Abstract
Purpose
This study was performed to prospectively compare the clinical and radiographic results between mobile-bearing (MB) and fixed-bearing (FB) TKAs using ceramic titanium nitride (TiN)-coated prostheses.
Methods
Seventy MB and 70 FB TKAs using TiN-coated prostheses (ACS®) were prospectively evaluated. There were no differences in demographic characteristics between the two groups. Clinically, the Knee Society knee and function scores, WOMAC, and range of motion (ROM) were compared. Considering the possibility of a kinematic change in the polyethylene (PE) insert and a decrease in ROM following MB TKA, serial changes in the ROM were also compared. The thickness of the PE insert was compared according to the size of the femoral component. Radiographically, the alignment and positions of the components were compared.
Results
There were no differences between the two groups in clinical scores or ROM (n.s.). The maximum flexion increased from 133.5° ± 8.3° to 137.6° ± 5.5° across all time points in the MB group. The serial maximum flexion angles did not differ between the two groups over time (n.s.). The average thickness of the PE insert was greater in the MB group (12.0 ± 1.9 vs. 11.2 ± 1.6 mm, respectively, p = 0.008), especially when a large femoral component was used (12.7 ± 1.9 vs. 11.0 ± 1.5 mm, p = 0.005). The pre- and postoperative mechanical axes and positions of the components did not differ between the two groups (n.s.).
Conclusions
TiN-coated MB TKA showed no significant advantage over FB TKA. The selection of bearing design would be clinically insignificant when using the TiN-coated TKA prosthesis.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The mobile-bearing (MB) prosthesis was designed to provide dual-surface articulation at both the upper and lower surfaces of a polyethylene (PE) insert after total knee arthroplasty (TKA). MB prostheses provide the advantages of increased femorotibial conformity and reduced contact stress and wear [13]. They also have the potential advantage of self-correcting rotational mismatch between the femur and tibia by optimizing the patellofemoral mechanics [28, 34]. Thus, enhancements in the range of motion (ROM) and deep knee flexion were expected from MB prostheses due to their more physiological kinematics [13]. However, previous randomized controlled trials [19, 22] and meta-analyses [13, 17] comparing fixed-bearing (FB) and MB TKA revealed no significant differences in the clinical or radiographic results, or survival rates, between these prostheses.
TKA prostheses commonly consist of cobalt–chromium-based alloys and ultrahigh molecular weight PE. Depositing a ceramic coating such as titanium nitride (TiN) on the surface is an alternative method of increasing the abrasion resistance of the metal components [20, 31]. The durability and abrasion strength of the coating surface were confirmed previously by retrieval and microscopic analyses [7, 12]. TiN provides a smoother, more wettable, and scratch-resistant surface, and minimizes wear of the PE insert [20]. Several clinical studies [27, 32] demonstrated promising mid-term clinical and radiographic results after TKA using TiN-coated MB prostheses. However, the authors did not determine whether these results were due to the TiN coating or the MB prosthesis.
A previous roentgen stereophotogrammetric analysis [36] demonstrated that the axial rotatory motion of MB prostheses decreased over time, indicating that kinematic changes had been caused by intrinsic factors. The motion between two different materials inevitably raises the resistance. Carbides, characterized by marked hardness, partly protrude from the surface of the metal component and thus increase the roughness of the articulating surface. They can be covered by the much harder TiN coating, thus obtaining a smoother surface; the roughness of cobalt chrome prostheses was reported to increase twofold during in vivo service compared to TiN-coated prostheses [12]. Furthermore, the high wettability of this component increases the lubrication, thus reducing the coefficient of friction compared to cobalt chrome implants [5]. TiN-coated MB prostheses have not yet been proven to retain rotary motion over time.
The Advanced Coated System (ACS)® (Implantcast GmbH, Buxtehude, Germany) provides an optimal solution for MB and FB TKA. The differences between MB and FB TKAs could depend on the characteristics of the articulating materials because the knee kinematics could be influenced by the roughness, lubrication, and wettability of the surface. Therefore, comparison of MB and FB TKAs using ceramic TiN-coated prostheses, which were different from previous cobalt chrome prostheses, will be necessary. To our knowledge, there have been no previous studies comparing the results between MB and FB TKAs using ceramic TiN-coated prostheses.
This study was performed to prospectively compare the clinical and radiographic results between MB and FB TKA using ceramic TiN-coated prostheses. It was hypothesized that the clinical and radiographic results of one type of prosthesis would be comparable to or better than those of the other type, especially with regard to ROM.
Materials and methods
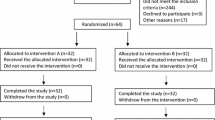
All consecutive patients undergoing primary TKA using TiN-coated posterior-stabilized prostheses (ACS® prosthesis) between January 2013 and December 2014 were enrolled in this study and prospectively evaluated. All TKAs were performed by a senior surgeon with more than 30 years of surgical experience. The study was approved by the institutional review board of our hospital (KHUH 2012-10-502). A detailed informed consent form was signed by each patient, and all information was kept confidential.
The inclusion criteria for patients were knee osteoarthritis of Kellgren–Lawrence grade 4 and persistent pain despite conservative treatment. The exclusion criteria were bilateral and revision TKA, inflammatory arthritis (except rheumatoid arthritis), previous ligament injuries, previous reconstructive procedures, and post-traumatic or post-infectious arthritis. During this period, 140 knees of 140 patients underwent TKA using ACS® prostheses according to the above inclusion and exclusion criteria. No patients were lost to follow-up before 2 years. The MB and FB prostheses were selected according to a number previously created by an online number generator, in the absence of clear indications for using either type of prosthesis [30].
The median age was 68 (range 52–82) years in the MB group and 69 (range 54–86) years in the FB group at the time of surgery. There were no significant differences between the two groups in terms of demographics or preoperative clinical status (Tables 1, 2). The average follow-up period was 4.1 years in both groups (Table 1).
Clinical evaluation
The patients’ clinical and radiographic results were evaluated in detail. Patients were contacted on a regular basis, and examinations were performed postoperatively at 6 weeks, 3 months, 6 months, and 1 year, and annually thereafter.
The Knee Society knee score and function score were used to evaluate pain and function [18]. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [14] was also recorded. The ROM was measured with a long-armed goniometer to determine the flexion contracture and maximum flexion angle. Considering the possibility of a kinematic change in the PE insert and decreasing maximum flexion angle during follow-up after MB TKA [36], serial changes in the maximum flexion angle, preoperatively and at 6 weeks, 3 months, 6 months, 1 year, 2 years, and the last follow-up postoperatively, were also compared between the two groups.
The thickness of the PE insert was recorded and compared between the MB and FB groups. It was also compared between the two groups according to the size of the femoral component.
Radiographic evaluation
Pre- and postoperative anteroposterior (AP), lateral, and axial radiographs, and orthoroentgenograms (full-length standing AP radiographs) were obtained to assess limb alignment and component positioning.
The pre- and postoperative mechanical axes were defined as the angle between the femoral and tibial mechanical axes on orthoroentgenograms. Detailed analyses of the AP and lateral radiographs were performed to evaluate the positions of components with α, β, γ, and δ angles by the Knee Society radiological evaluation method [11].
Pre- and postoperative true lateral views of the knee, in which the distal and posterior femoral condyles overlapped exactly, were obtained to measure the tibial posterior slope angle. The tibial posterior slope angle was defined as the angle formed by the perpendicular line of the tibial medullary canal axis and the medial tibial plateau (Fig. 1). Preoperative and postoperative patellar tilt angles were measured in Merchant view (Fig. 2). A positive value indicated opening toward the medial side of the patella. The joint line height was defined as the shortest distance between the fibular head and the lateral femoral condyle on AP radiographs (Fig. 3) [2].
Method for measuring the proximal tibial medullary canal-referenced posterior slope angle (°) (posterior slope: 90-a). The reference line connects two points, each of which is at the center of the medullary canal, 5 cm below the tibial tuberosity and 15 cm distal to the medial tibial plateau. The tibial posterior slope angle was defined as the angle formed by the perpendicular line of the tibial medullary canal axis and the medial tibial plateau
Method of measuring patellar tilt angle (°). A The preoperative patellar tilt angle is defined as the angle subtended by the equatorial line of the patella and the line connecting the anterior limits of the femoral condyles in Merchant view. b The postoperative patellar tilt angle is defined as the angle subtended by the equatorial line of the patella and the line connecting the anterior limits of the femoral component
Measurements were made on these images using a picture archiving and communication system (PACS) (Infinitt Healthcare, Seoul, South Korea). The quality of radiographic evaluation could be improved by standardization of the position of the knee and use of an identical distance between the X-ray beam and cassette. The images were transferred digitally to a PACS and then manipulated. Assessment was performed on a 61-cm (24-inch) monitor (SyncMaster 2494HMN; Samsung, Seoul, South Korea) in portrait mode using PACS software (Infinitt Healthcare). The software was capable of detecting minimum differences of 0.1° in angle and 0.1 mm in length [21].
Surgical technique and rehabilitation
The surgical techniques and principles did not differ between MB and FB TKAs. A medial parapatellar approach was used with a midline skin incision. Bone cuts were made with modified measured resection. Carefully planned soft tissue balancing was also performed. An intramedullary guide was used for femoral resection, and the transepicondylar axis was used to position the AP femoral cutting guide system for femoral component rotation. An extramedullary guide was used for tibial resection. The reference line for tibial rotation was accurately aimed at a line passing through the medial third of the tibial tuberosity and the second metatarsal or the middle of talus, which is 3–5 mm medial to the center of the ankle. The tibial slope was usually set to 3° of the posterior slope in the sagittal plane. Any contracted medial or lateral soft tissue was carefully evaluated with palpation and then selectively released as required to balance the knee. The flexion and extension gaps were also checked with a spacer block or trial component. All patellae were resurfaced and all implants were cemented onto cleaned, dried surfaces. The patellofemoral articulation was carefully evaluated with the no-thumb technique. No lateral retinacular release was performed. There were no knees in which postoperative patellar subluxation occurred.
Isometric exercises using the extensor and flexor muscles were initiated shortly after the operation. A Hemovac drain was inserted during surgery and then removed on the second postoperative day, followed by initiation of active and assisted ROM exercise. Full weight-bearing ambulation was started to the extent permitted by the patient’s condition at 4 days. There were no patients in whom postoperative stiffness necessitated manipulation under anesthesia.
Statistical analysis
The preoperative clinical and radiographic results were compared with the postoperative results (paired t test). Clinical and radiographic results before TKA and at the last follow-up visit were compared between the two groups (Student’s t test, Chi-square test, or Fisher’s exact test). Statistical analyses were performed with SPSS software (ver. 18.0; SPSS Inc., Chicago, IL, USA), and p < 0.05 was taken to indicate statistical significance.
To minimize any observation bias, two independent investigators repeated all radiographic measurements at an interval of 2 weeks. The intra- and interobserver reliabilities of all measurements were assessed with the intraclass correlation coefficient. In this study, the intraclass correlation coefficient values of all measurements were > 0.8 for both intra- and interobserver reliability. Thus, the average values could be used for the analysis.
Power analysis was performed to determine the minimum sample size affording sufficient power, with serial maximum flexion angle as the primary outcome. The clinically acceptable significant difference in the maximum flexion angle was set to 10° in flexion. Power analysis indicated that more than 52 cases were required to achieve sufficient power. Consequently, 70 patients each were included in the MB and FB groups.
Results
Clinical results
The average Knee Society knee and function scores, WOMAC score, and ROM had significantly improved at the last follow-up in both the MB and FB groups (Table 2). There were no differences in these scores or the ROM between the two groups (n.s.) (Table 2). The serial maximum flexion angles in the MB group at 6 weeks, 3 months, 6 months, 1 year, and 2 years postoperatively were 133.5° ± 8.3°, 136.0° ± 6.0°, 136.9° ± 5.8°, 137.7° ± 5.4°, and 137.6° ± 5.5°, respectively. The postoperative maximum flexion angle did not differ between the two groups at any time point (Table 3).
The average thickness of the PE insert was slightly greater in the MB group than the FB group (12.0 vs. 11.2 mm, respectively, p = 0.008). This tendency seemed to depend on the size of the femoral component, because it was thicker in the MB group only when a large femoral component was used (12.7 vs. 11.0 mm, respectively, p = 0.005) (Table 4).
Radiographic results
The average pre- and postoperative mechanical axes and positions of the components did not differ between the MB and FB groups (n.s.) (Table 5). The positions of the components in all patients were within the permissible range of ± 3°, except for the sagittal position of the femoral component in one patient in the FB group. None of the knees showed progressive or symptomatic radiolucent lines with a width ≥ 2 mm at any follow-up time point. The positions of all components remained unchanged.
There were no significant differences in the tibial posterior slope angle, patellar tilt angle, or joint line height between the two groups (Table 5).
Discussion
The most important finding of the present study was that the mid-term clinical and radiographic results after MB and FB TKA using TiN-coated prostheses were similar in terms of Knee Society knee and function scores, WOMAC score, and ROM, with satisfactory alignment and positioning of the components.
A number of previous studies [13, 22, 23, 29] showed that the cobalt–chromium-based alloy MB prosthesis achieves results that are essentially equivalent to those with the FB prosthesis. Kim et al. [23] performed a prospective randomized controlled trial with 444 patients who had simultaneous bilateral TKAs using the press-fit condylar Sigma MB prosthesis for one knee and the FB prosthesis for the opposite knee. They reported that excellent clinical and radiographic results were achieved at a minimum follow-up duration of 10 years, and there were no significant differences in Knee Society knee score, WOMAC score, University of Los Angeles activity score, ROM, or radiographic findings according to the type of prosthesis used. Matsuda et al. [26] also compared the clinical and radiographic results of NexGen Legacy posterior-stabilized (LPS) Flex (Zimmer Inc., Warsaw, IN) MB and FB TKAs, with specific attention paid to rotational alignment and ROM. This prospective, randomized study did not reveal any clinical advantages of the MB knee. Analysis of rotational alignment by CT did not reveal a particular advantage of the self-aligning mechanism of MB implants, as the clinical scores and ROM were similar between the two groups.
In the present study, there were no significant clinical or radiographic advantages of MB over FB ceramic TiN-coated prostheses. The present study is unique in that it represented the first comparison between MB and FB TKAs performed using ceramic TiN-coated prostheses. Most previous studies focused on comparison of TKAs between ceramics (such as zirconium and oxinium) and cobalt chrome [1, 33]. Several studies reported the outcomes of MB TiN-coated prostheses, but did not compare the outcomes of TiN-coated MB and FB TKAs [4, 27]. As knee kinematics could be influenced by surface lubrication and wettability, we felt that comparison of MB and FB TKAs using ceramic TiN-coated prostheses was a necessary addition to the literature.
The present study revealed a consistent increasing tendency in the postoperative maximum flexion angle over time. Wolterbeek et al. [36] performed a fluoroscopic study of knee kinematics at 8 months and 3 years to accurately assess changes in axial rotation over time in MB TKAs using NexGen LPS prostheses. The rotation of the femoral component and PE insert proved to be limited at 8 months postoperatively, and even decreased over time. The authors emphasized the importance of re-evaluating knee kinematics over time after MB TKA due to the possibility of low conformity between the femoral component and the PE insert, impingement due to the fixed anterior position of the PE insert-tibia pivot point, and fibrous tissue formation. However, in our study, there was no decrease in maximum flexion angle after either MB TKA or FB TKA. The average maximum flexion angles for MB TKAs were 136.0° and 137.6° at 6 months and 2 years postoperatively, respectively. These discrepancies between the results of the present and previous studies require further systematic study.
Another interesting finding was that there was no difference in maximum flexion between patients with MB and FB TiN-coated TKAs according to time. Several prospective randomized studies indicated that MB TKA patients seem to regain their motion earlier than FB TKA patients with cobalt chrome prostheses [15, 25]. Mahoney et al. [25] reported that the average knee flexion angle was greater in the MB group than the FB group at 6 months and 1 year postoperatively, but did not differ between the two groups at 2 years postoperatively. Harrington et al. [15] suggested that the better early motion could potentially be attributed to the design and kinematics of the MB. However, in the present study, the postoperative average maximum flexion angle was slightly greater in the MB group than the FB group at 3 and 6 months, although the difference was not statistically significant (Table 3). Although the ceramic used for FB TKAs, which provides a smoother, more wettable surface, may have contributed to the similar results obtained for MB and FB prostheses, additional studies in larger cohorts are necessary.
The only difference among the evaluated parameters in the present study was the thickness of the PE insert. The average thickness of the PE insert was slightly greater in the MB group than in the FB group, especially when a large femoral component of size #3 was used (12.7 vs. 11.0 mm, respectively, p = 0.005) (Table 4). Bearing dislocation and instability are major concerns in MB TKA, and an accurate surgical technique is mandatory during this procedure [8, 10]. We felt that the effort required to maximize flexion stability may have increased the thickness of the PE insert in MB TKA. However, we could not elucidate the precise mechanism responsible for the increased PE insert thickness, especially when a large femoral component (size #3) was used. A previous study using the ACS® MB prosthesis indicated that the thickness of the PE insert increased according to the size of the tibial component, and the authors also could not explain this phenomenon [27]. However, the flexion gap is influenced by the size of the femoral, rather than the tibial, component.
The tendency of the PE insert thickness to increase according to the size of the femoral component may have arisen from the morphological characteristics of the distal femur and the aspect ratio (AP/ML ratio) in Asian populations; numerous morphological studies have demonstrated that Asians have small and narrow femoral condyles [6, 37]. Hitt et al. [16] reported mismatches in both size and aspect ratio, and found that prostheses do not account for changes in aspect ratio across femoral condylar sizes. Mediolateral overhang can result in irritation of the soft tissue or overstuffing of the joint space [3]. It also increases the incidence of femoral component downsizing, which could make accurate flexion/extension balancing difficult [9]. This may have increased the thickness of the PE insert in combination with the surgeons’ concerns of instability in MB TKA.
The present study had several strengths. First, it included consecutive patients without loss to follow-up. Furthermore, the sample size was calculated through power analysis, all data were collected prospectively and analyzed as planned, and the radiographic measurements from high-quality images using a PACS permitted evaluation of patellofemoral articulation features, such as the patellar tilt angle.
The study also had limitations. First, there was no direct evidence that the nature of the surface, for example, in terms of surface roughness and friction coefficient, affects the rotational motion of the MB associated with knee flexion. Several factors, including implant design, soft tissue balancing, and formation of fibrous tissue, are known to affect MB motion [35, 36]. Zurcher et al. [38] reported that the implant design had a greater impact on rotatory bearing motion. The surface of the prosthesis was thought to be one of the implant features affecting the motion. In addition, the formation of fibrous tissue can influence the late limitation of motion on mobile bearing surfaces [36]. Accordingly, the serial knee flexion of TiN-coated MB and FB prostheses with different surfaces was compared to those described in the literature.
Another limitation was the relatively short follow-up in which to evaluate the benefit of wear resistance in TiN-coated TKA. A long-term follow-up evaluation is necessary, including survivorship analysis related to wear, because ceramic TiN-coated prostheses have the potential advantage of wear resistance. The study was also limited by differences in patient demographics from those of Western populations. Most of the patients in the present study were female and had a low BMI. Low BMIs and a higher proportion of females with osteoarthritis are common findings in Korean populations [24]. These differences should be taken into consideration when extrapolating our findings to other populations. Finally, the ROM was not measured radiographically under weight-bearing conditions.
Conclusion
In this study, clinical and radiographic results were similar after TKA using TiN-coated MB and FB prostheses. No significant advantage was found for TiN-coated MB TKA over FB TKA. The selection of bearing design would be clinically insignificant when using a TiN-coated TKA prosthesis.
References
Anderson FL, Koch CN, Elpers ME, Wright TM, Haas SB, Heyse TJ (2017) Oxidised zirconium versus cobalt alloy bearing surfaces in total knee arthroplasty: 3D laser scanning of retrieved polyethylene inserts. Bone Joint J 99-B(6):793–798
Bae DK, Song SJ, Park CH, Liang H, Bae JK (2017) Comparison of mid-term results between conversion total knee arthroplasties following closed wedge high tibial osteotomy and primary total knee arthroplasties: a matched pair study including patellar symptom and position. J Orthop Sci 22(3):495–500
Bonnin MP, Schmidt A, Basiglini L, Bossard N, Dantony E (2013) Mediolateral oversizing influences pain, function, and flexion after TKA. Knee Surg Sports Traumatol Arthrosc 21(10):2314–2324
Breugem SJM, Linnartz J, Sierevelt I, Bruijn JD, Driessen MJM (2017) Evaluation of 1031 primary titanium nitride coated mobile bearing total knee arthroplasties in an orthopedic clinic. World J Orthop 8(12):922–928
Campbell P, Shen FW, McKellop H (2004) Biologic and tribologic considerations of alternative bearing surfaces. Clin Orthop Relat Res 418:98–111
Cheng FB, Ji XF, Lai Y, Feng JC, Zheng WX, Sun YF et al (2009) Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee 16(5):341–347
Ching HA, Choudhury D, Nine MJ, Abu Osman NA (2014) Effects of surface coating on reducing friction and wear of orthopaedic implants. Sci Technol Adv Mater 15(1):014402
Crossett LS (2002) Fixed- versus mobile-bearing total knee arthroplasty: technical issues and surgical tips. Orthopedics 25(2 Suppl):s251–256
Dai Y, Scuderi GR, Penninger C, Bischoff JE, Rosenberg A (2014) Increased shape and size offerings of femoral components improve fit during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(12):2931–2940
Diamond OJ, Doran E, Beverland DE (2017) Spinout/dislocation in mobile-bearing total knee arthroplasty: a report of 26 cases. J Arthroplasty. https://doi.org/10.1016/j.arth.2017.09.016
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Fabry C, Zietz C, Baumann A, Ehall R, Bader R (2017) High wear resistance of femoral components coated with titanium nitride: a retrieval analysis. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4578-7
Fransen BL, van Duijvenbode DC, Hoozemans MJM, Burger BJ (2017) No differences between fixed- and mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25(6):1757–1777
Giesinger JM, Hamilton DF, Jost B, Behrend H, Giesinger K (2015) WOMAC, EQ-5D and knee society score thresholds for treatment success after total knee arthroplasty. J Arthroplasty 30(12):2154–2158
Harrington MA, Hopkinson WJ, Hsu P, Manion L (2009) Fixed- vs mobile-bearing total knee arthroplasty: does it make a difference?—a prospective randomized study. J Arthroplasty 24(6 Suppl):24–27
Hitt K, Shurman JR 2nd, Greene K, McCarthy J, Moskal J, Hoeman T et al (2003) Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am 85-A(Suppl 4):115–122
Hofstede SN, Nouta KA, Jacobs W, van Hooff ML, Wymenga AB, Pijls BG et al (2015) Mobile bearing vs fixed bearing prostheses for posterior cruciate retaining total knee arthroplasty for postoperative functional status in patients with osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003130.pub3(2):CD003130
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Jain NP, Lee SY, Morey VM, Chong S, Kang YG, Kim TK (2017) Early clinical outcomes of a new posteriorly stabilized total knee arthroplasty prosthesis: comparisons with two established prostheses. Knee Surg Relat Res 29(3):180–188
Kang KT, Son J, Kim HJ, Baek C, Kwon OR, Koh YG (2017) Wear predictions for UHMWPE material with various surface properties used on the femoral component in total knee arthroplasty: a computational simulation study. J Mater Sci Mater Med 28(7):105
Kim CW, Lee CR (2018) Effects of femoral lateral bowing on coronal alignment and component position after total knee arthroplasty: a comparison of conventional and navigation-assisted surgery. Knee Surg Relat Res 30(1):64–73
Kim YH, Park JW, Kim JS (2018) Comparison of high-flexion fixed-bearing and high-flexion mobile-bearing total knee arthroplasties—a prospective randomized study. J Arthroplasty 33(1):130–135
Kim YH, Park JW, Kim JS, Kulkarni SS, Kim YH (2014) Long-term clinical outcomes and survivorship of press-fit condylar sigma fixed-bearing and mobile-bearing total knee prostheses in the same patients. J Bone Joint Surg Am 96(19):e168
Koh IJ, Kim TK, Chang CB, Cho HJ, In Y (2013) Trends in use of total knee arthroplasty in Korea from 2001 to 2010. Clin Orthop Relat Res 471(5):1441–1450
Mahoney OM, Kinsey TL, D’Errico TJ, Shen J (2012) The John Insall Award: no functional advantage of a mobile bearing posterior stabilized TKA. Clin Orthop Relat Res 470(1):33–44
Matsuda S, Mizu-uchi H, Fukagawa S, Miura H, Okazaki K, Matsuda H et al (2010) Mobile-bearing prosthesis did not improve mid-term clinical results of total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 18(10):1311–1316
Mohammed A, Metcalfe A, Woodnutt D (2014) Medium-term outcome of titanium nitride, mobile bearing total knee replacement. Acta Orthop Belg 80(2):269–275
Rhee SJ, Cho JY, Jeung SH, Poon KB, Choi YY, Suh JT (2018) Combined rotational alignment change after total knee arthroplasty in different tibial component designs: implications for optimal tibial component rotational alignment. Knee Surg Relat Res 30(1):74–83
Schotanus MGM, Pilot P, Kaptein BL, Draijer WF, Tilman PBJ, Vos R et al (2017) No difference in terms of radiostereometric analysis between fixed- and mobile-bearing total knee arthroplasty: a randomized, single-blind, controlled trial. Knee Surg Sports Traumatol Arthrosc 25(9):2978–2985
Scott DF, Smith RR (2014) A prospective, randomized comparison of posterior stabilized versus cruciate-substituting total knee arthroplasty: a preliminary report with minimum 2-year results. J Arthroplasty 29(9 Suppl):179–181
Thienpont E (2015) Titanium niobium nitride knee implants are not inferior to chrome cobalt components for primary total knee arthroplasty. Arch Orthop Trauma Surg 135(12):1749–1754
van Hove RP, Brohet RM, van Royen BJ, Nolte PA (2015) No clinical benefit of titanium nitride coating in cementless mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(6):1833–1840
Vertullo CJ, Lewis PL, Graves S, Kelly L, Lorimer M, Myers P (2017) Twelve-year outcomes of an oxinium total knee replacement compared with the same cobalt-chromium design: an analysis of 17,577 prostheses from the australian orthopaedic association national joint replacement registry. J Bone Joint Surg Am 99(4):275–283
Vogt JC, Saarbach C (2009) LCS mobile-bearing total knee replacement. A 10-year’s follow-up study. Orthop Traumatol Surg Res 95(3):177–182
Wasielewski RC, Komistek RD, Zingde SM, Sheridan KC, Mahfouz MR (2008) Lack of axial rotation in mobile-bearing knee designs. Clin Orthop Relat Res 466(11):2662–2668
Wolterbeek N, Garling EH, Mertens B, Valstar ER, Nelissen RG (2009) Mobile bearing knee kinematics change over time. A fluoroscopic study in rheumatoid arthritis patients. Clin Biomech (Bristol Avon) 24(5):441–445
Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G (2011) Differences of knee anthropometry between Chinese and white men and women. J Arthroplasty 26(1):124–130
Zurcher A, van Hutten K, Harlaar J, Poll R (2017) Mobility of the rotating platform in low contact stress knee arthroplasty is durable. Knee Surg Sports Traumatol Arthrosc 25(8):2580–2585
Funding
This research did not recieve any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedrues performed in the present study were in accordance with the ethical standards of the institutional review board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Park, C.H., Kang, S.G., Bae, D.K. et al. Mid-term clinical and radiological results do not differ between fixed- and mobile-bearing total knee arthroplasty using titanium-nitride-coated posterior-stabilized prostheses: a prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 27, 1165–1173 (2019). https://doi.org/10.1007/s00167-018-5095-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5095-z