in all cases. This retrospective study analysed the changes in MMME and MMPE after transtibial fixation using open MRI and assessed cartilage degeneration using arthroscopic images and video recordings. We reviewed the patients’ medical records to determine age, sex, height, body weight, BMI, as well as preoperative and 3-month and 12-month postoperative clinical outcomes. The patient demographics are summarised in Table 1.
Arthroscopic assessment of the cartilage lesions and anterior cruciate ligament (ACL) were performed using arthroscopic images and video recordings. Evaluation of the cartilage and its documentation were carried out using the same ICRS articular cartilage lesion classification system at primary surgery and second-look arthroscopy. Articular surfaces on the medial femoral condyle (MFC) and lateral femoral condyle (LFC) were divided into nine segments (MF 1–9, LF 1–9). The medial tibial plateau (MTP) and lateral tibial plateau (LTP) were both divided into five segments (MT 1–5, LT 1–5). The trochlea was divided into three segments (T 1–3) and the patella was divided into nine segments (P 1–9) (Fig. 1). The ACL was evaluated using synovial coverage grade at primary surgery and at second-look arthroscopy.
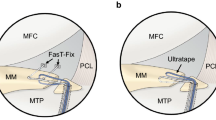
Surgical indications of MMPRT repair in patients under 70 years and a BMI less than 30 kg/m2 included varus alignment < 5º, mild cartilage lesion (ICRS low grade I or II) and K–L grade 0–II in radiographs. Patients were treated with a modified transtibial suture technique combined with FasT-Fix® (Smith & Nephew, Andover, MA, USA) after creating the tibial bone tunnel with an MMPRT guide, as previously described [7, 10, 18]. No. 2 Ultrabraid (or Ultratape) and FasT-Fix 360 reverse curve (Smith & Nephew) were used to stabilize the MM posterior horn in the modified Mason–Allen suture configuration (Fig. 2a–c) [7, 8, 10]. In cases with a tight medial compartment, we used the outside-in pie-crusting technique of the medial collateral ligament with a standard 18-gauge hollow needle (TERUMO, Tokyo, Japan) [28]. An MMPRT aiming guide (Smith & Nephew) was placed at the anatomic insertion of the MM posterior root [9]. A 2.4-mm guide pin was inserted at a 55° angle to the articular surface and a tibial tunnel was created with a 4.5-mm cannulated drill [18]. The Ultrabraid and/or uncut free end of the FasT-Fix sutures were retrieved through the tibial tunnel (Fig. 2d, e). Tibial fixation of the sutures was performed using double-spike plate and screw (Meira, Aichi, Japan) at 45° of knee flexion with an initial tension of 20 N [7, 8, 18].
Modified transtibial suture technique combined with FasT-Fix fixation. a Ultratape was passed through the posterior horn of the MM with the Knee Scorpion suture passer. b The first implant of FasT-Fix was inserted into the posterior horn of the MM, whereas the passed Ultratape was tensioned throughout the anterolateral portal. c The second implant of FasT-Fix was inserted into the posterior root of the MM across the Ultratape. d Modified transtibial suture technique combined with FasT-Fix fixation. e Schematic drawing of the modified transtibial suture technique combined with FasT-Fix fixation. The uncut free ends of the FasT-Fix suture and/or Ultratape were retrieved from the tibial tunnel at an anatomic attachment of the MM posterior root. Note that the FasT-Fix needle penetrated the meniscal horn and posterior joint capsule
The postoperative rehabilitation protocol was similar for all patients. All patients were initially kept non-weight bearing in the knee immobilizer for 2 weeks after surgery. Knee flexion exercises were limited to 90° for the first 4 weeks. The patients were allowed full weight bearing and 120° knee flexion after 6 weeks. Deep knee flexion was permitted 3 months postoperatively [7].
Open MRI scanning was performed in the supine and recumbent positions preoperatively and at 3 months and 12 months postoperatively using an Oasis 1.2 T (Hitachi Medical, Chiba, Japan) with a coil in the 10° (Fig. 3a) and 90° (Fig. 3b) knee-flexed positions under non-weight-bearing conditions. Standard sequences of the Oasis included a sagittal proton density-weighted sequence [repetition time (TR)/echo time (TE), 1718/12], using a driven equilibrium pulse with a 90° flip angle and coronal T2-weighted multi-echo sequence (TR/TE, 4600/84) with a 90° flip angle. The slice thickness was 4 mm with a 0-mm gap. The field of view was 16 cm with an acquisition matrix size of 320 (phase) × 416 (frequency) [23]. MM measurements were performed using a simple MRI-based meniscal sizing technique on the sagittal and coronal views at knee flexion angles of 10° and 90°.
MRI-based measurements: 10° and 90° knee-flexed position in a non-weight-bearing condition (a, b). Coronal and sagittal images of the knee flexed at 10° (c, e) and 90° (d, f). The MMME was measured as the distance from the medial edge of the tibial plateau cartilage to the medial border of the MM. The MMPE was measured as the distance from the posterior edge of the tibia to the posterior edge of the MM. MMME measurements were obtained in the mid-coronal plane by linking the coronal and sagittal image series and MMPE measurements were obtained passing orthogonally through the medial plateau. Medial and posterior margins of the MTP (solid lines) and MM (dashed lines). MMME medial meniscus medial extrusion, MMPE medial meniscus posterior extrusion
The MMME was measured from the medial margin of the tibial plateau (excluding osteophytes) to the outer border of the MM on the coronal MR image that crossed the midpoint of the anteroposterior length of the MM (Fig. 3c, d) [14]. The details of the MMPE measurements were determined from a previously described method. MMPE was measured using a line passing orthogonally through the MTP, which is the distance from the posterior edge of the tibia (excluding osteophytes) to the posterior edge of the MM (Fig. 3e, f). Using the posterior edge of the tibia as the standard, extrusions toward the posterior from the tibial edge represented a positive value, whereas a negative value was defined as the absence of such extrusions. Two orthopaedic surgeons (S.M. and Yu.O.) independently measured the MM extrusion in a blinded manner. MRI measurements were completed by two independent orthopaedic surgeons to determine inter-observer reliability using the intra-class correlation coefficient (ICC). Each observer repeated the measurements at a 4-week interval to determine intra-observer reliability.
Clinical outcomes were assessed preoperatively and at the 3-month, 6-month, and 12-month follow-ups after the surgery using the Knee Injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee (IKDC) subjective knee evaluation form, Lysholm score, Tegner activity level scale, and visual analogue scale (VAS) as indicators of pain score. Preoperative results were compared with the 3-month, 6-month, and 12-month follow-up results. The KOOS consists of five subscales: pain, symptoms, activities of daily living (ADL), sport and recreation function (sport/rec) and knee-related quality of life (QOL) outcomes.
Statistical analyses were performed using EZR software (Saitama Medical Center, Jichi Medical University, Tochigi, Japan). Data are expressed as mean ± standard deviation (SD), unless otherwise indicated. Statistical significance was set at p < 0.05. The repeated measure analysis of variance (ANOVA) was used to compare the preoperative and postoperative clinical scores. One-way ANOVA with Dunnett’s multiple comparison post hoc test was used to compare the preoperative and postoperative MRI data. The averages of these measurements were used in analysis. Differences in cartilage degeneration between primary and second-look arthroscopy were determined using the Wilcoxon signed-rank test. The Spearman’s rank correlation was calculated to assess the correlation between MMME and MM posterior translation and the area with significant change in cartilage degeneration. Linear regression analysis was used to assess the correlation of all clinical scores at 12 months with MMPE (knee flexion angles of 10° and 90°) and MMME (knee flexion angles of 10° and 90°). The sample size was estimated for a minimal statistical power of 80% (α = 0.05). Assuming a one-tailed testing, an alpha of 0.05 and an independent sample t test, a sample of 21 patients was sufficient to detect an effect size of d = 0.5 with 80% statistical power.
Results
Table 1 shows the clinical characteristics of type II MMPRT patients. All clinical scores significantly improved at 12 months postoperatively (p < 0.05, Fig. 4). MMME at 10° knee flexion was higher 12 months postoperatively than preoperatively (4.8 ± 1.5 vs. 3.5 ± 1.2, p = 0.01). On the other hand, MMPE at 90° knee flexion and MM posterior translation were smaller 12 months postoperatively than preoperatively (3.5 ± 1.1 vs. 4.6 ± 1.3, 7.2 ± 1.7 vs. 8.9 ± 2.0, p < 0.01) (Table 2). Significant differences in the area of cartilage degeneration were observed between primary surgery and second-look arthroscopy at the MFC (MF1–4), MTP (MT2), patella (P5), and trochlear (T2) (Tables 3, 4, 5). Articular cartilage degeneration of MFC correlated with MMME in knee extension (r = 0.5, p = 0.04) (Table 6). At the primary surgery, the ACL synovial coverage grade was A in all cases. However, at the second-look arthroscopy, ACL degeneration (synovial coverage grade B) was observed in one patient. Regarding measurements of MMME, the ICCs for intra-observer repeatability and inter-observer repeatability ranged between 0.82 and 0.87, and 0.87 and 0.90, respectively. For MMPE measurements, the ICCs for intra-observer repeatability and inter-observer repeatability ranged between 0.89 and 0.92, and 0.92 and 0.95, respectively. Correlations of all clinical scores with decreased MMPE and increased MMME were not detected.
Time-dependent clinical outcomes. Data were collected preoperatively and at 3-, 6-, and 12-month follow-ups. All scores were significantly improved at the 12-month follow-up after surgery. KOOS Knee Injury and Osteoarthritis Outcome Score, ADL activities of daily living, Sport/Rec sport and recreation function, QOL quality of life, IKDC International Knee Documentation Committee subjective knee evaluation form, VAS visual analogue scale. *p < 0.05
Discussion
There were three main findings from the present study. First, in type II MMPRT patients, MMPE at 90° knee flexion and MM posterior translation during knee flexion decreased after performing the modified transtibial suture technique combined with FasT-Fix fixation. In addition, suppression of cartilage degeneration was observed in the area of MFC from the middle to the posterior end of the site. Second, MMME at 90° knee flexion did not progress greatly, but did progress at the knee extension position. In addition, progression of partial cartilage degeneration was observed especially at the anteromedial site of MFC and this cartilage degeneration correlated with MMME in the knee extension position. Third, meniscus extrusion did not affect all clinical scores at the 12-month postoperative follow-up.
A biomechanical study that mimicked MMPRT type II (complete radial tear within 9 mm from root attachment) reported a significant reduction in the medial compartment contact area except for the extension knee position. At a knee flexion of 90°, the contact area of the medial compartment decreased by about 40%, while the contact pressure increased by about 70% [25]. Similar results were reported in another biomechanical study. The pathologically decreased contact area and increased contact pressure with a flexed knee were restored by transtibial fixation to the same extent as the intact knee [1]. The results of these biomechanical studies aligned with the results of our study, which indicated that improved MMPE and suppression of cartilage degeneration in the area of MFC from the middle to the posterior end of the site (MF5–9) led to restoration of meniscal hoop tension with the knee in a flexed position. In contrast to the good results reported in biomechanical studies, some reports have demonstrated cartilage degeneration and MMME progression on postoperative MRI and second-look examinations, regardless of good clinical outcomes [8, 22]. Similar to these results, our study demonstrated that despite MMME progression in the knee extension position and partial cartilage degeneration (especially anteromedial site of MFC cartilage), all clinical outcomes were improved. In addition, MMME in knee extension position and cartilage degeneration of area MF4 showed a moderate correlation. Hasegawa et al. reported that the strongest correlation between ACL and cartilage degeneration was found at the MFC [12]. In this study, we checked the ACL condition using arthroscopic images and video recordings. We could not detect obvious degenerative changes at the primary surgery, but at the second-look arthroscopy, ACL degeneration was observed in one patient. Thus, worsening MFC cartilage degeneration in this study may influence the ACL degeneration. Therefore, additional surgical procedures that can improve MMME in the knee extension position may prevent MFC and ACL degeneration.
In normal knees, the convex femoral condyle slides and rolls on the tibial plateau with knee flexion, and inevitably pushes the meniscus to move backward. During flexion, the meniscus moves backward and the anteroposterior diameter gradually decreases. The tibiofemoral contact area gradually decreases during flexion because of the large curvature radius at the femoral condyle top and the reduced rearward radius [15]. In the present study, MMME was smaller in the knee flexion position (3.3 mm) than in the knee extension position (4.8 mm). This result may be influenced by the change of curvature radius at the femoral condyle during knee flexion.
If the ACL and posterior cruciate ligament are normal at 90° knee flexion, anterior translation of the tibia is counteracted by the buttress effect of the MM [3]. This highlights the role of MM as a secondary stabilizer in knee flexion. In MRI analysis for MMPRT, the posterior translation of MM is 8.6 mm at 90° knee flexion [23]. In addition, the preoperative amount of posterior translation of the MM in MMPRT was very similar (8.9 mm). The amount of posterior translation of the MM after MMPRT repair improved to 7.2 mm, but the amount of posterior translation was about 2–3 mm more than that of a normal meniscus (4–5 mm) [27, 29]. It was unclear how this difference affected the kinematics (pathological MM translation and rotation of the tibia) in the knee joint. However, MMPRT in elderly patients, which has been considered difficult to repair due to degenerating meniscal tissue and poor healing ability, showed improved MMPE and amount of posterior translation induced by transtibial fixation.
This study did not evaluate MM extrusion (MMME/MMPE) under weight-bearing condition. The degree of MM extrusion (MMME) is significantly different between loaded and unloaded MRI in those with no osteoarthritis or minimal osteoarthritis [26]. On the other hand, the posterior segment of MM is strongly connected to the posterior joint capsule and the semi-membranous muscle [6]. Since the tension of these structures is increased in the loaded knee extension position, the influence on the MM posterior translation may be small. However, the posterior translation of MM in the loaded knee flexion position is unclear. Thus, further research using ultrasonography that can be applied clinically is required in future studies.
There were several limitations to this study. First, patient records were retrospectively assessed, the sample size was small, and the follow-up period was 1 year. Second, this study focused on type II MMPRTs; therefore, other tear patterns could not be evaluated. Third, this study did not evaluate MM extrusion (MMME/MMPE) under weight-bearing condition. Fourth, there was no video recording or image for evaluating posterior cruciate ligament, and there was no description of the posterior drawer test in the medical record, so detailed evaluation was not possible. Fifth, since MRI was two dimensional and did not include axial images, movement of the three-dimensional meniscus was not reflected in the analysis. Morphological analysis of the meniscus should be attempted using three-dimensional MRIs during knee flexion. Future studies should also include more patients with other types of tears and a longer follow-up period.
With regard to clinical relevance, MMPRT transtibial fixation will likely contribute to the dynamic stability of the MM in the knee flexion position. In daily clinical work, MMPRT transtibial fixation should be considered as an effective treatment for MMPRT even in middle-aged and elderly patients.
Conclusions
MMPRT transtibial fixation suppressed the progression of MMPE and cartilage degeneration in the knee flexion position in a short-term 1-year unloaded MRI and arthroscopic evaluation. However, in the knee extension position, MMME progressed and correlated with the MFC cartilage degeneration. Transtibial fixation can restore the meniscal morphology at 90° knee flexion, even in elderly patients with poor healing ability. However, the postoperative MM conditions did not affect all good clinical scores by the 1-year follow-up.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ADL:
-
Activities of daily living
- BMI:
-
Body mass index
- ICC:
-
Intra-class correlation coefficient
- ICRS:
-
International Cartilage Research Society
- IKDC:
-
International Knee Documentation Committee
- K–L:
-
Kellgren–Lawrence
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- LFC:
-
Lateral femoral condyle
- LTP:
-
Lateral tibia plateau
- MFC:
-
Medial femoral condyle
- MM:
-
Medial meniscus
- MMPRT:
-
Medial meniscus posterior root tear
- MMME:
-
Medial meniscus medial extrusion
- MMPE:
-
Medial meniscus posterior extrusion
- MRI:
-
Magnetic resonance imaging
- MTP:
-
Medial tibia plateau
- QOL:
-
Quality of life
- VAS:
-
Visual analogue scale
References
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus, similar to total meniscectomy. J Bone Jt Surg Am 90:1922–1931
Bae JH, Paik NH, Park GW, Yoon JR, Chae DJ, Kwon JH, Kim JI, Nha KW (2013) Predictive value of painful popping for a posterior root tear of the medial meniscus in middle-aged to older asian patients. Arthroscopy 29:545–549
Bhatia S, LaPrade CM, Ellman MB, LaPrade RF (2014) Meniscal root tears: significance, diagnosis and treatment. Am J Sports Med 42:3016–3030
Chung KS, Ha JK, Ra HJ, Kim JG (2016) A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc 24:1455–1468
Chung KS, Ha JK, Ra HJ, Lee HS, Lee DW, Park JH, Kim DH, Kim JG (2019) Pullout fixation for medial meniscus posterior root tears: clinical results were not age-dependent but osteoarthritis progressed. Knee Surg Sport Traumatol Arthrosc 27:189–196
DePhillipo NN, Moatshe G, Chahla J, Aman ZS, Storaci HW, Morris ER, Robbins CM, Engebretsen L, LaPrade RF (2019) Quantitative and qualitative assessment of the posterior medial meniscus anatomy: defining meniscal ramp lesions. Am J Sports Med 47:372–378
Fujii M, Furumatsu T, Kodama Y, Miyazawa S, Hino T, Kamatsuki Y, Yamada K, Ozaki T (2017) A novel suture technique using the FasT-Fix combined with Ultrabraid for pullout repair of the medial meniscus posterior root tear. Eur J Orthop Surg Traumatol 27:559–562
Fujii M, Furumatsu T, Xue H, Miyazawa S, Kodama Y, Hino T, Kamatsuki Y, Ozaki T (2017) Tensile strength of the pullout repair technique for the medial meniscus posterior root tear: a porcine study. Int Orthop 41:2113–2118
Furumatsu T, Kodama Y, Fujii M, Tanaka T, Hino T, Kamatsuki Y, Yamada K, Miyazawa S, Ozaki T (2017) A new aiming guide can create the tibial tunnel at favourable position in transtibial pullout repair for the medial meniscus posterior root tear. Orthop Traumatol Surg Res 103:367–371
Furumatsu T, Okazaki Y, Kodama Y, Okazaki Y, Masuda S, Kamatsuki Y, Takihira S, Hiranaka T, Yamawaki T, Ozaki T (2019) Pullout repair using modified Mason–Allen suture induces better meniscal healing and superior clinical outcomes: a comparison between two surgical methods. Knee 26:653–659
Furumatsu T, Okazaki Y, Okazaki Y, Hino T, Kamatsuki Y, Masuda S, Miyazawa S, Nakata E, Hasei J, Kunisada T, Ozaki T (2019) Injury patterns of medial meniscus posterior root tears. Orthop Traumatol Surg Res 105:107–111
Hasegawa A, Otsuki S, Pauli C, Miyaki S, Patil S, Steklov N, Kinoshita M, Koziol J, D’Lima DD, Lotz MK (2012) Anterior cruciate ligament changes in the human knee joint in aging and osteoarthritis. Arthritis Rheum 64:696–704
Hino T, Furumatsu T, Miyazawa S, Fujii M, Kodama Y, Kamatsuki Y, Okazaki Y, Ozaki T (2018) A histological study of the medial meniscus posterior root tibial insertion. Connect Tissue Res 9:1–8
Kamatsuki Y, Furumatsu T, Fujii M, Kodama Y, Miyazawa S, Hino T, Ozaki T (2018) Complete tear of the lateral meniscus posterior root is associated with meniscal extrusion in anterior cruciate ligament deficient knees. J Orthop Res 36:1894–1900
Kawahara Y, Uetani M, Fuchi K, Eguchi H, Hayashi K (1999) MR assessment of movement and morphologic change in the menisci during knee flexion. Acta Radiol 40:610–614
Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ (2011) Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy 27:1644–1653
Kim JY, Bin SI, Kim JM, Lee BS, Oh SM, Cho WJ (2019) A novel arthroscopic classification of degenerative medial meniscus posterior root tears based on the tear gap. Orthop J Sports Med 7:232596711982794
Kodama Y, Furumatsu T, Fujii M, Tanaka T, Miyazawa S, Ozaki T (2016) Pullout repair of a medial meniscus posterior root tear using a FasT-Fix® all-inside suture technique. Orthop Traumatol Surg Res 102:951–954
Krych AJ, Reardon PJ, Johnson NR, Mohan R, Peter L, Levy BA, Stuart MJ (2017) Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc 25:383–389
LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF (2014) Meniscal root tears: a classification system based on tear morphology. Am J Sports Med 43:363–369
LaPrade RF, LaPrade CM, James EW (2015) Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg 23:71–76
Lee SS, Ahn JH, Kim JH, Kyung BS, Wang JH (2018) Evaluation of healing after medial meniscus root repair using second-look arthroscopy, clinical and radiological criteria. Am J Sports Med 46:2661–2668
Masuda S, Furumatsu T, Okazaki Y, Kodama Y, Hino T, Kamatsuki Y, Miyazawa S, Ozaki T (2018) Medial meniscus posterior root tear induces pathological posterior extrusion of the meniscus in the knee-flexed position: an open magnetic resonance imaging analysis. Orthop Traumatol Surg Res 104:485–489
Okazaki Y, Furumatsu T, Yamaguchi T, Kodama Y, Kamatsuki Y, Masuda S, Okazaki Y, Hiranaka T, Zhang X, Ozaki T (2019) Medial meniscus posterior root tear causes swelling of the medial meniscus and expansion of the extruded meniscus: a comparative analysis between 2D and 3D MRI. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05580-6
Padalecki JR, Jansson KS, Smith SD, Dornan GJ, Pierce CM, Wijdicks CA, Laprade RF (2014) Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med 42:699–707
Patel R, Eltgroth M, Souza R, Zhang CA, Majumdar S, Link TM, Motamedi D (2016) Loaded versus unloaded magnetic resonance imaging (MRI) of the knee: effect on meniscus extrusion in healthy volunteers and patients with osteoarthritis. Eur J Radiol 3:100–107
Seil R, Duck K, Pape D (2011) A clinical sign to detect root avulsions of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 19:2072–2075
Todor A, Caterev S, Nistor DV (2016) Outside-in deep medial collateral ligament release during arthroscopic medial meniscus surgery. Arthrosc Tech 5:781–785
Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM (1999) Meniscal movement. An in-vivo study using dynamic MRI. J Bone Jt Surg Br 81:37–41
Acknowledgements
We would like to thank Editage (https://www.editage.jp) for English language editing.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kodama, Y., Furumatsu, T., Masuda, S. et al. Transtibial fixation for medial meniscus posterior root tear reduces posterior extrusion and physiological translation of the medial meniscus in middle-aged and elderly patients. Knee Surg Sports Traumatol Arthrosc 28, 3416–3425 (2020). https://doi.org/10.1007/s00167-019-05810-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05810-x