Abstract
Purpose
A varus-producing medial closing wedge high tibial osteotomy (MCWHTO) is an uncommon procedure. The aim of this retrospective study was to assess the survivorship and prevalence of post-operative subjective knee laxity and satisfaction in a large cohort of patients with a MCWHTO performed without a MCL-reefing procedure.
Methods
All patients (n = 176) who underwent a MCWHTO in our clinic between 2008 and 2016 were approached to participate. After review of patient charts, questionnaires were sent to willingly patients. Primary outcome was the survivorship of the MCWHTO; secondary outcome was patient-reported instability and satisfaction.
Results
One-hundred and thirteen patients participated in the study. The 5-year survival rate of the MCWHTO was almost 80%. A total of 77% of the patients was satisfied with the treatment. With regard to post-operative subjective knee laxity, 26% of the patients experienced instability of the knee post-operation. Instability was significantly correlated with the KOOS domains, the Lysholm score, the IKDC knee function score and the Physical and Mental Health Domains of the SF-36.
Conclusion
Medial closing wedge high tibial osteotomy provides good results regarding survivorship and patient satisfaction for patients with a valgus deformity which is located in the proximal tibia. Clinically relevant is that in the surgical technique without MCL-reefplasty instability is significantly correlated with worse patient-reported outcome measures. The addition of a MCL reefing procedure will improve outcome in selected patients.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High tibial osteotomy (HTO) is a surgical method to correct malalignment of the leg and has proven to be a good therapeutic option for delaying and potentially preventing the progression of knee OA. HTO is most favourably performed in the more active and younger patient in whom total knee arthroplasty (TKA) is less desirable [22].
Osteotomy procedures for varus malalignment are frequently performed. Valgus malalignment deformity of the knee, however, is much less frequent (2–2.8%) [1]. The corrective procedure, i.e. a varus-producing osteotomy in these valgus knees, is most often performed in the distal femur [10, 19]. Correction in the proximal (or high) tibia is much less common. However, if the valgus leg deformity is located in the tibia, the correction should be performed in the tibia to prevent an abnormal knee joint line obliquity [6, 11]. Besides the lateral open wedge HTO technique alternatively, a medial closing wedge HTO (MCWHTO) can be performed to correct the valgus leg alignment [2, 3].
A recent study by Mirouse et al. [17] showed unsatisfactory medium-term outcomes for high tibial varus osteotomies. In 19 consecutive patients, they reported an overall failure rate of 52% at mean follow-up of 4.3 years and they concluded that this procedure should not be performed in valgus osteoarthritic patients. In contrast, good clinical outcomes were reported previously in a gait analysis study on kinetics and kinematics of gait after a varus-producing HTO similar to that of a healthy control group [6]. Furthermore, in a recent prospective short-term study investigating laxity after MCWHTO performed in our own clinic, significant short-term improvements in patient-reported outcome scores, such as knee pain, functioning and quality of life (QoL), were found in all 11 patients [15]. However, also increased MCL laxity at mean 6 months post-operation was found which urged us to review our MCWHTO-patient population.
The medial collateral ligament laxity has been found to increase in instrumented laxity measurements performed pre- and post-operatively after MCWHTO [15]. The risk of increased laxity after MCWHTO had been described by Coventry in the past. He stated that, by removing a bony wedge on the medial side of the proximal tibia, a laxity of the superficial medial collateral ligament (MCL) is introduced and he, therefore, suggests to perform a surgical reefing procedure at all times to tighten the MCL [4, 5]. Historically, in our clinic no reefing procedures of the MCL have been performed during MCWHTO as wedge removal was performed below the level indicated by other authors. Therefore, the complete deep MCL and part of the superficial MCL inserts proximal of the osteotomy cuts and instability has not been a common complaint by our patients after these procedures.
The aim of this retrospective study was to assess the survivorship and prevalence of subjective knee laxity in a large cohort of patients who underwent MCWHTO without MCL-reefingplasty. We hypothesize that subjective knee laxity does not occur more often in MCWHTO without MCL-reefingplasty compared to historic MCWHTO cohorts with reefingplasty and, therefore, we expect comparable outcomes regarding patient satisfaction and survival. In addition, the possible relationships between instability and knee pain, functioning and QoL were explored. Furthermore, we tried to identify possible factors that may influence knee instability post-operation.
Materials and methods
All patients older than 18 years who underwent a unilateral or bilateral varus-producing MCWHTO between 2008 and 2016 in the Sint Maartenskliniek were selected from the hospital’s electronical medical record system. Minimal follow-up was set at 6 months. Since full weight-bearing without the use of walking aids was allowed after 4 weeks, reliable outcomes can be expected at this follow-up time. The surgery criteria were symptomatic valgus malalignment located in the proximal tibia, indication for a medial CWHTO, based on the severity of the complaints and the observed deformity according to Paley [18]. Patients were excluded if they had a double-level osteotomy of the knee, were lost to follow-up after the surgery, had an amputation of the operated leg, underwent a medial reefing procedure, initially or after the MCWHTO or were deceased. Patients were contacted by telephone and asked if they were willing to participate in the study, including a telephone survey and a questionnaire. If patients were not available by phone after multiple attempts, background information and questionnaires were sent by mail. This study was approved by the local Medical Research and Ethical Committee of the Maartenskliniek Woerden. Medical ethical approval number: (0665).
Surgical technique
The operations were performed by three different orthopaedic surgeons using the same technique consisting of oblique transverse cuts and a biplanar tuberosity cut correcting to neutral mechanical alignment (Fig. 1). The osteotomy site is located at approximately 4–5 cm below the medial tibia plateau and runs oblique towards the tip of the fibula. The biplanar tuberosity cut is performed in a proximal direction to ensure compression on the osteotomy site by the patellar tendon. Fixation after closure was performed with an angle-stable Tomofix plate. The location of the wedge removal is distal to the attachment of the deep part of the MCL and just within the attachment of the superficial part of the MCL on the medial proximal tibia [14]. Post-operative full weight-bearing was allowed directly post-operation. After 4 weeks no walking aids were mandatory.
Pre- and post-operative radiographs of a medial closing wedge high tibia osteotomy. The pre-operative alignment is shown in the long-leg radiograph (a). The osteotomy pre- and post-operative views in the coronal plane are shown in b and c. d, e Show the lateral view of the pre- and post-operative knee. In d the biplanar tuberosity cut is clearly shown
Measurements
When the patient agreed to participate, patient charts were consulted to gather information about the patient’s amount of correction, indication of surgery, re-operations, time to re-operation, and the occurrence of plate removal. Pre- and post-operative hip–knee–ankle angle measurements were made to the nearest 0.1° with use of the measurement tool within the radiographic database programme (Sectra workstation IDS7, version 16.1.22.1566 (2015), Sectra AB, Linköping, Sweden). During the telephone interview, patients were asked to indicate if they experienced instability of the operated knee at this moment and if they had experienced instability of the operated knee at the moment of full weight-bearing after surgery. Also, re-operations and the satisfaction about the result of the surgery were evaluated. Finally, patients were asked to fill in questionnaires, patient-reported outcome measurements (PROMs), documenting subjective knee laxity, functioning and quality of life. The validated Dutch Knee Injury and Osteoarthritis Outcome Score (KOOS) was used to assess subjective knee function and quality of life and consists of five different subscales: (1) pain, (2) symptoms, (3) function in daily living, (4) function in sports and recreation, and (5) knee-related quality of life [8, 20]. The score for each subscale was calculated, where 0 indicates severe knee problems and 100 indicates no knee problems. The validated Dutch International Knee Documentation Committee (IKDC) Subjective Knee Form was used to assess symptoms and limitations in function and sports. A higher score indicates a better function (0–100 scale) [9, 12]. The IKDC Current Health Assessment Form (SF36 form) was used to measure health status with respect to different dimensions: (1) physical functioning, (2) social functioning, (3) role limitations due to physical problems, (4) role limitations due to emotional problems, (5) bodily pain, (6) mental health, (7) vitality, (8) general health perception, and (10) change in perceived health during the last 12 months. All raw scores were converted to a 0–100 scale, with higher scores indicating higher levels of functioning or well-being. The Lysholm knee scale was used to assess ligament injuries of the knee [7, 13]. In addition, patients were asked to fill in a NRS Instability, with a higher score indicating more instability of the operated knee at this moment (range 0–10).
Statistical analysis
Patient characteristics, feeling of instability and patient satisfaction with the treatment were analyzed descriptively and reported as means with standard deviations and ranges or as numbers and percentages. The Kaplan–Meier method was used to estimate the probability of survival of the MCWHTO. Failure of the MCWHTO was defined as a redo HTO or TKA. The NRS Instability score were compared between (1) patients who at the time of the survey experiencing instability of the operated knee and patients who did not, (2) patients with a post-traumatic indication for correction and patients who had not, and (3) patients who had a redo HTO or TKA and patients who had not. Mann–Whitney U tests were used for the analysis. The correlation between the amount of post-operatively correction in mm and the severity of knee instability as measured with the NRS Instability score was analyzed using Spearman’s correlation. To assess possible relationships between the severity of knee instability as measured with the NRS Instability score and the (1) KOOS, (2) SF36 form and (3) Lysholm knee scale, also Spearman’s correlation was used.
Results
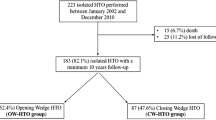
A total of 176 patients underwent a unilateral or bilateral varus-producing MCWHTO between 2008 and 2016 in the Maartenskliniek Woerden. Indications varied from valgus leg deformity acquired after growth disorders without osteoarthritis, post-meniscectomy lateral compartment osteoarthritis, primary lateral compartment osteoarthritis, post-traumatic lateral osteoarthritis after malunited tibia plateau fractures, and salvage realignment procedures preceding TKR placement. Figure 2 shows the flow diagram of patients included in the study. Of the 142 patients who were approached, 113 patients (80%) agreed to participate in the study. Patient characteristics are given in Table 1. Mean age was 50 years (SD 11.5); two-thirds of the patients were female (69%). The hip–knee–ankle (HKA) angle was changed from a pre-operative mean of 5.9° valgus (SD 4.3) to a mean of 0.1° varus (SD 3.4) post-operatively. The mean time post-surgery was 56 months and varied from 6 months to almost 17 years. The majority of the patients reported to have a job (74%) and a small majority participated in sports (62%).
Knee laxity
A total of 28 patients experienced instability of the operated knee at the time of the survey. 27 patients indicated that they experienced instability of the operated knee starting at the moment of full weight-bearing after surgery (see Table 2). 19 out of the 27 patients who experienced instability of the operated knee after surgery still experienced knee instability at follow-up. 66 out of the 74 patients that did not experience instability of the operated knee after surgery still had no instability complaints at follow-up. The remaining eight patients developed instability over time. There was a significant difference in NRS Instability score between patients who were currently experiencing instability of the operated knee and patients who were not: 6.7 (± 2.4) and 3.2 (± 2.7) (p < 0.01).
Further subgroup analysis based on indication for surgery showed no significant difference in NRS Instability scores between patients with a post-traumatic or salvage indication for correction and patients in any of the other indication groups: 4.5 (± 3.2) and 4.2 (± 3.0) (n.s.). No correlation was found between the amount of post-operative correction and the severity of knee laxity as measured with the NRS Instability score.
Re-operations and survival
A total of 39 patients underwent at least one type of re-operation in our clinic or elsewhere. The type of operation was either an arthroscopy of the ipsilateral knee (n = 22), a redo HTO due to overcorrection (n = 3) or total knee arthroplasty (TKA, n = 14). Year of re-operation was missing in ten patients. A subgroup analysis for time to re-operation showed 19 patients with a re-operation < 2 years versus 10 patients with a late re-operation. No significant difference in NRS stability was found between these two groups: 4.8 (± 2.7) vs 6.3 (± 3.3) (n.s.).
Failed MCWHTO was present in 17 patients after a mean of 3.0 (± 2.6) years (n = 16, year of redo HTO/TKA is missing in 1 patient). The NRS Instability score was not different between patients who had a redo HTO or TKA and patients who had not: 4.6 (± 3.3) and 4.3 (± 3.0) (n.s.). The 5-year survival without a redo HTO or TKA was 79.9% (Fig. 3). A total of 5 out of the 17 patients with a failed MCWHTO indicated that they experienced instability of the operated knee post-surgery. There was no difference in the prevalence of failed MCWHTO between patients with or without instability of the operated knee post-surgery (n.s.).
Patient-reported outcome and correlation to knee instability
Table 3 shows the mean outcome scores in functioning and quality of life for the KOOS, SF36 and Lysholm knee scale. Knee instability was significantly correlated with the KOOS domains, the Lysholm score, the IKDC knee function score, and the Physical and Mental Health Domains of the SF36, indicating a higher subjective knee laxity score is being associated with worse scores on knee functioning and health status (Table 4).
The majority of the patients, 88 out of the 113 (78%) were satisfied with the surgery and would recommend the treatment to others, (see Table 1). Patients that were satisfied with the surgery had a significantly lower NRS Instability score compared to patients who were not satisfied: 3.81 (± 3.0) and 6.58 (± 2.2) (p < 0.01). Patients who underwent a re-operation were significantly less satisfied compared to those patients who did not need a re-operation (p = 0.02).
Discussion
The most important finding of the present study was that the 5-year survival rate of MCWHTO’s performed without MCL-reefingplasty was almost 80%. This is the largest cohort study to date to analyze patients who underwent a medial closing wedge high tibial osteotomy and a total of 78% of the patients was satisfied with the treatment. With regard to post-operative knee laxity, 25% of the patients experienced instability of the knee post-operative at the start of full weight-bearing and 70% remained to have instability complaints at 4.5-year follow-up. A negative correlation was found between instability and PROMs. No factors could be identified that could predict knee instability post-operation.
The 5-year survival rate of the present study (79.9%) shows a far better result compared to the 57.5% presented in the recent study by Mirouse et al. [17]. The only other study that published results with regard to survival rate after medial CWHTO is the study by Coventry [5]. He reported seven failures in 31 osteotomies (22.6%): one unicondylar prosthesis implantation 1 year after the osteotomy and six TKA placements with a mean time to re-surgery of 9.8 years. The high failure rate in the study of Mirouse et al. may be explained due to their inclusion criteria. They included patients with < 10° valgus deformity for the MCWHTO with disregard to the deformity evaluation. If the valgus deformity is in the femur and the correction is made in the proximal tibia, this will inflict joint line obliquity and may lead to persistent pain and HTO failure [5, 21]. As Coventry already stated in 1987: the final decision of whether to do an osteotomy of the proximal part of the tibia or of the distal part of the femur depends on the assessment of both the anatomical axis and the tilt of the tibial plateau. One must not be considered without the other [5]. The present study shows that with proper patient selection, paying attention to deformity analysis and only indicating patients with a tibial valgus deformity for a MCWHTO, the survivorship after MCWHTO seems within well acceptable limits. Furthermore, a gait analysis study on three patient groups after varization osteotomies correcting valgus leg alignment confirms the importance of leg correction at the location of the deformity preventing an abnormal joint line obliquity [6].
The prevalence of patient-reported knee laxity (25%) in this study is slightly higher than found in previous studies. Only two studies have studied this matter. Coventry assessed the knee laxity at 1-year post-operation after MCWHTO for 31 patients and documented four patients with marked laxity and 3 patients with a moderate laxity. This results in 22% laxity in their cohort. Coventry performed a reefing of the MCL in all his patients [5]. Shoji and Insall reported on 49 knees after MCWHTO. They reported instability as the presence of a thrust while walking. Although the number of patients with a thrust was 30 out of the 49, only a total of 10 patients (20%) complained about instability post-operation. They performed a distal advancement of the MCL in only 5 of the 49 patients with satisfactory results for 3 patients [21]. In this study, no MCL-reefingplasty has been performed in any of the patients and this may have resulted in a varus laxity as was previously shown in a cohort prospectively analyzed with instrumented laxity measurements [15]. As no objective laxity measurements had been performed pre-operatively and post-operatively in the patients of the present study, the subjective knee instability reported by the patients cannot be related to increased laxity caused by the MCWHTO. However, the lack of an MCL-reefingplasty in our patients might still explain the slightly higher prevalence of subjective knee instability in comparison with the other two studies. It remains uncertain whether all patients need an extra MCL-reefingplasty re-tensioning the MCL. Probably only those patients with clear per-operative MCL tension loss after wedge resection may benefit from this additional treatment.
A total of 78% of the patients was satisfied with the surgery and an equal amount would recommend this type of surgery to other persons. This result is in agreement with other studies. Coventry found major pain relief in 77% of his patients with a follow-up of 3–17 years [5]. Shoji and Insall reported 28 patients (57%) who were satisfied and 21 unsatisfied patients, with persistent pain being the mean reason for dissatisfaction [21]. They also noted that all of the 21 unsatisfied patients showed some form of instability. Another study by Chambat et al. reviewed 47 patients and reported a ‘very good’ or ‘good’ outcome with the Guépar score in 34 (72%) of their patients. The remaining 13 patients (28%) scored ‘fair’ and ‘bad’ but reflected patients with a very long follow-up [3]. In a recent study, Mirouse et al. described knee functional outcome in 19 patients after MCWHTO using the International Knee Society (IKS) score as primary outcome measure. They stated that an IKS score < 140 was undesirable and found that only nine patients (47%) had a score of 140 or higher [17]. However, as mentioned above inclusion criteria including valgus less than 10° for tibial correction irrespective of pre-operative valgus deformity in the femur are questionable and may cause worse results in their study. Using a lateral opening wedge varization HTO, an alternative to the MCWHTO technique described in the present study, Marti et al. reported an excellent or good knee score in 88% of their well selected patients with a mean follow-up of 11 years of 36 osteotomies [16].
Although we have found a good patient satisfaction in 88 of the 113 cases (78%), still almost a quarter of the patients indicated to be dissatisfied. We have shown that the patients who were dissatisfied with the surgery showed significant lower NRS instability scores compared to the satisfied patient group, so patient satisfaction may be influenced by knee instability. This result is also visible in the significant negative correlations regarding the PROMS. Almost all analyzed PROMS showed fair to strong negative correlation with subjective knee laxity reported by the patients. The key element, therefore, will be to identify which patients will be prone to develop this knee instability and may benefit from the reefing procedure of the MCL as was previously described by Coventry [4, 5]. However, to date no predictable model is available to select those patients who would benefit from this extra procedure. Therefore, we suggest that the surgeon intra-operatively checks the valgus laxity in flexion angles of 30° and 70° before and after performing the MCWHTO and if deemed necessary performs a reefingplasty of the MCL. This might prevent instability complaints post-operation and thereby might increase overall patient satisfaction.
The current study has some limitations. The retrospective nature is less reliable for evaluating patient outcome, especially the directly post-operative experienced subjective knee laxity. For some patients this was more than 10 years ago. Moreover, the wide range in follow-up, 6 months–17 years, is less reliable for survival analysis. Ideally, a minimal 2 years of follow-up would provide some more information with regard to early failure rates (within 1 year). However, due to a very limited number of studies regarding the varus-producing HTO, we believe this study will still contain valuable information to prove that a MCWHTO is a viable treatment option for patients with a tibial valgus deformity. Especially, long-term survival, outcome scores and subjective knee laxity after a MCWHTO without MCL-reefingplasty are of interest in answering our hypothesis. Another limitation is the rather large loss to follow-up group and the number of patients that were not willing to participate. We were only able to approach 142 patients of the total 167 eligible patients, and 113 of the 142 were willing to participate. This might inflict a bias in outcome. What the effect of this bias may be is hard to predict. Either really dissatisfied patients may refuse to participate or very satisfied patients for whom the operation was performed a long time ago. Therefore, we have assumed that the results are a good reflection of the cohort that was operated on between 2008 and 2016. Moreover, being the largest cohort on this type of surgery this study is clinically relevant as only a few studies with low patient numbers and conflicting results are available in the literature. Furthermore, this study has shown that a medial closing wedge HTO improves knee function and decreases complaints in a diverse population of patients with a tibial valgus malalignment. Instability possibly caused by increase of laxity after MCWHTO correlates negatively with outcome so intra-operative laxity testing is advised after MCWHTO, as an additional MCL-reefingplasty in patients with increased laxity may improve outcome.
Conclusion
This study shows that a medial closed wedge high tibial osteotomy without medial reefingplasty provides good results regarding survivorship and patient satisfaction for patients with a valgus deformity located in the proximal tibia despite slightly higher subjective knee laxity findings post-operation. Instability is significantly correlated with worse outcome and, therefore, a MCL-reefingplasty can improve the outcome in selected patients with an increase in MCL laxity per-operatively and as a result this laxity should be tested during surgery.
Abbreviations
- BMI:
-
Body mass index
- HKA:
-
Hip–knee–ankle
- HTO:
-
High tibial osteotomy
- IKDC:
-
International Knee Documentation Committee
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- MCL:
-
Medial collateral ligament
- MCWHTO:
-
Medial closing wedge high tibial osteotomy
- NRS:
-
Numeric rating scale
- PROMS:
-
Patient-reported outcome measurement scores
- SF-36:
-
Short Form 36
- TKA:
-
Total knee arthroplasty
- QoL:
-
Quality of life
References
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat Award: is neutral mechanical alignment normal for all patients?: the concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Cerciello S, Lustig S, Servien E, Batailler C, Neyret P (2017) Correction of tibial valgus deformity. J Knee Surg 30:421–425
Chambat P, Denoyers J, Selmi TAS, Dejour D, Denoyers J (2000) Varus tibial osteotomy. Oper Tech Sports Med 8:44–47
Coventry B (1985) Current upper tibial concepts review for osteoarthritis. J Bone Jt Surg 67–A:1136–1140
Coventry B (1987) Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee. J Bone Jt Surg 69-A:32–38
van Egmond N, Stolwijk N, van Heerwaarden R, van Kampen A, Keijsers NLW (2017) Gait analysis before and after corrective osteotomy in patients with knee osteoarthritis and a valgus deformity. Knee Surg Sports Traumatol Arthrosc 25(9):2904–2913
Eshuis R, Lentjes GW, Tegner Y, Wolterbeek N, Veen MR (2016) Dutch translation and cross-cultural adaptation of the Lysholm score and Tegner activity scale for patients with anterior cruciate ligament injuries. J Orthop Sports Phys Ther 46:976–983
de Groot IB, Favejee MM, Reijman M, Verhaar J, Terwee N CB (2008) The Dutch version of the Knee Injury and Osteoarthritis Outcome Score: a validation study. Health Qual Life Outcomes 6:16
Haverkamp D, Sierevelt IN, Breugem SJM, Lohuis K, Blankevoort L, van Dijk CN (2006) Translation and validation of the Dutch version of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med 34:1680–1684
Haviv B, Bronak S, Thein R, Thein R (2013) The results of corrective osteotomy for valgus arthritic knees. Knee Surg Sports Traumatol Arthrosc 21(1):49–56
van Heerwaarden RJ, Wagenaar F, Hofmann S (2004) Double osteotomies of the femur and the tibia. In: Lobenhoffer et al (eds) Osteotomies around the knee, 1st edn. Thieme, Stuttgart, pp 167–184
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29:600–613
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004) Reliability, validity, and responsiveness of the Lysholm knee scale for various chondral disorders of the knee. J Bone Jt Surg Am 86-A:1139–1145
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L (2007) The anatomy of the medial part of the knee. J Bone Jt Surg Am 89:2000–2010
Van Lieshout WAM, Martijn CD, van Ginneken BJT, van Heerwaarden RJ (2018) Medial collateral ligament laxity in valgus knee deformity before and after medial closing wedge high tibial osteotomy. Instrumented laxity measurements and patient reported outcome. J Exp Orthop. https://doi.org/10.1186/s40634-018-0164-2
Marti RK, Verhagen RAW, Kerkhoffs GMMJ, Moojen TM (2001) Proximal tibial varus osteotomy: indications, technique, and five to twenty-one-year results. J Bone Jt Surg Ser A 83:164–170
Mirouse G, Dubory A, Roubineau F, Poignard A, Hernigou P, Allain J, Flouzat Lachaniette CH (2017) Failure of high tibial varus osteotomy for lateral tibio-femoral osteoarthritis with < 10° of valgus: outcomes in 19 patients. Orthop Traumatol Surg Res 103:953–958
Paley D (2002) Principles of deformity correction. Springer, Berlin
Puddu G, Cipolla M, Cerullo G, Franco V, Giannì E (2010) Which osteotomy for a valgus knee? Int Orthop 34:239–247
Roos EM, Toksvig-Larsen S (2003) Knee injury and Osteoarthritis Outcome Score (KOOS)—validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1:17
Shoji H, Insall J (1973) High tibial osteotomy for osteoarthritis of the knee with valgus deformity. J Bone Jt Surg Am U S 55:963–973
W-Dahl A, Robertsson O, Lohmander LS (2012) High tibial osteotomy in Sweden, 1998–2007. Acta Orthop 83:1–5
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
WvL was responsible for data collection and interpretation, assisted in the study design and drafted the manuscript; BvG conducted the telephone calls, was responsible for data acquisition and performed the statistical analysis and wrote the method and results section; GK revised the manuscript and assisted with study design and result interpretations; RvH was the project supervisor and responsible for the study design, performed most of the surgeries, assisted in writing and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The first author has received a contribution from the Marti Keuning-Eckhardt Stichting (Stichting MKE) to conduct this research. None of the other authors have anything to declare.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
van Lieshout, W.A.M., van Ginneken, B.J.T., Kerkhoffs, G.M.M.J. et al. Medial closing wedge high tibial osteotomy for valgus tibial deformities: good clinical results and survival with a mean 4.5 years of follow-up in 113 patients. Knee Surg Sports Traumatol Arthrosc 28, 2798–2807 (2020). https://doi.org/10.1007/s00167-019-05480-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05480-9