Abstract
Purpose
The purpose of this study was to examine early radiological and clinical outcomes following minimally invasive double level osteotomy (DLO) procedure performed for osteoarthritic knees with severe varus deformity.
Methods
Twenty consecutive patients who underwent DLO for varus osteoarthritic knees were included in the study. All patients could be tracked for a minimum of 1 year. Periodical radiological and clinical evaluations were performed at 6 and 12 months after surgery. In the radiological assessment, the following parameters were measured on full-length weight-bearing radiographs both pre- and postoperatively: mechanical tibiofemoral angle (mTFA), mechanical lateral distal femoral angle (mLDFA), mechanical medial proximal tibial angle (mMPTA), and joint-line convergence angle (JLCA). In addition, subjective clinical results were evaluated using the Knee Injury and Osteoarthritis Outcome Score (KOOS) and the International Knee Documentation Committee (IKDC) Subjective Score.
Results
The mean age of the study population was 62.5 ± 6.8 years (range 45–76 years). In the radiological evaluation, the preoperative mTFA, mLDFA, mMPTA, and JLCA values averaged 13.5° ± 3.1° varus, 91.1° ± 1.4°, 82.3° ± 2.0°, and 5.8° ± 2.3°, respectively. At 6 and 12 months, all of the radiological parameters significantly improved and corrected to the values within normal range. In the clinical assessments at the follow-up evaluations, both the KOOS and IKDC subjective scores significantly improved from the preoperative values. No significant changes were noted between the 6 and 12-month results in the radiological and clinical assessments.
Conclusions
The minimally invasive DLO technique is a valuable surgical technique accomplishing restoration of physiologic knee joint alignment and orientation with significant improvement in patient-registered clinical outcomes in early postoperative evaluation. Although the follow-up period is still short, the excellent clinical and radiological outcomes shown in the present study support the efficacy of this procedure.
Level of evidence
Retrospective case series, Level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteotomy around the knee is a well-established and commonly employed surgical option for active patients with unicompartmental knee osteoarthritis [6, 28]. In recent years, a surgical technique has evolved with the introduction of minimally invasive biplanar opening wedge osteotomy with locking plate fixation, which enables early bone union and functional recovery [8, 18, 19, 29, 33]. Based on this progress, satisfactory mid-term outcomes have been reported for opening-wedge high tibial osteotomy (OWHTO) [11, 21]; however, limitations and shortcomings associated with correction in the proximal tibia alone have also been reported [3, 5, 22, 27, 34]. When correction of severe varus deformity is performed with HTO alone, a large wedge opening may result in non-physiologic lateral inclination of the joint line (Fig. 1). This situation can lead to several potential problems such as increased shear force at the cartilage [14, 20], femoral subluxation in full weight-bearing, overloading of the knee joint capsule, and difficulty in converting to total knee arthroplasty (TKA) [13, 15, 25, 26]. Considering the aforementioned shortcomings of HTO, double level osteotomy (DLO) has been introduced with the intention of restoring physiologic joint alignment and orientation for knees following correction of severe varus deformity (Fig. 2) [19, 32]. There have been several studies reporting the outcomes of DLO [2,3,4,5, 16, 27, 38]. In the studies published from the 1960s to the 1980s, the reported outcomes were rather discordant including both positive and negative results [2, 3, 5, 16, 32, 38]; however, those studies from the earlier days included both osteoarthritic and rheumatoid knees, and detailed consideration for knee alignment was not given in the surgical planning and procedure. Consequently, the clinical advantage of DLO over isolated HTO was not readily accepted in those days. Following 2000, the surgical concept of DLO has evolved for restoration of physiologic joint alignment and orientation. Babis et al. and Saragaglia et al. reported a satisfactory outcome of DLO with this concept [3, 27]. To date, however, there still is a paucity of evidence in literatures supporting the efficacy of DLO for restoration of normal anatomy and resultant symptomatic improvement. In addition, surgical technique has been further refined in the last decade with the introduction of the minimally invasive biplanar osteotomy technique and rigid fixation using a locking compression plate (LCP). Although these refinements in surgical technique are expected to improve the surgical outcome, results of the current DLO procedure have not been reported in literatures.
Preoperative planning of double level osteotomy using digital planning software. a Severe varus deformity of the right knee with combined deformity in both the femur and tibia (mLDFA: 90.6°, mMPTA: 81°, mTFA: − 16° varus). b Osteotomy simulation started with isolated OWHTO, and was considered for cases with an anticipated mMPTA of more than 95° or a wedge size of more than 15 mm. Simulation for OWHTO in this case shows that the wedge size was 17 mm and mMPTA was 97° when HTO alone was used to correct the varus deformity
In preoperative planning, mLDFA was set at 85°. a In the preoperative surgical simulation, the required wedge size was 12 mm with an mMPTA of 91.7°. b At the postoperative evaluation, measured mTFA, mLDFA, and MPTA were 1.2°, 85°, and 90.9°, respectively. OWHTO opening wedge high tibial osteotomy, mLDFA mechanical lateral distal femur angle, mMPTA mechanical medial proximal tibia angle, mTFA mechanical tibio-femoral angle
The purpose of this study, therefore, was to examine the early radiological and clinical outcomes following minimally invasive DLO performed with a modern concept and procedure. It was hypothesized that DLO, which is currently performed in our practice, would accomplish restoration of normal joint alignment and orientation with resultant clinical improvement.
Materials and methods
Twenty consecutive patients who underwent DLO in our institute during the study period from January 2014 to September 2016 were included in the study. The patient population comprised 5 males and 15 females with a mean age of 62.5 ± 6.8 years (range 45–76 years). All patients could be followed-up for at least 1 year after surgery, and the mean follow-up period was 20.7 ± 6.8 months (range 12–36 months).
Radiological and clinical evaluations were performed before surgery and at the follow-ups. In the radiological assessment, the following parameters were measured: mechanical tibiofemoral angle (mTFA), mechanical lateral distal femoral angle (mLDFA), mechanical medial proximal tibial angle (mMPTA), and joint-line convergence angle (JLCA) [9, 30]. Radiological measurement was performed on long-leg weight-bearing radiographs using digital planning software (mediCAD®, Hectec, Germany) [31]. In addition, validated patient-registered outcome measures, Knee Injury and Osteoarthritis Outcome Score (KOOS), and the score of the International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form were used for quantitative evaluation of clinical outcome.
Indications for a double level osteotomy and planning
In our unit, DLO is indicated when there is a combined deformity in the femur and the tibia in the active patient population and the patient wishes to retain high levels of activity or continue sitting on his or her heels (Japanese-style sitting). As a preoperative functional requirement, the level of pain should still allow the patient to have an active life style.
Radiological assessment and surgical planning were carried out on long-leg weight-bearing radiographs using digital planning software (mediCAD®, Hectec, Germany). In preoperative surgical planning, deformity correction by osteotomy was simulated to achieve restoration of physiologic joint alignment and orientation. Normal values for each of the radiological parameters reported in literatures are as follows: − 1° to 3° for mTFA, 85°–90° for mLDFA, 85°–90° for mMPTA, and 0°–2° for JLCA [23, 24]. Regarding the intended parameter values during the preoperative surgical simulation and planning of the osteotomy, the mTFA was set to 0.5°–1° (a slight valgus alignment), while mLDFA and mMPTA were set to 85° and 90°, respectively. Preoperatively, the surgical simulation was started with isolated OWHTO. If the predicted mMPTA in the surgical simulation was 95° or greater (or the wedge size was 15 mm or greater) for deformity correction with OWHTO alone, DLO was considered as a surgical option (Fig. 2) and surgical planning was conducted accordingly [20].
Surgical procedure
All surgeries were performed by the first author (H.N.) under general anaesthesia. Arthroscopy was performed prior to the osteotomy procedure. During arthroscopy, osteophytes in the notch were removed when present to improve extension. DLO was started with closing-wedge distal femoral osteotomy (CWDFO). A 4–5 cm longitudinal incision was made at the lateral side of the femur just above the femoral epicondyle according to the biplanar technique, which was developed by a working group from the Netherlands organized by R. van Heerwaarden [7, 10, 12]. Fixation of the osteotomy was accomplished following the minimally invasive plate osteosynthesis (MIPO) technique which was established by the same group [37] (Figs. 3, 4). The TomoFix medial distal femur (MDF) anatomical plate (DePuy Synthes, Solothurn, Switzerland) originally designed for the contralateral femur was bent according to the individual’s anatomy and positioned under the vastus lateralis muscle for osteotomy fixation. A drain was placed, and the layers were closed. At this stage, the alignment following CWDFO was checked under fluoroscopy for confirmation of correspondence with preoperative planning (Fig. 5). Afterwards, the osteotomy procedure was completed with subsequent OWHTO. The OWHTO procedure performed in this study followed the technique described by Staubli et al. and Lobenhoffer and Agneskirscner [19, 33]. After the osteotomy was made, the medial wedge was gradually opened while the limb alignment was monitored on fluoroscopy by checking the position of the alignment rod at the knee. Once the optimal location of the alignment rod at the knee corresponding to the preoperative planning was attained (with %MA of approximately 52–55%), the osteotomy site was fixed with that position. With the intent of improving the mechanical properties of the osteotomy site and enhancing bony union, a wedge-shaped bone substitute (ß-TCP: Osferion 60; Olympus Terumo Biomaterials, Tokyo, Japan) was inserted into the osteotomy gap in all of the cases included in this study [17, 35]. For fixation, a TomoFixTM medial high tibial (MHT) plate (DePuy Synthes, Solothurn, Switzerland) was placed anteromedially and the osteotomy site was fixed using lag screws (Figs. 6, 7). Finally, autogenous bony pieces and chips obtained from the femoral closing wedge and osteophytes were grafted into the tibial opening wedge to fill the remaining gap in the tibial opening wedge [1].
Preoperative assessment and surgical planning using digital planning software (a and b) and the intraoperative fluoroscopic image (c, white arrows indicate the mechanical axis). a The radiological parameters measured by digital planning software. b Surgical planning for DFO in the preoperative surgical simulation. c Intraoperative fluoroscopic image after DFO showing the mechanical axis (indicated by the metal alignment rod) passing through the same position as in the preoperative planning. DFO distal femoral osteotomy
Postoperative rehabilitation
The operated knee was not immobilized after surgery, and range of motion exercise was started as tolerated on the following day. Weight-bearing was not allowed for 3 weeks after surgery. Partial weight-bearing using crutches with 20 kg was started at 3 weeks with progression to full weight-bearing at 4 weeks.
Postoperative follow-up
Postoperative follow-up evaluations were periodically performed every 3 months within a year and then every 6 months afterward. Comprehensive radiological and clinical evaluations were conducted at 6 months and 1 year, and the results were compared to the preoperative status. To examine whether the surgical results could be attained as planned, radiological parameter values at the preoperative planning and the 1-year postoperative evaluation were compared for each case, and the difference was regarded an indicator for surgical accuracy. The study design was approved by the Institutional Review Board of Hyogo College of Medicine [No. 2218], and informed consent was obtained from all study subjects.
Statistical analysis
Differences between the pre- and postoperative clinical and radiological parameters were statistically assessed using the paired Student’s t test with a significance level set at P < 0.05. The statistical analysis was performed using SPSS version 19 software (IBM, Armonk, New York, USA). A post hoc power analysis was conducted for comparison of the pre-and postoperative radiological parameters using a 2-sided test. Consequently, it was shown that the sample size of 20 in this study could achieve an adequate power of 0.99 with an α of 0.05.
Results
As for postoperative complications, a major intraoperative arterial injury was encountered in a 44-year-old female patient. In this case, the popliteal artery was injured during the distal femoral osteotomy. Although major bleeding was stopped by local compression, immediate postoperative examination revealed clinical signs of circulatory deficiency. CT angiographic findings indicated injury to the popliteal artery. Six hours after surgery, the injured site was primarily repaired by the vascular surgeons. Although the operated limb could be salvaged, peroneal nerve palsy and drop foot due to a subsequent compartment syndrome remained as a sequel. During the study period, no other complication related to the surgical procedure was noted, and solid bony union was achieved in all knees before 1 year .
Radiological results (Table 1)
Preoperatively, all knees exhibited varus deformity with the mean mTFA angle of 13.5° ± 3.1° varus (range 10.2°–23.6°). The mean mLDFA was 91.2° ± 1.4° (range 88.8°–95°), and the mean mMPTA was 82.3 ± 2.0° (range 77.2°–86.4°) indicating that sources of the deformity were present in both femoral and tibial sides. The mean JLCA was 5.8 ± 2.3° (range 2.5°–10.8°) showing increased joint convergence compared to the normal value.
Radiological evaluation at 6 months showed restoration of normal knee alignment with the mean TFA corrected from 13.5° varus to 1.1° valgus. Other radiological parameters for joint orientation, such as mLDFA and mMPTA, were corrected to normal ranges with significant postoperative changes. JLCA was also significantly reduced after surgery. When these values were repeatedly measured at 12 months, no changes were noted during the subsequent postoperative period, and thus restoration of normal alignment and orientation confirmed at 6 months was maintained up to 12 months after surgery. In the preoperative surgical simulation, the correction angles for the femur and the tibia were planned to be 6.5° ± 1.3° and 9.4° ± 2.4° on average, while the angles actually attained at surgery were 5.6° ± 1.8° and 8.2° ± 3.4°, respectively, based on the differences between the angle values measured before surgery and at 12 months. Consequently, surgical accuracy values, defined as the differences between the preoperative planning and 12-month postoperative measurements for mTFA, mLDFA, and mMPTA angles, ranged from 1.4° to 2.1° on average (Table 2), and satisfactory surgical accuracy could be accomplished.
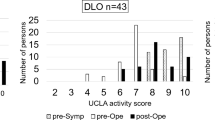
Clinical results
As shown in Table 3, clinical outcomes as assessed by the KOOS and IKDC subjective scores significantly improved after surgery. Clinical improvement was already evident as early as 6 months after surgery and maintained at 12 months.
Discussion
The most important findings of the present study were that DLO performed for severe varus osteoarthritic knees in our practice could achieve restoration of normal knee alignment and orientation with resultant improvement in patient-registered clinical outcomes. No changes in radiological parameters from 6 to 12 months and satisfactory clinical improvement as early as 6 months indicate that satisfactory bony union and early functional recovery could be accomplished by the refined surgical procedure with minimally invasive biplanar osteotomy and rigid internal fixation.
The procedure and outcomes of DLO were initially reported in the 1960s by Benjamin [4]. He reviewed his experiences with DLO for knees with rheumatoid arthritis (RA) and osteoarthritis (OA) and reported favourable results. Subsequent to this paper, several studies examined the efficacy of DLO as a surgical option for knees with joint destruction and severe impairment [2, 16, 32, 38]. The majority of these studies reported rather unfavourable surgical outcomes with unpredictable symptomatic relief and a substantially high incidence of postoperative motion loss. Schüller et al. have stated that DLO should be abandoned in management of RA knees [32], while Iveson et al. reported a higher incidence of complication following DLO compared to single (isolated tibial) osteotomy [16]. However, it should be noted that surgical indication of DLO in these studies included both RA and OA knees and strict consideration for knee joint alignment and orientation was not given. Moreover, extensive surgical exposure was required, and no internal fixation was used to fix the osteotomy site. Therefore, the rather negative reports in those days cannot be extrapolated to DLO with modern surgical concepts and procedures.
In 2002, Babis et al. [3] presented a paper describing indication and results of double level osteotomy for varus osteoarthritic knees with the application of a modern surgical concept and procedure. They precisely analyzed the alignment for each knee using computer-aided radiological analysis, and indication for DLO was determined based on preoperative planning using a computer-based system (OASIS: Osteotomy Analysis and Simulation Software). In their series, DLO was performed for 29 knees with an average preoperative mTFA of -13.9° (varus), which corresponded to the amount of varus deformity in our patient population. When conversion to TKA or severe pain was deemed to be a surgical failure, the cumulative survival rate at an average follow-up period of 100 months was 95%. In 2012, Saragaglia et al. reported satisfactory results of DLO performed for osteoarthritic knees with severe varus [27]. They utilized the principles of computer-assisted surgery to achieve the intended amount of correction. CWDFO followed by OWHTO of the tibia and the use of intraoperative navigation in their procedure enabled accurate and consistent deformity correction. In addition, the use of a rigid plate fixation helped prevent postoperative alignment change caused by malunion. These two studies have shown that DLO can achieve satisfactory mid- to long-term outcome if the appropriate surgical indicate and procedure are followed; however, subsequent to these two papers, there have been no papers reporting radiological and functional outcomes of DLO. In recent years, the surgical technique for DLO has further evolved with the introduction of minimally invasive biplanar osteotomy and rigid internal fixation with a locking compression plate system. The intent of the present study was to report the surgical outcome using these current procedure modifications.
The theoretical advantage of DLO over single-level HTO is correction of severe varus knee deformity with restoration of physiological joint line inclination. Joint line obliquity following a large amount of correction by performing a tibial osteotomy alone may lead to several potential problems [13, 20, 25, 26]. Based on the follow-up results after single level HTO, Terauchi et al. reported that knees with varus inclination of the distal femur bear the risk for postoperative recurrence of varus deformity and recommended TKA or overcorrection for those knees rather than considering the increased surgical invasion associated with DLO [36].
In the surgical planning in our current practice, the intended radiological parameters were adjusted to the normal ranges with an mTFA of 0.5°–1° (a slight valgus), an mMPTA of 90°, and an mLDFA of 85°. To date, no consensus has been reached regarding the optimal alignment and orientation to aim for. Although overcorrection in coronal alignment with lateral deviation of the mechanical axis at the joint level is advocated in some papers [3, 36], our surgical procedure with only mild overcorrection (mean postoperative mTFA: 0.8°) and restoration of physiological joint orientation parameters (mLDFA and mMPTA) could attain satisfactory functional improvement. In addition, a satisfactory bony union without postoperative alignment change and early functional recovery as early as 6 months were noted in this study, which further support the efficacy of the current procedure with minimally invasive biplanar osteotomy with rigid internal fixation.
There are several limitations included in the study. First, the follow-up period (minimum of 1 year) was too short, and the number of included subjects was small. Second, the goal of alignment for DLO in this study was close to neutral; however, the optimal postoperative alignment has yet to be defined. Moreover, all radiological assessments were performed by one observer which may induce bias. Although inter- and intraobserver reliabilities for the radiological assessments were not examined in this study, high intra- and interrater reliabilities with the use of digital planning software has been confirmed in a previous study [31].
Conclusions
The minimally invasive DLO technique is a valuable surgical technique accomplishing restoration of physiologic knee joint alignment and orientation with significant improvement in patient-registered clinical outcomes in the early postoperative evaluation.
References
Akiyama T, Okazaki K, Mawatari T, Ikemura S, Nakamura S (2016) Autologous osteophyte grafting for open-wedge high tibial osteotomy. Arthrosc Tech 5:e989–e999
Angel JC, Liyanage SP, Griffiths WE (1974) Double osteotomy for the relief of pain in arthritis of the knee. Rheumatol Rehabil 13:109–119
Babis GC, An KN, Chao EY, Rand JA, Sim FH (2002) Double level osteotomy of the knee: a method to retain joint-line obliquity. Clinical results. J Bone Jt Surg Am 84:1380–1388
Benjamin A (1969) Double osteotomy for the painful knee in rheumatoid arthritis and osteoarthritis. J Bone Jt Surg Br 51:694–699
Benjamin A (1974) Double osteotomy of the knee. Scand J Rheumatol 3:65
Bonnin MP, Laurent JR, Zadegan F, Badet R, Pooler Archbold HA, Servien E (2013) Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc 21:64–73
Brinkman JM, Freiling D, Lobenhoffer P, Staubli AE, van Heerwaarden RJ (2014) Supracondylar femur osteotomies around the knee: Patient selection, planning, operative techniques, stability of fixation, and bone healing. Orthopade 43:S1–S10
Brinkman JM, Luites JW, Wymenga AB, van Heerwaarden RJ (2010) Early full weight bearing is safe in open-wedge high tibial osteotomy. Acta Orthop 81:193–198
Elson DW (2017) The surgical accuracy of knee osteotomy. Knee 24:167–169
Freiling D, van Heerwaarden R, Staubli A, Lobenhoffer P (2010) Die varisierende Closed-Wedge-Osteotomie am distalen Femur zur Behandlung der unikompartimentalen lateralen Arthrose am Kniegelenk. Oper Orthop Traumatol 22:317–334
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P (2013) Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc 21:170–180
Freiling D, van Heerwaarden R, Staubli A, Lobenhoffer P (2010) The medial closed-wedge osteotomy of the distal femur for the treatment of unicompartmental lateral osteoarthritis of the knee. Oper Orthop Traumatol 22:317–334
Hernigou P, Duffiet P, Julian D, Guissou I, Poignard A, Flouzat-Lachaniette CH (2013) Outcome of total knee arthroplasty after high tibial osteotomy: does malalignment jeopardize the results when using a posterior-stabilized arthroplasty? HSS J 9:134–137
Hierholzer G, Müller K (1985) Corrective osteotomies of the lower extremity after trauma, vol 1, Springer, Berlin, pp 195–223
Hofmann S, Lobenhoffer P, Staubli A, Van Heerwaarden R (2009) Osteotomies of the knee joint in patients with monocompartmental arthritis. Orthopade 38:755–769
Iveson JM, Longton EB, Wright V (1977) Comparative study of tibial (single) and tibiofemoral (double) osteotomy for osteoarthrosis and rheumatoid arthritis. Ann Rheum Dis 36:319–326
Kobayashi H, Akamatsu Y, Kumagai K, Kusayama Y, Saito T (2017) Radiographic and computed tomographic evaluation of bone union after medial opening wedge high tibia osteotomy with filling gap. Knee 24:1108–1117
Lee KM, Chang CB, Park MS, Kang SB, Kim TK, Chung CY (2015) Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthritis Cartilage 23:232–238
Lobenhoffer P, Agneskirchner JD (2003) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11:132–138
Nakayama H, Schröter S, Yamamoto C, Iseki T, Kanto R, Kurosaka K, Kambara S, Yoshiya S, Higa M (2018) Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc 26:1873–1878
Niemeyer P, Koestler W, Kaehny C, Kreuz PC, Brooks CJ, Strohm PC, Helwig P, Suedkamp NP (2008) Two-year results of open-wedge high tibial osteotomy with fixation by medial plate fixator for medial compartment arthritis with varus malalignment of the knee. Arthroscopy 24:796–804
Oh KJ, Ko YB, Bae JH, Yoon ST, Kim JG (2016) Analysis of knee joint line obliquity after high tibial osteotomy. J Knee Surg 29:649–657
Paley D, Herzenberg J (2005) Principles of deformity correction, vol 3. Springer, Berlin, pp 1–18
Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A (1994) Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 25:425–465
Preston S, Howard J, Naudie D, Somerville L, McAuley J (2013) Total knee arthroplasty after high tibial osteotomy: no differences between medial and lateral osteotomy approaches. Clin Orthop Relat Res 472:105–110
Ramappa M, Anand S, Jennings A (2013) Total knee replacement following high tibial osteotomy versus total knee replacement without high tibial osteotomy: a systematic review and meta-analysis. Arch Orthop Trauma Surg 133:1587–1593
Saragaglia D, Nemer C, Colle PE (2008) Computer-assisted double level osteotomy for severe genu varum. Sports Med Arthrosc 16:91–96
Schröter S, Ateschrang A, Lowe W, Nakayama H, Stockle U, Ihle C (2015) Early full weight-bearing versus 6-week partial weight-bearing after open wedge high tibial osteotomy leads to earlier improvement of the clinical results: a prospective, randomised evaluation. Knee Surg Sports Traumatol Arthrosc 25:325–332
Schröter S, Gonser CE, Konstantinidis L, Helwig P, Albrecht D (2011) High complication rate after biplanar open wedge high tibial osteotomy stabilized with a new spacer plate (Position HTO Plate) without bone substitute. Arthroscopy 27:644–652
Schröter S, Ihle C, Elson DW, Döbele S, Stöckle U, Ateschrang A (2016) Surgical accuracy in high tibial osteotomy: coronal equivalence of computer navigation and gap measurement. Knee Surg Sports Traumatol Arthrosc 24:3410–3417
Schröter S, Ihle C, Mueller J, Lobenhoffer P, Stockle U, van Heerwaarden R (2013) Digital planning of high tibial osteotomy. Interrater reliability by using two different software. Knee Surg Sports Traumatol Arthrosc 21:189–196
Schüller HM, van Dijk CN, Fidler MW (1987) Poor results of double osteotomy for the rheumatoid knee. Acta Orthop Scand 58:253–255
Staubli AE, De Simoni C, Babst R, Lobenhoffer P (2003) TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia–early results in 92 cases. Injury 34:55–62
Strecker W (2006) Planning analysis of knee-adjacent deformities. I. Frontal plane deformities. Oper Orthop Traumatol 18:259–272
Takeuchi R, Bito H, Akamatsu Y, Shiraishi T, Mosishita S, Koshino T, Saito T (2010) In vitro stability of open wedge high tibial osteotomy with synthetic bone graft. Knee 17:217–220
Terauchi M, Shirakura K, Katayama M, Higuchi H, Takagishi K, Kimura M (2002) Varus inclination of the distal femur and high tibial osteotomy. J Bone Jt Surg Br 84:223–226
Visser J, Brinkman JM, Bleys RL, Castelein RM, van Heerwaarden RJ (2013) The safety and feasibility of a less invasive distal femur closing wedge osteotomy technique: a cadaveric dissection study of the medial aspect of the distal femur. Knee Surg Sports Traumatol Arthrosc 21:220–227
Zaalberg GS, Wouters HW (1972) Double osteotomy of the knee-joint according to Benjamin. Acta Orthop Belg 58:89–90
Funding
There was no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study fornal consent is not required.
Rights and permissions
About this article
Cite this article
Nakayama, H., Iseki, T., Kanto, R. et al. Physiologic knee joint alignment and orientation can be restored by the minimally invasive double level osteotomy for osteoarthritic knees with severe varus deformity. Knee Surg Sports Traumatol Arthrosc 28, 742–750 (2020). https://doi.org/10.1007/s00167-018-5103-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5103-3