Abstract
Purpose
To evaluate short- to midterm outcomes of medial patellofemoral ligament reconstruction (MPFL) using patient-reported outcome measures and functional testing.
Methods
Twenty-four patients were examined regarding knee function after MPFL reconstruction, with a mean follow-up time of 45.3 ± 18.4 months since surgery. Knee function was evaluated using the Tegner score, VAS, the knee injury and osteoarthritis outcome score (KOOS), the Lysholm score, SF-36 and EQ-5D-3L as well as functional scores. A group of uninjured persons of the same age and same gender composition was used for comparison.
Results
Eight (40%) patients managed to return to their pre-injury activity level. Five (25%) patients stated that they had experienced further patella dislocations after surgery but only two (10%) had sought medical help. Patients showed significantly poorer results in all PROMs compared to controls. The results obtained with SF-36 showed significant differences in physical health between the groups, but not in mental health. The functional performance test results showed overall poorer results for the patients versus controls: 11.5 sets for the square jump (6.7–15.7) versus 21 sets (18–26), 11.5 sets for the step-down test (6.5–15) versus 22 sets (18–26), and 77 cm for the single-leg hop for distance (32.2–110.5) versus 126 cm (115–37); all (P < 0.005).
Conclusions
After MPFL reconstruction, patients do not regain normal knee function, as measured by PROMs and functional tests, compared to an uninjured control group. Patients should be informed about residual functional limitations despite improved stability.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The annual incidence of primary patella dislocation worldwide is reported at 5.8 per 100,000. Residual problems are common and can lead to significant functional restraints and limitations on everyday activities and sports due to knee instability and pain [5, 6].
The treatment of choice after primary patellar dislocation is non-surgical, except for injuries with large osteochondral fragments that may require immediate surgical treatment. Surgery is usually indicated after recurrent dislocations [10]. One of the primary surgical treatments for recurrent patella instability is reconstruction of the medial patellofemoral ligament (MPFL) [8]. The results are good in terms of patient-reported outcomes [6] with reported re-dislocation rates in the range of 0–17% [6, 8]. However, to the best of our knowledge, no study has evaluated knee function after surgery using standardized physical tests.
The purpose of this study was therefore, to evaluate short- to midterm outcomes of MPFL reconstruction using both patient-reported outcome measures (PROMs) and functional testing. PROMs provide subjective results and help us compare our study with others. Using functional tests, we can evaluate knee function in situations similar to everyday physical activities. Our hypothesis patients with recurrent patella dislocations who underwent MPFL reconstruction would experience good knee function and a low rate of residual dislocation.
Materials and methods
The patients included in this retrospective study were identified from medical records on surgical procedures between 2008 and 2013. The minimum follow-up time was 18 months. All patients were treated with MPFL reconstruction at a university hospital in Sweden. Patient characteristics are presented in Table 1.
The indication for surgery was recurrent patella dislocations despite adequate physiotherapy. Adequate physiotherapy was defined as at least 6 months of supervised training sessions 1–2 times per week at a specialized institution. It was established from medical records that all the patients had two or more confirmed dislocations prior to surgery. The median age of the patients at the time of surgery was 20 (13–41) years. The patients were scheduled for clinical follow-up evaluations at the hospital 6 weeks and 3 months after their procedures. After that, there were only follow-ups if needed.
Patients suffering from diabetes, rheumatic diseases, neuromuscular diseases, Ehler-Danlos syndrome and Down’s syndrome were excluded, as were patients with severe psychosocial disorders and known substance abuse.
The patients in this study went through a treatment algorithm used by experienced surgeons. Patients were scheduled for MPFL- reconstruction only if their q-angle was not obviously pathological; their TT-TG distance was not over 20 mm, which would have directed them towards a distal realignment or combined procedure; or they had a level of trochlea dysplasia (types B or D according to Dejour), which would have directed them towards trochleaplasty.
The MPFL reconstruction was performed using a free gracilis tendon graft anatomically positioned with the use of peroperative radiographs as described by Schottle et al. [21].
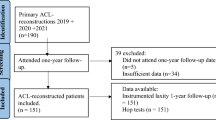
Thirty-six patients met the criteria and were invited to participate in the follow-up study, which included both PROMs and clinical functional testing. Eight patients chose not to participate because they were not interested, did not have the time or had moved away from the area. None of these patients had sought medical help because of re-dislocations. Three patients could not be reached, and one patient was excluded because of mental illness. The remaining 24 completed and sent in self-reported outcome questionnaires, and 20 of these participated in the clinical functional testing. The other four could not attend the clinical assessment because of other minor health issues or because they had moved to another region of Sweden.
Because the hypothesis was that knee function after surgery would be good in comparison to uninjured knees, a healthy control group was chosen for comparison. The control group consisted of 22 subjects recruited from the university medical school. They underwent the same assessment as the patients, although three did not complete the self-reporting questionnaires. The controls had no medical history of surgery or significant injuries in the lower extremities or hip. The subjects in the control group were not pair-matched, but their age and level of activity were similar to those of the patients. Since this injury is more common among females, the uninjured control group contained more females than males. Because no differences were observed between the right and left legs of the controls, their right legs were used for comparison [4].
Study design
This is a retrospective study of subjects who had undergone isolated MPFL reconstruction between 2008 and 2013 with a mean follow-up time of 45.3 ± 18.4 months. Four of the 24 patients had a follow-up time that was less than 24 months but had been discharged and medically cleared from physical therapy.
All 36 eligible patients were sent self-reporting questionnaires. Those who chose to participate in the study underwent a physical assessment at the clinic, which included patient history, knee symptoms and function, and range of motion measured with a goniometer. The patients were also asked to estimate their level of knee pain during the past few weeks, from 0 to 10 on a visual analogue scale (VAS) [16]. The patients were asked to estimate how many patella dislocations they had experienced before and after surgery, how many months of physiotherapy they had completed after surgery and whether they had experienced any other complications. The subjects in the control group completed the same physical assessments and self-reporting questionnaires.
Patient-reported outcomes
All eligible patients were asked to complete the following validated questionnaires: Tegner activity Scale [25], the Knee injury and Osteoarthritis Outcome Score (KOOS) [20], the Lysholm knee score [11] as well as the 36-Item Short Form Survey (SF-36) [24] and European quality of life-5 dimensions -3L (EQ-5D-3L) and EQ-5D-3L-VAS (health status of the day of the interview) [12] to evaluate patient satisfaction and quality of life.
Functional tests
The square jump test, the step-down test and the single-leg hop for distance were used to evaluate knee function.
Square jump test This validated test was included in the study to evaluate knee stability during multidirectional movements [19]. The number of jumps successfully performed without touching the frame was recorded.
Step-down test This unilateral test has good reliability and emulated walking down a step. The number of times patients could repeat the test in 30 s was recorded [16].
Single-leg hop for distance This validated test was originally developed to evaluate anterior cruciate ligament deficiency but it has also proven reliable in healthy participants. Strength, coordination and agility are evaluated by putting stress on the quadriceps, hamstrings, and hip muscle [3]. This test can be performed either with the patient’s hands behind their back [19] or hanging freely at the side of the body. The latter method was used in this study [3]. The subject was instructed to hop as far as they could, while maintaining their balance and postural control. Three hops were performed on each leg with the possibility of a fourth if the hops were longer each time [3, 19].
Ethics
This study began as a student project that was approved by the faculty of Medicine at Lund University in compliance with all the rules of the Swedish Ethical Review Act. Under that Act, an additional IRB approval is not necessary. In fact, it cannot be issued after the study has begun. All patients and controls were informed both in writing and orally about the study and completed informed consent forms before enrollment. All patients had the option to withdraw from the study at any time.
Statistical analysis
The statistical analysis was performed with the SPSS Statistics for MAC 22.0 software package. Patient characteristics and descriptive data are presented as the mean, range and standard deviation unless otherwise stated, while the results of the self-reported questionnaires and the functional tests are presented as the median and interquartile range (Q1–Q3). Because of the small size of the study group, the non-parametric Mann–Whitney U test was used to compare the two independent groups. A P value < 0.05 was defined as indicating statistical significance. Power analysis was not performed prior to the study due to its exploratory nature. However, a post hoc power analysis showed a 99% power for the different KOOS subscales (n = 22 patients, n = 24 controls) and over a 90% power for the functional performance tests (n = 20 patients, n = 22 controls).
Results
Physical assessments showed that patients had a poorer range of motion regarding flexion: 130° (125°–130°) compared to the controls 132.5° (130°–140°) (P < 0.005). No difference in knee extension was found between the groups. Five of 20 patients who participated in the clinical assessment had experienced a dislocation after surgery, but only two had sought medical attention for it. Patients’ median Tegner activity levels are presented in Table 2. Eight (40%) of patients managed to return to their pre-injury activity level. The visual analogue scale for pain over the past week (VAS) together with Lysholm score and Quality of life measured by EQ-5D-3L are presented in Table 2.
Patients versus control group median KOOS results are presented in Table 3.
The results obtained with SF-36 are presented in Fig. 1. Patients versus control group median SF36 PCS (physical component summary) and SF 36 MCS (mental component summary) scores and interquartile range (Q1–Q3) were: SF36 PCS 46 (36–50) versus 58 (56–59), (p < 0.005): SF36 MCS 47(39–56) versus 45 (40–49), (n.s.).
The functional performance tests showed overall poorer results for the patients as compared to the controls: 11.5 sets for the square jump (6.7–15.7) versus 21 sets (18–26), 11.5 sets for the step-down test (6.5–15) versus 22 sets (18–26), and 77 cm for the single-leg hop for distance (32.2–110.5) versus 126 cm (115–37); all (P < 0.005), Fig. 2.
Discussion
The most important finding of this study is that patients who have undergone MPFL reconstruction do not regain normal knee function after surgery. Compared to healthy controls, they show significantly poorer results in both PROMs and functional tests. The re-dislocation rate after surgery was 2/20 (10%), according to medical records, i.e., those seeking medical help. However, when the patients were asked if they had experienced recurrent dislocations, 5/20 (25%) stated that they had. In a review by Buckens et al. [6] lower re-dislocation frequencies between 0 and 8% and a subluxation frequency of 0–10% were reported. Camp et al. [7] reported a higher recurrent dislocation rate of 28% (8 patients), only three of whom did not require reoperation. Enderlein et al. [8] carried out one of the largest studies on the success of MPFL reconstruction which included 224 patients. They found a re-dislocation rate of 4.5%, but over 39% had experienced a sensation of subluxation. The study did not include any functional tests. The definition of postoperative re-dislocation in several of the studies is vague, and no clear differentiation is made between subluxation and dislocation. Furthermore, it is difficult for patients to define the sensation of instability, indicating that functional tests provide a useful complement to the assessment of those patients, and may provide additional information to create a more accurate picture of knee function than subjective scores and re-dislocation or reoperation rates alone.
Another problem in comparing different studies is the long time between primary dislocation and surgery, as well as the long follow-up time and possible development of osteoarthritis in some cases. In a study by Numera et al. [18] the mean time from the first dislocation to surgery was 4.6 (0.8–25) years. Patients who showed moderate to severe osteoarthritic changes at radiograph examination were excluded from their analysis. In the present study, mean time to surgery was 8.4 (1–27) years, which is considerably longer. This is because surgery was not indicated unless the patient had repeated dislocations after adequate physiotherapy. Patients who had developed osteoarthritis were not offered surgery and were, therefore, not included in our study.
The patients in this study had slightly poorer range of motion regarding flexion than the control group. However, the clinical significance of this finding was not investigated, as the test did not involve kneeling, deep squats or similar movements. A limited range of motion is common after knee surgery, and it is rare for patients to regain full movement [22].
The Tegner activity scores showed that 40% of the patients were able to return to their pre-injury activity level or higher. The scores in this study, a median of 6 before injury and a median of 5 post-injury, are comparable to values reported in some studies [15]. For example, Lim et al. [15] reported a mean post-surgery Tegner activity score of 3.45. However, the patients in the present study had lower Lysholm knee scores than in previous studies. A median score of 74 is a reasonable result, but not as good as the average postoperative scores of 89–92 given in some systemic reviews [6, 9]. Although MPFL reconstruction was the focus of most studies, several studies considered a combined approach that involved MPFL reconstruction together with tibial tubercle transfer, lateral release or chondroplasty [5, 9]. Ahmad et al. [1] reported a post-surgery Lysholm score of 88.7 in a study where surgery combined with distal realignment procedures or additional ligament reconstruction was excluded—similar to the inclusion criteria of this study. However, only subluxations, not confirmed dislocations were required for surgery, so their patient profile is not directly comparable to ours.
The median value of pain on the VAS was 3, indicating that patients still experienced some pain several years after surgery. This corresponds with findings of other studies, in which a decrease in pain was observed after surgery, although some patients experienced pain during some sporting activities and others even in everyday life [13]. According to Aktin et al. [2] 56% of patients still experienced pain 24 weeks after surgery.
The KOOS profile of the patients in the present study was lower than that of the control group but still indicated a good overall result regarding activities of daily living and pain, which is in line with the findings of Larsson et al. [14].
Significant differences were found in both SF-36 and EQ-5D-3L between the patients and the controls. The controls reported a subjectively better state of health. However, consistent with other studies, the patients reported overall good health despite their injured knees [9].
The patients’ functional performance was significantly poorer than that of the control group in all three tests. These tests reveal difficulties that cannot be discovered with questionnaires. The difference may be due not only to patients’ weaker muscles, but also to psychological factors such as lack of confidence in knee reliability [9]. The most efficient physical treatment has not yet been determined, and it has been shown that muscle strength is reduced after rehabilitation regardless of treatment [23]. Furthermore, the fact that patients with patellar instability are often complex cases with alterations in soft tissue restraint and ligament function, as well as skeletal abnormalities, makes it difficult to restore normal knee function. The surrounding structures may be impaired after multiple patella dislocations, and cartilage lesions may prevent complete functional recovery [17]. Surgery can cause scarring and, in some cases, create an under- or over-constrained MPFL, which may affect knee function [7].
A variety of outcome measures and clinical tests can be used to diagnose and evaluate patella instability prognosis. A specific functional test or patient-reported outcome measure for this patient group has not yet been developed, which warrants future studies in this field.
This study was based on a small number of participants: ~ 20 subjects in each group. The control group was not pair-matched. For some of the PROMs the patients had to estimate knee function several years back in time. These data about symptoms, rehabilitation and levels of activity are, therefore, less reliable. Radiograph examinations were not used at follow-up to assess post-traumatic arthritis, which made it difficult to fully explain the reasons for the poorer results in the patient group. According to the treatment algorithm, no patients with significantly increased Q-angle or TT-TG distance over 20 mm should be present in this group. However, we have no data on these measurements.
Conclusions
Results showed that patients with recurrent patellar dislocations treated with MPFL reconstruction did not regain normal knee function, as measured by PROMs and functional tests. Due to the limitations described above, no certain conclusions could not be drawn regarding the cause of these results, though possibilities include laxity, insufficient rehabilitation and impaired neuromuscular control, anatomical variations, or development of osteoarthritis. Patients undergoing MPFL reconstruction should be informed about the residual functional limitations they are likely to experience despite their improved post-surgery stability.
Abbreviations
- MPFL:
-
Medial patellofemoral ligament
- PROMs:
-
Patient reported outcome measures
- VAS:
-
Visual analogue scale
- KOOS:
-
Knee injury and Osteoarthritis Outcome Score
- EQ-5D-3L:
-
European quality of life—5 dimensions
References
Ahmad CS, Brown GD, Stein BS (2009) The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med 37:2021–2027
Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C (2000) Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med 28:472–479
Augustsson J, Thomee R, Linden C, Folkesson M, Tranberg R, Karlsson J (2006) Single-leg hop testing following fatiguing exercise: reliability and biomechanical analysis. Scand J Med Sci Sports 16:111–120
Bade MJ, Kohrt WM, Stevens-Lapsley JE (2010) Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sports Phys Ther 40:559–567
Baer MR, Macalena JA (2017) Medial patellofemoral ligament reconstruction: patient selection and perspectives. Orthop Res Rev 9:83–91
Buckens CF, Saris DB (2010) Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: a systematic review. Am J Sports Med 38:181–188
Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ (2010) Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med 38:2248–2254
Enderlein D, Nielsen T, Christiansen SE, Faunø P, Lind M (2014) Clinical outcome after reconstruction of the medial patellofemoral ligament in patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc 22:2458–2464
Fisher B, Nyland J, Brand E, Curtin B (2010) Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: a systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy 26:1384–1394
Frosch S, Balcarek P, Walde TA, Schuttrumpf JP, Wachowski MM, Ferleman KG et al (2011) The treatment of patellar dislocation: a systematic review. Z Orthop Unfall 149:630–645
Johnson DS, Smith RB (2001) Outcome measurement in the ACL deficient knee—what’s the score? Knee 8:51–57
Karlsson JA, Nilsson JA, Neovius M, Kristensen LE, Gulfe A, Saxne T et al (2011) National EQ-5D tariffs and quality-adjusted life-year estimation: comparison of UK, US and Danish utilities in south Swedish rheumatoid arthritis patients. Ann Rheum Dis 70:2163–2166
Kohn LM, Meidinger G, Beitzel K, Banke IJ, Hensler D, Imhoff AB et al (2013) Isolated and combined medial patellofemoral ligament reconstruction in revision surgery for patellofemoral instability: a prospective study. Am J Sports Med 41:2128–2135
Larson E, Edwards A, Albright J (2014) Functional outcomes of MPFL reconstruction vs. graft tissue placement. Iowa Orthop J 34:38–43
Lim AK, Chang HC, Hui JH (2008) Recurrent patellar dislocation: reappraising our approach to surgery. Ann Acad Med Singapore 37:320–323
Loudon JK, Wiesner D, Goist-Foley HL, Asjes C, Loudon KL (2002) Intrarater reliability of functional performance tests for subjects with patellofemoral pain syndrome. J Athl Train 37:256–261
Ménétrey J, Putman S, Gard S (2014) Return to sport after patellar dislocation or following surgery for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc 22:2320–2326
Nomura E, Horiuchi Y, Kihara M (2000) A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar dislocation. Knee 7:211–215
Ostenberg A, Roos E, Ekdahl C, Roos H (1998) Isokinetic knee extensor strength and functional performance in healthy female soccer players. Scand J Med Sci Sports 8:257–264
Roos EM, Lohmander LS (2003) The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64
Schottle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35:801–804
Shah N (2008) Increasing knee range of motion using a unique sustained method. N Am J Sports Phys Ther 3:110–113
Smith TO, Davies L, Chester R, Clark A, Donell ST (2010) Clinical outcomes of rehabilitation for patients following lateral patellar dislocation: a systematic review. Physiotherapy 96:269–281
Sullivan M, Karlsson J, Ware JE Jr (1995) The Swedish SF-36 Health Survey—I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med 41:1349–1358
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Funding
No fundings have been recieved.
Author information
Authors and Affiliations
Contributions
All authors were involved in the design of the study. MB and AJ performed data collection and data analysis. MB together with DR and IK drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Biesert, M., Johansson, A., Kostogiannis, I. et al. Self-reported and performance-based outcomes following medial patellofemoral ligament reconstruction indicate successful improvements in knee stability after surgery despite remaining limitations in knee function. Knee Surg Sports Traumatol Arthrosc 28, 934–940 (2020). https://doi.org/10.1007/s00167-019-05570-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05570-8