Abstract
Purpose
Clinicians have different techniques and varying levels of experience with the pivot shift test, introducing variability into its performance. The purpose of this study was to evaluate the influence of teaching and repetition on the success rate and anterior translation of the lateral knee compartment during the pivot shift test in a cadaveric ACL injury model.
Methods
Twenty-five participants (five each of medical students, orthopaedic surgery residents, physical therapists, athletic trainers, sports medicine fellows) were recruited and a senior orthopaedic surgeon served as gold standard examiner. Each participant performed 20 pivot shift tests on lower extremity cadaveric specimens with ACL deficiency and lateral meniscectomy: 5 prior to education (baseline), 10 after watching an instructional video (passive teaching), and 5 after an interactive education session (active teaching). The anterior translation of the lateral knee compartment was recorded during each pivot shift test using electromagnetic tracking system.
Results
For medical students and orthopaedic surgery residents, significant improvement in success rate was found when compared to baseline (12% and 24%, respectively) after both passive (36% and 60%, respectively) and active teaching (52% and 72%, respectively) (p < 0.5). Medical students and residents were the only participants that independently achieved significant increases in anterior translation of the lateral knee compartment, each tripling the respective baseline value (p < 0.5). In the entire study population, significant increases in anterior translation of the lateral knee compartment and success rate of the pivot shift test were seen with continuous repetition (p < 0.5). However, the standard deviation of anterior translation of the lateral knee compartment was more than twice the gold standard examiner’s standard deviation, indicating a high degree of variability.
Conclusion
Teaching of the pivot shift test plays a major role in the development of a proper technique. However, variability persisted despite teaching and repetition. New methods may be needed to improve the teaching of the pivot shift test.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pivot shift test is a highly specific examination for rotatory knee laxity in patients with anterior cruciate ligament (ACL) deficiency and the grade of the pivot shift test is a commonly used outcome measure to evaluate knee function before and after ACL reconstruction [1,2,3]. During the pivot shift test, the knee is continuously flexed while internal torque and gentle valgus stress are applied by the examiner, leading to anterior subluxation of the lateral tibial plateau and a subsequent palpable reduction [4, 5]. Traditionally, the laxity of the knee during the pivot shift test is graded subjectively based on the examiner’s perception of the translation during the reduction event as either a glide (grade 1), a clunk (grade 2), or a gross clunk (grade 3) [6,7,8,9]. Recently, this subjective grading has been supplemented by methodologies that enable clinicians to objectively quantify the pivot shift test [10]. For example, some devices quantify the pivot shift test by measuring the acceleration of the tibia using an inertial sensor or measuring the magnitude of the anterior translation of the lateral knee compartment during the reduction event [11, 12].
Regardless of the methodology, all subjective and objective grading systems require a repeatable pivot shift test technique to compare knee laxity over time, across patients, and among clinicians. For proper grading, it is important to achieve an appropriate amount of anterior translation of the lateral knee compartment during the pivot shift test. However, the complexity of the pivot shift test causes a high degree of intra- and inter-examiner variability and makes the pivot shift test dependent on the experience and technique of the examiner [13, 14]. Use of a standardized technique has been shown to help provide more consistent quantitative results among experienced senior orthopaedic surgeons, but there is a lack of literature regarding the ability of unexperienced clinicians to learn the pivot shift test [4].
In the clinical setting, people commonly learn this complex clinical examination through instructional videos or textbooks (passive teaching) or through hands-on teaching (active teaching), which results in variability of techniques among different clinicians and limits comparisons between studies. Teaching this examination to other types of clinicians involved in the process of rehabilitation, such as physical therapists, could potentially enable a longitudinal monitoring of rotatory laxity—pre-operatively, intraoperatively, and during the rehabilitation process. Thus, the objective of this study is to examine the effect of teaching and repetition on the success rate of the pivot shift test and on the amount of anterior translation of the lateral knee compartment during the pivot shift test. It was hypothesized that both teaching and repetition will lead to significant increases of the success rate and anterior translation of the lateral knee compartment in all participating groups of clinicians due to use of the proper technique of the pivot shift test with additional instruction and practice. Furthermore, it was hypothesized that participants with less clinical experience will have significantly higher increases in success rate and anterior translation of the lateral compartment compared to more experienced examiners. The results of this study are of clinical significance as a reproducible pivot shift technique is essential for determining the type of surgical intervention (i.e. need for extra-articular lateral tenodesis) and the longitudinal assessment of rotatory laxity in the follow-up.
Materials and methods
Twenty-five subjects (five each of medical students, orthopaedic residents, physical therapists, athletic trainers, and sports medicine fellows) were recruited for the study protocol. Additionally, one senior orthopaedic surgeon served as the gold standard. Two cadaveric fresh-frozen full lower extremity specimens were utilized for the performance of the pivot shift tests. The specimens were thawed for 36 h at room temperature prior to starting the testing protocol. Subsequently, a thorough manual, radiographic, and arthroscopic examination was conducted to exclude specimens with bony or ligamentous abnormalities. After the completion of this evaluation, the ACL and the lateral meniscus were resected arthroscopically to enable a positive pivot shift test. Two specimens were used for this study to ensure consistent biomechanical properties of the tissue since testing was completed over several consecutive days. Testing on each of the specimens was conducted within 48 h, on two consecutive testing days. In between data acquisition, the specimens were stored in a refrigerator to decelerate tissue degradation. Regular control of the ligamentous laxity was performed to rule out that the repetitive mechanical stress of the pivot shift negatively affected the biomechanical properties of the specimens. While the participants performed all of their trials on one of the specimens, the senior orthopaedic surgeon performed ten pivot shift tests on both full lower extremity specimens to establish the standard for comparison purposes.
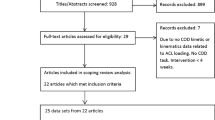
The experimental protocol (Fig. 1) began with an evaluation of each subject’s baseline knowledge about the pivot shift test using a questionnaire, consisting of four questions about the technique utilized during the pivot shift test:
-
What are the three essential steps of the pivot shift test?
-
Which compartment of the knee is mainly involved in the subluxation occurring during the pivot shift test?
-
During the pivot shift test, what is happening at the joint surface when the “clunk” occurs? (indicating that the knee is unstable)
-
If you are examining a left knee for instability with the pivot shift test, which hand do you hold the lower leg with?
Each subject performed five pivot shift tests using their baseline technique on the injured knee, while the six degrees of freedom kinematics were recorded. Then, each subject received passive teaching in the form of an instructional video about the pivot shift test [15]. After passive teaching, each subject completed the same questionnaire again to assess if the participants expanded their knowledge about the pivot shift test through passive teaching. Additionally, each subject performed another ten pivot shift tests on the ACL deficient knee using the standardized technique shown in the instructional video, while six degrees of freedom kinematics were recorded. Afterwards, each subject was individually taught by two experienced examiners with expertise in the pivot shift test how his/her technique could be improved to match the technique shown in the passive teaching video using a hands-on approach (active teaching). After active teaching, each subject performed another five pivot shift tests on the injured knee, while six degrees of freedom kinematics were recorded.
An electromagnetic tracking system (Nest of Birds, Ascension Technology, Shelburne VT) was used to obtain the six degrees of freedom kinematics of the pivot shift test. This system utilized three electromagnetic sensors, one fixed on the femur, one on the tibia, and one on a stylus, to digitize anatomical landmarks on the femur and tibia. The accuracy of this system was 0.5 mm for translation and 0.5° for rotation. The anterior translation of the lateral knee compartment was measured using previously described methods [16,17,18].
To determine which pivot shift tests were successful, quantitative criteria were developed. For each time point, \(({t_i},~{x_i})\) an extended slope \({s_i}=\frac{{{x_{i+2}} - {x_{i - 1}}}}{{{t_{i+2}} - {t_{i - 1}}}}\) was calculated to compensate for noise in the slope of the anterior translation of the lateral knee compartment as a function of time (see Fig. 2). The maximum anterior translation of lateral knee compartment, which marks the maximal subluxation of the tibia and the start of the reduction event, and the minimum anterior translation of lateral knee compartment, which marks the end of the reduction event and the pivot shift test, were automatically selected based on a conversion in the algebraic sign of the extended slope. The difference between maximum and minimum anterior translation of the lateral knee compartment, representing the translation of the lateral knee compartment during the reduction event, was calculated to quantify the pivot shift test. The pivot shift test was graded as negative if no conversion in the algebraic sign was present. Pivot shift tests were defined as positive if the recorded anterior translation of the lateral knee compartment during the reduction event was higher than the minimum reduction translation, which was defined as the square root of the standard deviation of anterior translation of the lateral knee compartment during the reduction event across all subjects. The success rate was calculated to be the number of positive pivot shift tests as defined by the criteria above divided by total number of pivot shift tests performed. The anterior translation of the lateral knee compartment was normalized using the average anterior translation of the lateral knee compartment of the gold standard examiner on the corresponding specimen and reported as a percentage.
Selection of the reduction event during the pivot shift test. First the slope of the anterior translation of the lateral compartment was calculated for each time point \(({t_i},{x_i})\) (grey mark) based on the values \(({t_{i - 1}},{x_{i - 1}})\) and \(({t_{i+2}},{x_{i+2}})\) (white marks). The start of the reduction event of the pivot shift and the end of the reduction event of the pivot shift were determined using the conversion of the algebraic sign at the maximum and minimum of the curve as selection criteria. The difference in anterior translation of the lateral knee compartment between the start and the end of the reduction event was used for the quantification of the pivot shift test
Approval for this study was obtained from the Institutional Review Board of the University of Pittsburgh and the Committee for Oversight in Research Involving Decedents (CORID) in accordance with the ethical standards of the Declaration of Helsinki (1964) and its later amendments (PRO15060142).
Statistical analysis
Data analysis was performed using Microsoft Excel 2013 and SPSS (version 20.0, SPSS Inc., Chicago, USA). T tests were used to analyze the results of the questionnaires before and after the instructional video. ANOVAs were used to compare the anterior translation of the lateral knee compartment within each group before and after each teaching session. Fischer’s exact tests were applied to analyze each group’s success rates of the pivot shift test (positive vs. negative pivot shift tests) before and after each teaching session. Pearson’s correlation coefficient was used to evaluate the effect of repetition on the success rate of the pivot shift test within each education and across the entire population. When comparing the trial-by-trial development of the entire study population, a one-sided t test was used to analyze the anterior translation of the lateral knee compartment values before and after teaching. The sample size of five participants per discipline was calculated based on a preliminary test using an a priori power analysis (G*Power) to establish 80% power. As the pretest revealed a high degree of variability, 20 repetitions per participants were chosen to allow for unsuccessful attempts as well as simultaneously examine the effect of repetition on the pivot shift examination. Statistical significance was set at p < 0.05.
Results
Six degrees of freedom kinematics were recorded for the 500 pivot shift tests performed by the participating clinicians (20 for each of the 25 participants) and the 20 pivot shift tests performed by the senior orthopaedic surgeon (10 on each of the specimens). A total of 190 pivot shift tests were performed on the first specimen and 330 on the second specimen. Of the 500 pivot shift tests performed, 319 (61.3%) pivot shift tests were graded as negative pivot shift tests based on the exclusion criteria. The remaining successful pivot shift tests were used for the analysis of the changes in anterior translation of the lateral knee compartment with teaching and repetition.
The results of the questionnaires showed that all subgroups had baseline knowledge about the pivot shift test with 75% correct answers on average across all subjects and at least 50% correct answers for each participant before watching the instructional video. Moreover, the second questionnaire showed the positive impact of passive teaching on theoretical knowledge about the pivot shift test with an increase in the percentage of correct answers in all groups. In the entire study population, a significant increase of the theoretical knowledge was noted with 89% correct answers after passive teaching compared to 75% correct answers at baseline (p < 0.05).
Significant improvements in success rate compared to baseline were noted after both passive and active teaching only for medical students and orthopaedic surgery residents (p < 0.05) (Fig. 3). The medical students had a baseline success rate of 12%, which increased to 36% after passive teaching and to 52% after active teaching, while the orthopaedic surgery residents had a baseline success rate of 24%, which increased to 60% after passive teaching and to 72% after active teaching. In addition, only medical students and orthopaedic surgery residents showed a significant increase in the success rate with continuous repetition (p < 0.05). Athletic trainers, physical therapists, and sports medicine fellows demonstrated no significant change in success rate after both passive and active teaching, and with continuous repetition. Among all subjects, the success rate after passive and after active teaching (41%) was significantly higher than the baseline success rate (26%, p < 0.05). When looking at the overall success rate of the pivot shift test of all subjects in the study (Fig. 4), a continuous increase in the success rate with more repetitions was noted (r = 0.424, p < 0.05). However, variability persisted within all groups and throughout the entire study protocol as seen on the high percentage of negative pivot shift tests despite passive and active teaching.
Success rate of the pivot shift test with repetition. Influence of teaching and repetition on the success rate of the pivot shift test. Each data point represents the average of all 25 participants for that trial. Vertical lines illustrate the timing of passive and active teaching. The dashed line shows a linear regression trendline for the effect of repetition. Repetition continuously increased the success rate of the pivot shift test, but the teaching sessions did not produce a step-wise increase in success rate or increase it over 50%
All groups improved their anterior translation of the lateral knee compartment after passive and active teaching by generating anterior translation values with similar magnitudes as the gold standard examiner’s average (illustrated by the dashed line in Fig. 5). Sports medicine fellows achieved anterior translation of the lateral knee compartment values comparable to the gold standard examiner even before teaching. In the entire study population, incremental increases in anterior translation of the lateral compartment were noted with the introduction of passive and active teaching (p < 0.05) (Fig. 6). However, despite teaching, a large amount of variability persisted in the anterior translation of the lateral knee compartment within each group, recognizable by the high standard deviation of anterior translation of the lateral knee compartment of all participants, being more than twice as high as the gold standard examiner’s standard deviation. As a result, only medical students and orthopaedic surgery residents achieved statistically significant increases in anterior translation of lateral knee compartment after teaching (p < 0.05). Variability of the anterior translation of the lateral knee compartment was only weakly associated with clinical experience, as an analysis of variance revealed that only 21.7% of the variability of the anterior translation of the lateral compartment was accounted for by group membership.
Magnitude of the reduction event during the pivot shift test after teaching in each group. Percentage of anterior translation of the lateral knee compartment of the gold standard examiner’s average for each group before and after passive and active teaching. The dashed line shows the gold standard examiner’s average anterior translation of the lateral knee compartment. Ant. anterior, Lat. lateral. *p < 0.05
Magnitude of the reduction event pivot shift test with repetition and teaching in the entire study population. Influence of teaching and repetition on the percentage anterior translation of the lateral knee compartment. Each data point represents the average of all 25 participants at that trial. Vertical lines illustrate the timing of passive and active teaching. Incremental improvements were noted after each of the teaching sessions as shown by the dashed line. Ant. anterior, Lat. lateral. *p < 0.05
Discussion
An important finding of this study was that passive and active teaching effectively increased the anterior translation of the lateral knee compartment during the pivot shift test to values close to those of the gold standard examiner. In fact, after only passive teaching, all groups were able to generate anterior translation values comparable to those of the senior orthopaedic surgeon serving as gold standard examiner. Additionally, repetition seemed to influence the success rate of the pivot shift test, leading to a significant increase in the success rate with continuous repetition in only medical students and orthopaedic surgery residents.
The analysis within each group revealed that only the medical students and orthopaedic surgery residents had significant increases in success rate and anterior translation of the lateral knee compartment after teaching. Similar to medical students and orthopaedic surgery residents, athletic trainers and physical therapists also had low baseline values of anterior translation, but subsequently did not improve significantly. Sports medicine fellows had a higher baseline value and achieved anterior translation of the lateral knee compartment values comparable to the gold standard examiner even before teaching. This suggests that level of training might have an effect on the degree of influence that teaching has on the success and technique of the pivot shift test. The fact that the study population is diverse, with clinicians who have varying levels of training with the pivot shift test, could be a potential explanation for the high variance of the anterior translation of the lateral knee compartment. However, only 21.7% of the overall variability in anterior translation of the lateral knee compartment was accounted for by group membership.
This study showed that passive teaching was able to improve the theoretical knowledge about the pivot shift test based on assessment through a questionnaire. A similar effect of written and video instruction (passive teaching) on the theoretical knowledge about a screening musculoskeletal examination has been shown in a previous study [19]. Additionally, small group teaching (active teaching) was evaluated and found to be superior to passive teaching in the actual performance of the clinical examination despite no differences in theoretical knowledge [19]. Contrary to these findings, active teaching with individualized feedback in this study did not significantly improve the variability of anterior translation of the lateral knee compartment or the success rate of the pivot shift test compared to the passive teaching group.
Continuous repetition led to a significant increase in the success rate when including all subjects of the study and, in particular, medical students and orthopaedic surgery residents. This finding indicates that beside passive and active teaching, a regular performance of the pivot shift test, each with a sufficient number of repetitions, might be needed to achieve a repeatable technique with a adequate success rate. However, in terms of learning clinical examinations, there is a lack of literature examining the effect of repetition on the actual performance of the clinician and further research is needed to evaluate how many repetitions and how frequent clinicians need to perform this examination to effectively learn examining skills. Having the ability to perform a reproducible pivot shift is essential for determining the type of surgical intervention, for example, if an additional extra-articular lateral tenodesis is needed, as well as for the longitudinal monitoring of rotatory laxity in the follow-up process. This study constitutes a first step to optimize the learnability of the pivot shift examination to improve the diagnostic skills of prospective clinicians.
One limitation of this study design is that it does not allow for a direct comparison between the effects of passive and active teaching so it remains unclear if passive teaching was actually equivalent to active teaching. It would be an important comparison since there have been several studies that have found similar results to those of the aforementioned study [19]. For example, a recent study evaluating the education of critical care fellows on mechanical ventilation by comparing a guided self-directed learning group with a group that additionally received hands-on tutoring found significantly higher improvements when the fellows received hands-on tutoring [20]. One possible reason for the lack of difference between active and passive teaching in this study could be the low number (five) of pivot shift tests performed after subjects underwent active teaching. This might not be a sufficient number of repetitions to improve the muscle memory for the complex manoeuvers after active teaching. The effectiveness of passive teaching compared to active teaching would be an area to explore further with a study design that directly compares the two methods independently and provides a sufficient number of repetitions after each teaching session.
Conclusion
Both teaching and repetition contribute to slightly improving the success rate of the pivot shift test, but only teaching contributes to increasing the magnitude of the anterior translation of the lateral knee compartment. Future studies will focus on determining the effects of passive and active teaching methods on learning of the proper technique of the pivot shift test.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ANOVA:
-
Analysis of variance
References
Ayeni OR, Chahal M, Tran MN, Sprague S (2012) Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 20:767–777
Kieser C, Junker C (1986) The reliability of the lateral pivot-shift as a clinical sign of anterior cruciate insufficiency. In: Trickey EL, Hertel P (eds) Surgery and arthroscopy of the knee. Springer, Berlin, Heidelberg
Ostrowski JA (2006) Accuracy of 3 diagnostic tests for anterior cruciate ligament tears. J Athl Train Natl Athl Train Assoc 41:120–121
Hoshino Y, Araujo P, Ahlden M, Moore CG, Kuroda R, Zaffagnini S, Karlsson J, Fu FH, Musahl V (2012) Standardized pivot shift test improves measurement accuracy. Knee Surg Sports Traumatol Arthrosc 20:732–736
Losee RE (1983) Concepts of the pivot shift. Clin Orthop Relat Res 172:45–51
Benjaminse A, Gokeler A, van der Schans CP (2006) Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther 36:267–288
Irrgang JJ, Ho H, Harner CD, Fu FH (1998) Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6:107–114
Jakob RP, Stäubli HU, Deland JT (1987) Grading the pivot shift. Objective tests with implications for treatment. J Bone Jt Surg Br 69:294–299
Musahl V, Hoshino Y, Ahlden M, Araujo P, Irrgang JJ, Zaffagnini S, Karlsson J, Fu FH (2012) The pivot shift: a global user guide. Knee Surg Sports Traumatol Arthrosc 20:724–731
Lopomo N, Zaffagnini S, Amis AA (2013) Quantifying the pivot shift test: a systematic review. Knee Surg Sports Traumatol Arthrosc 21:767–783
Muller B, Hofbauer M, Rahnemai-Azar AA, Wolf M, Araki D, Hoshino Y, Araujo P, Debski RE, Irrgang JJ, Fu FH, Musahl V (2016) Development of computer tablet software for clinical quantification of lateral knee compartment translation during the pivot shift test. Comput Methods Biomech Biomed Eng 19:217–228
Zaffagnini S, Lopomo N, Signorelli C, Marcheggiani Muccioli GM, Bonanzinga T, Grassi A, Raggi F, Visani A, Marcacci M (2014) Inertial sensors to quantify the pivot shift test in the treatment of anterior cruciate ligament injury. Joints 2:124–129
Noyes FR, Grood ES, Cummings JF, Wroble RR (1991) An analysis of the pivot shift phenomenon. The knee motions and subluxations induced by different examiners. Am J Sports Med 19:148–155
Peeler J, Leiter J, MacDonald P (2010) Accuracy and reliability of anterior cruciate ligament clinical examination in a multidisciplinary sports medicine setting. Clin J Sport Med 20:80–85
Instructional video about the pivot shift exam. https://www.youtube.com/watch?v=kOZA2xkiWdY. Accessed 1 Feb 2019
Bedi A, Musahl V, Lane C, Citak M, Warren RF, Pearle AD (2010) Lateral compartment translation predicts the grade of pivot shift: a cadaveric and clinical analysis. Knee Surg Sport Traumatol Arthrosc 18:1269–1276
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105:136–144
Kuroda R, Hoshino Y (2016) Electromagnetic tracking of the pivot-shift. Curr Rev Musculoskelet Med 9:164–169
Lawry GV, Schuldt SS, Kreiter CD, Densen P, Albanese MA (1999) Teaching a screening musculoskeletal examination: a randomized, controlled trial of different instructional methods. Acad Med 74:199–201
Ramar K, De Moraes AG, Selim B, Holets S, Oeckler R (2016) Effectiveness of hands-on tutoring and guided self-directed learning versus self-directed learning alone to educate critical care fellows on mechanical ventilation—a pilot project. Med Educ Online 21:32727
Funding
There was no external source of funding for this study.
Author information
Authors and Affiliations
Contributions
JHN performed acquisition, interpretation, and analysis of data, and drafted the original manuscript. NKP, JPZ, and CIM performed acquisition, interpretation, and analysis of data. RED and VM edited the original manuscript, assisted with the interpretation and analysis of data, and conceived and designed the original project.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this study confirm that they have no conflicts of interest related to this study.
Ethical approval
Prior to the start of this study, approval was obtained from the Institutional Review Board of the University of Pittsburgh and the Committee for Oversight in Research Involving Decedents (CORID) in accordance with the ethical standards of the Declaration of Helsinki (1964) and its later amendments (PRO15060142).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Naendrup, JH., Patel, N.K., Zlotnicki, J.P. et al. Education and repetition improve success rate and quantitative measures of the pivot shift test. Knee Surg Sports Traumatol Arthrosc 27, 3418–3425 (2019). https://doi.org/10.1007/s00167-019-05370-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05370-0