Abstract
Purpose
This study evaluated the clinical efficacy of continuous passive motion (CPM) following knee arthroplasty and determined the predictors of effect sizes of range of motion (ROM) and functional outcomes in patients with knee arthritis.
Methods
A comprehensive electronic database search was performed for randomized controlled trials (RCTs), without publication year or language restrictions. The included RCTs were analyzed through meta-analysis and risk of bias assessment. Study methodological quality (MQ) was assessed using the Physiotherapy Evidence Database (PEDro) scale. Inverse-variance weighted univariate and multivariate metaregression analyses were performed to determine the predictors of treatment outcomes.
Results
A total of 77 RCTs with PEDro scores ranging from 6/10 to 8/10 were included. Meta-analyses revealed an overall significant favorable effect of CPM on treatment success rates [odds ratio: 3.64, 95% confidence interval (CI) 2.21–6.00]. Significant immediate [postoperative day 14; standard mean difference (SMD): 1.06; 95% CI 0.61–1.51] and short-term (3-month follow-up; SMD: 0.80; 95% CI 0.45–1.15) effects on knee ROM and a long-term effect on function (12-month follow-up; SMD: 1.08; 95% CI 0.28–1.89) were observed. The preoperative ROM, postoperative day of CPM initiation, daily ROM increment, and total application days were significant independent predictors of CPM efficacy.
Conclusion
Early CPM initiation with rapid progress over a long duration of CPM application predicts higher treatment effect on knee ROM and function. The results were based on a moderate level of evidence, with good MQ and potential blinding biases in the included RCTs. An aggressive protocol of CPM has clinically relevant beneficial short-term and long-term effects on postoperative outcomes.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
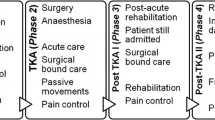
Continuous passive motion (CPM) immediately after arthroplastic surgery is primarily advocated for its potential benefits on knee ROM and acute stay conditions [23, 24, 35]. The effects of CPM on postoperative outcomes have been investigated through several systemic reviews and meta-analyses [15, 17, 30, 36, 41, 42, 44]. Despite controversies, CPM has been used as an adjunct therapy to the standard postoperative rehabilitation regimen, because it offers short-term benefits during acute stay [6, 17, 30, 36, 44]; however, its long-term effectiveness during postacute follow-up remains uncertain [15, 17, 30].
Most systemic reviews and meta-analyses regarding the effectiveness of CPM have included study selection or inclusion criteria with restrictions on language [15, 30, 36, 41, 42] or publication time [30, 44]. In addition, only a few reviewers have excluded studies with low methodological quality [36, 44]. Furthermore, the majority of the articles included in most systemic reviews were published in American or European countries, and few trials with Asian populations have been included [15, 17, 30, 36, 41, 42, 44]; it remains unclear whether countries or patient populations influence the effects of CPM therapy. Thus, the results reported in previous systematic reviews [40] may be biased.
In clinical practice, various prescriptions of CPM are used with multiple application parameters. CPM efficacy may depend on its application protocol, and several studies have compared the effectiveness of various CPM parameters, including the CPM initiation on the postoperative day (POD), the initial ROM (i.e., the flexion arc of motion) in the CPM device, daily increment in ROM, daily usage time, and the total application duration [2, 3, 8, 28, 29]. However, the influence of CPM parameters on treatment outcomes remains unclear [15, 17, 42]; furthermore, it remains unclear whether any parameter predicts the treatment effects on postoperative knee ROM and functional outcomes. Identification of the determinants of CPM treatment outcomes may enhance postoperative rehabilitation, because early maximum ROM regain is a clear prognostic factor for functional activity [33].
Using meta-analyses and subgroup analyses, this study was aimed to evaluate the clinical efficacy of CPM after knee arthroplasty in patients with arthritis and identified differences between populations. Furthermore, we performed metaregressions to identify the predictors of the effect of CPM therapy on postoperative outcomes during hospital stay and postacute follow-up. For clinical usefulness, determining the predictors of treatment effect of CPM following arthroplasty may help clinical practitioners establish optimal rehabilitation protocols and improve treatment efficiency for arthritis.
Materials and methods
This study was conducted in accordance with Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines [31] and was registered with the International Prospective Register of Systematic Reviews (PROSPERO, ID number: CRD42018099139). In this study, a comprehensive search for original research articles on the clinical efficacy of postoperative CPM following knee arthroplasty was conducted using the databases of Medline, PubMed, Excerpta Medica dataBASE, Cochrane Library Database, the Physiotherapy Evidence Database (PEDro), and China Academic Journals Full-Text Database and the search engine of Google Scholar. In addition, secondary sources were searched, including papers cited in the systemic review and meta-analysis studies. No restrictions were applied for the publication year and language. If English titles were not provided in non-English articles, they were translated to English using translation software (Ginger Software, Inc.). The search was restricted to published or in-press human studies. Two reviewers (CDL and YSC) independently searched for the articles, screened studies, and extracted data. Any disagreement between the reviewers were resolved through consensus, with other team members (HCC and SWH) acting as arbiters.
Search strategy
We used the following search terms in the Excerpta Medica dataBASE for identifying articles on CPM after knee arthroplasty and associated conditions: [“continuous passive motion” OR “CPM”] AND [“knee arthroplasty” OR “total knee replacement”] AND [“osteoarthritis” OR “gonarthritis” OR “rheumatoid arthritis”]. The detailed search formulas for each database are presented in online Table S1.
Study selection criteria
Articles were included if they fulfilled the following criteria: (1) the trial design was a randomized control trial (RCT) with an experimental group (i.e., CPM) and a comparison control group; (2) CPM was employed as the primary treatment; (3) the control group received regular postoperative nursing care (RNC) or underwent active exercise training (AET); (4) all patients had received a diagnosis of arthritis; (5) primary outcomes included knee joint ROM (active or passive knee flexion or the full range from extension to flexion) and pain measured using a quantifiable scale such as the visual analog scale (VAS); (6) secondary outcomes included patient-reported performance-based physical function; and (7) the following application parameters could be extracted: POD of CPM initiation, initial and final ROM set, daily ROM increment, daily application time, and application duration (i.e., total application days).
Articles meeting any of the following criteria were excluded: (1) the article evaluated an animal model, a case report, or case series; (2) the study in the article was a prospectively designed trial without a comparison group; (3) the full text of the article was unavailable; and (4) the study had fair or poor methodological quality, which was identified as a PEDro score of < 6/10 [32].
Data extraction and management
For the included studies, a data extraction sheet was developed and refined. An author (CDL) extracted the relevant data from the included studies, and another author (SWH) reviewed the extracted data. Any disagreement between the two authors was resolved through consensus. A third author (THL) was consulted if the disagreement persisted. The data of interest were group design, patient characteristics (population, age, sex, diagnosis, duration of disease onset), surgical conditions (e.g., prosthesis used and operated leg), CPM application parameters (e.g., POD of CPM initiation, initial setting in ROM, and daily increment in ROM), and follow-up period. The primary outcome of interest in the meta-analysis and metaregression was full knee ROM. If the trial did not report full knee ROM, it was estimated by subtracting knee flexion from knee extension, and knee extension was assumed as 0° when only knee flexion was reported. If the trial reported both active and passive ROM as well as knee flexion and extension, active ROM measures were included in the analyses. Pain severity was evaluated using either the VAS or a patient-reported scale. The functional scores used by the studies were Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Knee Society Score, and Hospital for Special Surgery Knee Scoring.
If any of the CPM application parameters were reported in terms of ranges, the medians of the ranges were used for analyses. If a study did not report any value and stated that the daily ROM increment during CPM therapy was determined according to patient tolerance, the daily ROM increment was assumed to be 15°; this value was chosen, because most of the previous protocols have used daily ROM increments of 5° to 20° [17, 30, 36, 42, 44] and it concurred with our previous results [26].
Assessment of methodological quality
The PEDro classification scale was employed to assess the methodological quality in the included trials [10]. Any disagreement between the two researchers (CDL and HCC) was resolved through consensus, and a third researcher (THL) was consulted if the disagreement could not be resolved. On the basis of the PEDro score, the methodological quality of the included RCTs was rated as high (≥ 7/10) or medium (< 7/10) [5].
Assessment of risk of bias
Two authors (CDL and HCC) independently assessed the risk of bias of the included studies using the Cochrane risk of bias tool [18, 20]. Any difference of opinion was resolved through consensus, and if necessary, any disagreement was resolved by a third reviewer (THL).
Statistical analysis
The effect sizes of CPM on the primary and secondary outcome measures were estimated by calculating the standard mean differences (SMDs) of the mean outcome between the treatment and control groups weighted by the inverse of the variation for every included study. SMD was used for meta-analysis when different scales were used to measure the same concept (e.g., pain and function score). In accordance with Cohen’s criteria [9], we categorized the magnitude of the SMD as trivial (d < 0.20), small (0.20 ≤ d < 0.60), moderate (0.60 ≤ d < 1.20), and large (d ≥ 1.20), which represent the categories modified by Hopkins [21]. If data were reported as a standard error or confidence interval (CI), they were recalculated algebraically from the trial data for imputing the sample mean and SD following the Cochrane Handbook for Systematic Reviews of Interventions [20]. The odds ratio (OR) with a 95% CI was estimated to indicate treatment success. Statistical heterogeneity of the included studies was assessed using the Q test (χ²) and I2 statistics, with high values indicating high heterogeneity [4]. If the study had more than one CPM or control intervention, each comparison was considered as an independent one for the meta-analyses [19]. Random-effects models were used for the meta-analyses. The effects of CPM on primary and secondary outcomes during hospital acute stay (≤ 2 weeks) and postacute follow-up (> 1 month) were separately analyzed. All meta-analyses were conducted using RevMan 5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark).
Subgroup analysis was performed on the basis of the population area, follow-up duration, methodological design, and quality level. The significance of all subgroup differences was assessed, and I2 statistics were computed to estimate the degree of subgroup variability. Potential publication bias was investigated through the visual inspection of a funnel plot [39] and through Egger’s regression asymmetry test [13].
Following a previously described method [5], we graded levels of evidence (LoE) for each outcome of interest in accordance with an evidence synthesis guideline [12] derived from van Tulder’s criteria [43] (Table 1).
To determinate the significant predictors of CPM efficacy for primary and secondary outcomes, inverse-variance weighted univariate and multivariate metaregression was performed using SPSS (version 17; IBM, Armonk, New York, USA). The mean age, body mass index, preoperative ROM as well as function, CPM application parameters, intervention design, control-group type, and follow-up duration were entered as covariates. First, univariate linear regression analyses were separately performed for each covariate at acute stay and postacute follow-up. To determine significant parameters, all CPM application parameters were then included in a stepwise multivariate regression analysis as covariates; the analysis was controlled for age, methodological design, preoperative ROM, and follow-up duration.
Results
Trial flow
The search yielded 916 articles (Fig. 1). After duplicate article removal and abstract screening, 160 eligible RCTs were identified for full-text assessment. The final sample comprised 77 RCTs, which included 93 comparisons between CPM group and the control group receiving RNC or AET. Characteristics of the included RCTs are presented in Table S2 and are summarized in Table 2.
Study characteristics
In total, 6038 patients with mean ages ranging from 52.0 to 74.2 years (overall mean age 65.7 years). These patients experienced symptoms for a mean duration of 110.2 months (range 4–264 months). The 77 RCTs included populations from Americas (709 patients), Asia (4395 patients), Europe (692 patients), and Oceania (144 patients) (Table 2).
CPM application parameters and treatment protocols are summarized in Table S3. All included RCTs applied a CPM intervention protocol that was initiated on POD 0–14 with an initial flexion ROM of 30°–90°, a daily ROM increment of 5°–20° as tolerable by patients, a daily application time of 0.5–12 h, and an intervention duration of 1–21 days.
Risk of bias in the included studies
A summary of the PEDro scores of the included RCTs is presented in Table 3. The individual PEDro scores and the rated quality levels are listed in Tables S4 and S2, respectively. Regarding the cumulative PEDro score, interrater reliability was acceptable, and the intraclass correlation coefficient was 0.97 (95% CI 0.95–0.98, P < 0.001). Of the included RCTs, 20.8% and 79.2% were classified as high and medium, respectively, with an overall mean (range/total) PEDro score of 6.4 (6–8/10). The risk of bias as assessed using the Cochrane Collaboration risk of bias tool (Fig. S1) was generally low or unclear. An overall summary of the risk of bias among the included RCTs is presented in Fig. 2. Selection, blinding, attrition, and agenda biases were considered the greatest potential risks of bias in the included RCTs.
Publication bias
Visual inspection of the funnel plots of ROM regain did not reveal substantial asymmetry (Fig. 3). In addition, Egger’s linear regression test provided no evidence of reporting bias among the trials (n.s.).
Publication bias plot. Funnel plot for effect size of knee ROM. The SMDs of knee ROM is plotted on the x-axis and standard error of SMD is plotted on the y-axis. The vertical dotted line indicates the mean value of the SMDs. Visual inspection of the funnel plot of the SMDs of pain score did not reveal substantial asymmetry. Egger’s linear regression test results indicated no evidence of reporting bias among the studies (n.s.). ROM range of motion, SMD standard mean difference
Meta-analyses
Treatment success rates and general outcomes
Treatment success rates (TSRs) for pain severity and global outcomes were mostly assessed using a Likert scale [7, 34] (Table S2). In the overall follow-up duration, the CPM group had a higher TSR than the non-CPM or active control group in the random-effects model (OR 3.64, P < 0.00001; LoE, moderate; Fig. S2).
Effect of CPM on postoperative pain
During acute stay, SMDs for pain reduction after CPM therapy were observed from POD 3 (SMD = − 0.87, P = 0.005) to POD 14 (SMD = − 0.70, P = 0.002) without significant heterogeneity among follow-up time frames (I2 = 0%) (Fig. S3), and an overall SMD of − 0.96 (P < 0.0001; LoE, moderate) favoring CPM was observed (Fig. S4).
During postacute follow-up, SMDs were observed only for short-term effects on pain reduction at 1-month follow-up (SMD = − 0.56, P = 0.01), favoring CPM; there was significant difference in heterogeneity among time frame subgroups (I2 = 64%) (Fig. S5). In the overall postacute follow-up duration, a significant SMD of − 0.64 favoring CPM (P = 0.005; LoE, moderate) was observed (Fig. S6).
Effect of CPM on range of motion
The meta-analysis for knee ROM during acute hospital stay revealed that irrespective of the application protocol and methodological design, CPM significantly improved knee ROM on POD 5 with an SMD of 0.75 (P = 0.001); similar results were observed on POD 10 and POD 14 (Fig. 4 and Table S5) and no significant heterogeneity among time frames was observed during acute stay (Fig. S7).
Forest plot of CPM therapy. Subgroup analyses for knee range of motion and functional recovery during the follow-up periods. Subgroup results plotted on the right-hand side indicate effects favoring CPM, and the combined effects are plotted using black diamonds. CI confidence interval, IV inverse variance, Random random-effects model, CPM continuous passive motion, POD postoperative day, PEDro Physiotherapy Evidence Database, RNC regular nursing care, AET active exercise training
During postacute follow-up, significant effects on knee ROM were only observed at 3-month follow-up (SMD = 0.80, P < 0.00001; LoE, moderate) (Fig. 4 and Table S6); however, no significant heterogeneity was observed among time frames (Fig. S8).
Effect of CPM on functional outcome
During acute stay, the effect of CPM on pooled functional scores was significant with an SMD of 1.59 (P = 0.03) on POD 5, and similar results were observed on POD 10 and POD 14, irrespective of the application protocol and methodological design (Fig. 4 and Table S5); however, significant differences were observed among time frames during acute stay (I2 = 79.2%) (Fig. S9).
Similar results were observed at 3-month (SMD = 0.86, P < 0.00001), 6-month (SMD = 1.02, P = 0.004), and 12-month (SMD = 1.08, P = 0.009) follow-up (Fig. 4 and Table S6); no significant differences were observed among time frames during postacute follow-up (I2 = 0%) (Fig. S10).
Subgroup analysis
During acute stay, all kinds of subgroups, except CPM intervention designs during all acute stay time frames, showed significant group differences in knee ROM as well as function (Fig. 4 and Table S5).
During postacute follow-up, significant differences in knee ROM effect were observed between the quality-level, population-area, control-type, and intervention-design subgroups at 3-month follow-up only (Fig. 4 and Table S6). At 3-month and 12-month follow-ups, significant differences in knee function effect was also observed in quality-level and population subgroups.
Metaregression analysis
Determinants of CPM efficacy
Young age (R2 = 18.9%, P = 0.001), low BMI (R2 = 30.3%, P = 0.04), and less preoperative ROM (R2 = 20.3%, P = 0.006) predicted greater effect sizes of knee ROM, pain, and functional outcomes during acute stay (Table S7); similar results were observed in knee ROM at postacute follow-up (Table S8). After all time frames were pooled, patients with a preoperative ROM of < 100°achieved a positive effect size of knee ROM following postoperative CPM therapy (β = −0.05; 95% CI − 0.07, − 0.03; P < 0.001) (Fig. 5).
Multivariate metaregression between preoperative ROM and effects of CPM on knee ROM. Each circle represents an independent comparison. The size of each circle is proportional to that study’s weight (inverse-variance weighted). The regression prediction is represented by the solid line for effect size (SMD) of knee ROM (β = −0.05; 95% CI − 0.07 to − 0.03; P < 0.001). Dotted lines represent the 95% CI. The metaregression model was adjusted for age, methodological design and quality, and follow-up time of each comparison. CPM continuous passive motion, ROM range of motion
Regarding CPM application parameters, a greater daily ROM increment (R2 = 47.5%, P < 0.001) and longer duration of CPM application (R2 = 18.3%, P = 0.003) significantly predicted larger effect sizes of postoperative ROM and functional recovery during acute stay (Table S7). At postacute follow-up, CPM application parameters had no effect on outcomes, except that an earlier POD of CPM initiation (R2 = 9.9%, P = 0.048) significantly predicted greater function recovery (Table S8). In addition, the POD of CPM initiation (R2 = 22.7%, P = 0.02) and daily ROM increment (R2 = 61.6%, P < 0.001) were also predictors of the effect size of treatment success.
The control type and CPM intervention design were significantly associated with the effect sizes of knee ROM at acute stay and postacute follow-up, respectively (Tables S7 and S8); similar results were observed in knee function. Follow-up duration was not associated with effect sizes of outcomes at acute stay and postacute follow-up (Tables S7 and S8).
CPM application parameters are associated with CPM efficacy
Four iterations of multiple linear regressions were performed for data analysis (Table 4). After controlling for patient characteristics and methodological designs, greater daily ROM increment and early POD of CPM initiation independently predicted greater effect sizes of postoperative knee ROM; similar results were found for function and treatment success.
Discussion
The meta-analyses provided statistically significant moderate evidence supporting that CPM increased the TSR, reduced pain, restored the knee ROM, and enhanced functional recovery, regardless of the follow-up duration, application parameters, and methodological design. We further identified that patient’s age and preoperative ROM significantly influenced the effect size of knee ROM after CPM therapy; in addition, CPM application parameters including POD of CPM initiation and daily ROM increment independently predicted effects on knee ROM and function.
In this meta-analysis, there was moderate evidence supporting that CPM exerted not only short-term benefits on postoperative knee ROM which is in line with previous systemic reviews [15, 36, 42, 44] but also long-term (12 months) effects on knee function which is conflicting to the previous results [17, 30, 41]. Unlike previous systemic reviews [15, 17, 30, 36, 41, 42, 44], in the current meta-analysis, RCTs without restrictions on publication year or language were selected, comparatively more RCTs with Asian populations were included, and RCTs with low methodological quality were excluded. The differences in the study selection and inclusion criteria may have contributed to the inconsistency between our results and previous systemic reviews.
Older age, knee stiffness, and obesity are risk factors for poor postoperative ROM [1, 14, 16, 22, 37] and rehabilitation outcomes during hospital acute stay and postacute follow-up [25,26,27]. In the present study, the results indicated that a lower preoperative ROM of < 100° can be predicted to achieve a positive effect size of knee ROM after CPM; this result is consistent with a previous study result indicating that patients with stiff knees before TKA surgery may experience greater gain in knee ROM postoperatively compared with those without knee stiffness [45].
The results of this meta-analysis revealed that CPM application parameters, particularly the POD of CPM initiation, daily ROM increment, and total days of application, were independent determinants of CPM clinical efficacy. Our findings are supported by previous studies [15] but are inconsistent with a recent Cochrane analysis [17]. It is believed that CPM demonstrated positive biologic effects on tissue healing, edema, hemarthrosis, and joint function [6, 35, 38]. Therefore, CPM may exert the greatest benefit with early initiation, greater progress in motion arc, and longer duration of application during acute hospital stay.
Several limitations of this study must be considered. First, although the data did not suggest substantial publication bias, heterogeneity was observed among the included RCTs, which may be attributed to the varying methodological designs and application protocols. Second, the nature of CPM intervention led to a high risk of blinding biases; however, all the included RCTs had good methodological quality (PEDro score ≥ 6). Finally, other confounding factors such as disease duration, surgery technique, prosthesis design, and postdischarge rehabilitation, which may have contributed to treatment efficacy [11], were not assessed when analyzing effect sizes of ROM and functional outcomes.
In this study, the clinically relevant results were identified that patient characteristics influenced the treatment effects of CPM therapy; in addition, an aggressive protocol of CPM application may predict greater treatment effects on postoperative outcomes. Such results may help clinical practitioners establish prompt and efficient rehabilitation protocols after knee arthroplasty in arthritis patients, especially for those with older age, higher BMI, and poor preoperative ROM.
Conclusion
In this study, we provided moderate evidence indicating that postoperative CPM therapy exerted significant short-term effects on TSR, pain, and knee ROM and a long-term effect on functional recovery in patients with arthritis. In addition, patient characteristics and CPM applications may influence treatment efficacy. Owing to potential biases (blinding biases) in the included RCTs of this study, we recommend that CPM should be cautiously applied to achieve favorable postoperative outcomes.
References
Alzahrani K, Gandhi R, Debeer J, Petruccelli D, Mahomed N (2011) Prevalence of clinically significant improvement following total knee replacement. J Rheumatol 38(4):753–759
Basso DM, Knapp L (1987) Comparison of two continuous passive motion protocols for patients with total knee implants. Phys Ther 67(3):360–363
Bennett LA, Brearley SC, Hart JA, Bailey MJ (2005) A comparison of 2 continuous passive motion protocols after total knee arthroplasty: a controlled and randomized study. J Arthroplasty 20(2):225–233
Bowden J, Tierney JF, Copas AJ, Burdett S (2011) Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalised Q statistics. BMC Med Res Methodol 11:41–53
Briani RV, Ferreira AS, Pazzinatto MF, Pappas E, De Oliveira Silva D, Azevedo FM (2018) What interventions can improve quality of life or psychosocial factors of individuals with knee osteoarthritis? A systematic review with meta-analysis of primary outcomes from randomised controlled trials. Br J Sports Med 52(16):1031–1038
Brosseau L, Milne S, Wells G, Tugwell P, Robinson V, Casimiro L et al (2004) Efficacy of continuous passive motion following total knee arthroplasty: a metaanalysis. J Rheumatol 31(11):2251–2264
Carifio J, Perla RJ (2007) Ten common misunderstandings, misconceptions, persistent myths and urban legends about likert. J Soc Sci 3(3):106–116
Chiarello CM, Gundersen L, O’Halloran T (1997) The effect of continuous passive motion duration and increment on range of motion in total knee arthroplasty patients. J Orthop Sports Phys Ther 25(2):119–127
Cohen J (1988) The analysis of variance. In: Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates, Hillsdale, pp 273–406
de Morton NA (2009) The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother 55(2):129–133
Dennis DA, Komistek RD, Scuderi GR, Zingde S (2007) Factors affecting flexion after total knee arthroplasty. Clin Orthop Relat Res 464:53–60
Dorrestijn O, Stevens M, Winters JC, van der Meer K, Diercks RL (2009) Conservative or surgical treatment for subacromial impingement syndrome? A systematic review. J Shoulder Elbow Surg 18(4):652–660
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Farahini H, Moghtadaei M, Bagheri A, Akbarian E (2012) Factors influencing range of motion after total knee arthroplasty. Iran Red Crescent Med J 14(7):417–421
Grella RJ (2008) Continuous passive motion following total knee arthroplasty: a useful adjunct to early mobilisation? Phys Ther Rev 13(4):269–279
Harvey IA, Barry K, Kirby SP, Johnson R, Elloy MA (1993) Factors affecting the range of movement of total knee arthroplasty. J Bone Joint Surg Br 75(6):950–955
Harvey LA, Brosseau L, Herbert RD (2014) Continuous passive motion following total knee arthroplasty in people with arthritis. Cochrane Database Syst Rev 2:CD004260
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD et al (2011) The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Higgins JPT, Deeks JJ, Altman DG (2011) Chapter 16: special topics in statistics. In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]: the cochrane collaboration. http://handbook.cochrane.org. Accessed Jun 04, 2018
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The cochrane collaboration. http://handbook.cochrane.org. Accessed Jun 04, 2018
Hopkins WG (2002) A scale of magnitudes for effect statistics a new view of statistics. http://sportsci.org/resource/stats/effectmag.html. Accessed Jun 04, 2018
Jarvenpaa J, Kettunen J, Kroger H, Miettinen H (2010) Obesity may impair the early outcome of total knee arthroplasty. Scand J Surg 99(1):45–49
Johnson DP, Eastwood DM (1992) Beneficial effects of continuous passive motion after total condylar knee arthroplasty. Ann R Coll Surg Engl 74(6):412–416
Lachiewicz PF (2000) The role of continuous passive motion after total knee arthroplasty. Clin Orthop Relat Res 380:144–150
Liao CD, Huang YC, Chiu YS, Liou TH (2017) Effect of body mass index on knee function outcome following continuous passive motion in patients with osteoarthritis after total knee replacement. Physiotherapy 103(3):266–275
Liao CD, Huang YC, Lin LF, Chiu YS, Tsai JC, Chen CL et al (2016) Continuous passive motion and its effects on knee flexion after total knee arthroplasty in patients with knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 24(8):2578–2586
Liao CD, Huang YC, Lin LF, Huang SW, Liou TH (2015) Body mass index and functional mobility outcome following early rehabilitation after a total knee replacement: a retrospective study in taiwan. Arthr Care Res (Hoboken) 67(6):799–808
MacDonald SJ, Bourne RB, Rorabeck CH, McCalden RW, Kramer J, Vaz M (2000) Prospective randomized clinical trial of continuous passive motion after total knee arthroplasty. Clin Orthop Relat Res (380):30–35
Maniar RN, Baviskar JV, Singhi T, Rathi SS (2012) To use or not to use continuous passive motion post-total knee arthroplasty presenting functional assessment results in early recovery. J Arthroplasty 27(2):193–200 e1
Mayo BS, Rodriguez-Mansilla J, Sanchez BG (2015) Recovery from total knee arthroplasty through continuous passive motion. An Sist Sanit Navar 38(2):297–310
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1
Moseley AM, Herbert RD, Sherrington C, Maher CG (2002) Evidence for physiotherapy practice: a survey of the physiotherapy evidence database (PEDro). Aust J Physiother 48(1):43–49
Naylor JM, Ko V, Rougellis S, Green N, Mittal R, Heard R et al (2012) Is discharge knee range of motion a useful and relevant clinical indicator after total knee replacement? Part 2. J Eval Clin Pract 18(3):652–658
Norman G (2010) Likert scales, levels of measurement and the “laws” of statistics. Adv Health Sci Educ Theory Pract 15(5):625–632
O’Driscoll SW, Giori NJ (2000) Continuous passive motion (CPM): theory and principles of clinical application. J Rehabil Res Dev 37(2):179–188
Postel JM, Thoumie P, Missaoui B, Biau D, Ribinik P, Revel M et al (2007) Continuous passive motion compared with intermittent mobilization after total knee arthroplasty. Elaboration of French clinical practice guidelines. Ann Readapt Med Phys 50(4):244–257
Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME (2003) Predicting range of motion after total knee arthroplasty. Clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am 85-A(7):1278–1285
Salter RB (1989) The biologic concept of continuous passive motion of synovial joints. The first 18 years of basic research and its clinical application. Clin Orthop Relat Res (242):12–25
Sedgwick P, Marston L (2015) How to read a funnel plot in a meta-analysis. BMJ 351:1–3
Sterne JAC, Egger M, Moher D (2011) Chapter 10: addressing reporting biases. In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The cochrane collaboration. http://www.handbook.cochrane.org. Accessed 12 Oct 2018
Tedesco D, Gori D, Desai KR, Asch S, Carroll IR, Curtin C et al (2017) Drug-free interventions to reduce pain or opioid consumption after total knee arthroplasty: a systematic review and meta-analysis. JAMA Surg 152(10):e172872
van Dijk HJD, Elvers JWH, Ruijter A, Oostendorp RAB (2007) Effect of continuous passive motion after total knee arthroplasty: a systematic review. Phys Singap 10(4):9–19
van Tulder M, Furlan A, Bombardier C, Bouter L (2003) Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976) 28(12):1290–1299
Viswanathan PKM (2010) Effect of continuous passive motion following total knee arthroplasty on knee range of motion and function: a systematic review. New Zeal J Physiother 38(3):14–22
Winemaker M, Rahman WA, Petruccelli D, de Beer J (2012) Preoperative knee stiffness and total knee arthroplasty outcomes. J Arthroplasty 27(8):1437–1441
Funding
This study was funded by grants from Taipei Medical University-Shuang Ho Hospital, Ministry of Health and Welfare, Taiwan (grant no. W107HCP-04). The funding source had no role in the design, implementation, data analysis and interpretation, or reporting of the study. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official view of the funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest related to the publication of this article.
Ethical approval
This study dealt with published data only, no ethical approval has been necessary since sensitive information has not been provided or utilized in this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liao, CD., Tsauo, JY., Huang, SW. et al. Preoperative range of motion and applications of continuous passive motion predict outcomes after knee arthroplasty in patients with arthritis. Knee Surg Sports Traumatol Arthrosc 27, 1259–1269 (2019). https://doi.org/10.1007/s00167-018-5257-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5257-z