Abstract
Purpose
The purpose of this study was to assess the variations in tibial tubercle–trochlear groove distance and angle as a function of age and gender in a population of children without patellar instability (PI) compared with those with PI.
Methods
A retrospective review of 869 children’s knee MRIs, ages 5 to 15 years, were evaluated using a control group (792 children) without evidence of PI and a group with PI (77 children). Tibial tubercle–trochlear groove distance (TT–TGd) and angle (TT–TGa) were measured twice by two readers to assess intra- and inter-observer reliability and compared between PI and control groups. In both groups, functions of age and gender on TT–TGd and TT–TGa values were evaluated.
Results
Both TT–TGd and TT–TGa measurements showed excellent intra- and inter-observer reliability. The mean TT–TGd for the PI group was 17.2 mm (SD 6.6) and significantly higher than the mean TT–TGd for the control group (10.4 SD 3.8 mm, P = 0.001). The mean TT–TGa for the PI was 20.8° (SD 8.3°), which was also significantly higher than the mean TT–TGa for the control group (12.5° SD 4.6°, P < 0.001). Control group revealed a positive correlation between age and TT–TGd measurements (r = 0.243, P < 0.001). The mean TT–TGa for girls (13.3° SD 4.7°) was higher than the mean TT–TGa for boys (11.9° SD 4.4°) in the control group (P < 0.001).
Conclusion
TT–TGa and TT–TGd are reliable and can be used for the evaluation of the extansor mechanism alignment in children with and without PI. However, it must be considered that TT–TGd is increasing in growing patients. Soft-tissue procedures may be prone to failure, since bony procedures for patellar alignment cannot be done until skeletal maturity.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellar dislocation is one of the common disorders in children and adolescents with an estimated incidence of 29–43 per 100,000 [7, 12, 16]. Risk factors related to patellar instability can include bone structural changes (trochlear dysplasia, patella alta, lateralization of tibial tubercle, and rotational abnormalities around the knee) and soft tissue factors (weak medial patellofemoral ligament, atrophic vastus medialis obliquus muscle, and conditions associated with generalized ligamentous laxity) [4, 18].
One of the risk factors, lateralization of the tibial tubercle, has been considered as an important element in the assessment and treatment of the patellar instability (PI). The lateralization distance, which was defined as tibial tubercle–trochlear groove distance (TT–TGd), was initially described by Goutallier on axial radiograph of the knees [9]. Later, Dejour et al. used axial computed tomographic (CT) images and improved the reliability of the TT–TGd measurement [4]. By achieving good correlation between magnetic resonance images (MRI) and CT measurements, Schoettle et al. showed that TT–TGd of both cartilaginous and osseous landmarks can be reliably measured on MRI [19].
Hinckel et al. mentioned that the assessment of lateral quadriceps vector only by TT–TGd could be a limited evaluation because of undermining the rotational factors such as internal rotation of the distal femur, external rotation of the tibia or external rotation of the patellar tendon insertion. They stated that angular measurements are more closely associated with patellar instability than TT–TGd [11].
There are few studies that evaluated the effect of age and gender on TT–TGd measurement, and also according to our knowledge, there is no study that searched for the same question on rotational measurements [2, 5, 6]. For this purpose, the study was conducted to assess the angular and distance measurements of lateral quadriceps vector in a large range of age group with no history of PI compared with a group of children with a known history of PI, by also giving a specific focus on age and sex. It was hypothesized that children with patellar instability would have greater values of both distance and rotational measurements and these measurements will also be higher in older and boys than girls.
Materials and methods
All MRI and charts, from the period between January of 2014 and December of 2016, were reviewed to identify the children between 5 and 15 years of age with knee MR images. Children with history of the previous knee surgery, preexisting deformity (skeletal dysplasia, developmental, or acquired angular-rotational deformities), destructive osseous neoplasm, and unreadable MRIs were excluded from the study. 869 children’s MRI views were collected. From them, children with patellar instabilities were identified. The diagnosis of PI was verified through the examination of the medical records (clinical history and related physical examination) or radiological findings (contusion of the lateral femoral condyle or medial portion of the patella, osteochondral fragment, and lesion of the medial patellofemoral ligament). Seventy-seven children (44 left and 33 right knees) had patellar instability. Rest of the cohort (792 children, 393 left and 399 right knees) was selected as control group to evaluate the changes of the measurements according to age and to compare with the knees with PI. The diagnostic indications of MRI in the control group were as follows: knee pain, discoid meniscus and other meniscal lesions, benign neoplasm (e.g. non-ossifying fibroma, osteoid osteoma), Osgood–Schlatter disease, symptomatic plica, and growing pains. None of the control group had any disease history that could affect the patellofemoral morphology.
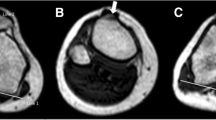
MR images had been performed on a 1.5 T Signa Scanner (General Electric Healthcare, Milwaukee, WI). T2-weighted turbo spin-echo axial knee images were used for evaluation. Measurements were done on a light picture archiving and communications system (PACS) workstation (Koninklijke Philips Electronics, Eindhoven, The Netherlands). TT–TGd was measured as previously described by Schoettle et al. [19]. First, the deepest point of the trochlear groove was identified in the axial craniocaudal image. Then, a line was drawn through the deepest point of the trochlear groove perpendicular to the posterior condyle tangent line (Fig. 1). A second line was drawn parallel to the trochlear line through the middle portion of the patellar tendon at the level of insertion to the tibial tubercle. The distance between these two lines in millimeters represented the TT–TGd. For rotational analysis, tibial tubercle–trochlear groove angle (TT–TGa) was measured as previously described by Hinckel et al. [11]. First, a line was drawn from the deepest point of the trocheal groove to the posterior condyle tangent, similar to the TT–TGd measurement. Then, both lines were transferred to the axial cut, where the patellar tendon was fully inserted to the tibial tubercle. The angle between the both lines starting from trochlear groove and middle point of the patellar tendon insertion to the posterior condyle tangent line–trochlear line intersection point was measured as TT–TGa (Fig. 2).
Patellar tendon-level axial cut: condylar tangent line (1), condylar trochlear line (2), and patellar tendon center and line (3). TT–TGd (**) is the distance measured between condylar trochlear line (2) and patellar tendon line (3). TT–TGa (*) is the angle measured between condylar trochlear line (2) and the line to the patellar tendon center
Two independent readers undertook measurements blindly. With 1 week apart, 50 randomly selected MRI views were measured again to assess the inter- and intra-observer reliability.
This study was approved by Baltalimani Bone Diseases Education and Research Hospital Institutional Review Board (03.08.2017/12) and informed consent was waived, because the study was a retrospective cross-sectional review.
Statistical analysis
Data management was carried out using Microsoft Excel 2007 (Microsoft Redmond,Washington). Statistical analysis was performed using SPSS version 17 (SPSS, Inc., Armonk, NY, USA). Descriptive statistics were given as mean and standart deviations (SD). Normality of the variable distribution was tested with skewness and kurtosis. Categorical variables (gender) were compared with Chi-squared test. Continuous variables (TT–TGd, TT–TGa, and age) were compared using the independent samples t test. Pearson correlation coefficient was used to test for the correlation of age between TT–TGd and TT–TGa in children with and without patellar instability. An intraclass correlation coefficient (ICC) was calculated to assess inter and intra observer reliability. Binary logistic regression model was generated to determine which measurement (TT–TGd or TT–TGa) is most significantly predictive of the presence or absence of patellar instability. Statistical significance was set as P < 0.05. Calculated sample size (effect size 0.8, alpha error 0.05, power 0.95) revealed a minimum of 42 subjects per group.
Results
Agreement within the first and the second measurements for TT–TGd (weighted kappa, 0.986; 95% CI 0.975–0.992; P < 0.001) and TT–TGa (weighted kappa, 0.954; 95% CI 0.921–0.974; P < 0.001) was excellent. Agreement between the two readers for TT–TGd (weighted kappa, 0.939; 95% CI 0.89–0.96; P < 0.001) and TT–TGa (weighted kappa, 0.951; 95% CI 0.89–0.97; P < 0.001) was also excellent.
In the control group, 340 were girls (42.9%) and 452 were boys (57.1%). The overall mean age was 12 (SD 2.8) years. The mean TT–TGd was 10.4 (SD 3.8) mm and the mean TT–TGa was 12.5° (SD 4.6°). The mean age for girls (11 SD2.7 years) and the mean age for boys (11 SD 2.9 years) were similar (n.s.). There was no significant difference in the mean TT–TGd between sexes (girls 10.6 mm SD3.8 vs. boys 10.2 mm SD 3.8, n.s.). However, the mean TT–TGa for girls (13.3° SD 4.7°) was significantly higher than the mean TT–TGa for boys (11.9° SD 4.4°) (P < 0.001). There was a positive modest correlation between age and TT–TGd (r = 0.243, P < 0.001) (Fig. 3). No statistically significant correlation was detected between age and TT–TGa (n.s.) (Fig. 4). To eliminate the age bias during comparison with the PI group, additional correlation analysis between age, TT–TGd and TT–TGa measurements were conducted by extracting the children less than 7 years of age and matching the age range with the PI group. There was still a positive correlation between age and TT–TGd (r = 0.194, P < 0.001). In addition, age and TT-TTGa did not show statistically significant correlation (n.s.).
In the PI group, the overall mean age was 13 (SD 2.1) years. The mean age for girls (12 SD 2.2 years) was slightly lower than the mean age for boys (13 SD 1.8 years, P = 0.046). The mean age for the PI group was statistically significantly higher when compared with the mean age for the control group (P = 0.001).
In the PI group, 40 (51.9%) were girls and 37 (48.1%) were boys and the sex distribution was similar with the control group (n.s.).
The mean TT–TGd for those with PI was 17.2 mm (SD 6.6), which was significantly higher than the mean of 10.4 (SD 3.8) mm for the control group (P = 0.001). The mean TT–TGa for those with PI was 20.8° (SD 8.3°), which was also significantly higher than the mean of 12.5° (SD 4.6°) for the control group (P < 0.001) (Table 1).
In the PI group, there was no significant difference in the mean TT–TGd (girls 16 mm SD 6.4 vs. boys 18.5 mm SD 6.6, n.s.) between sexes. In addition, no significant difference was observed in the mean TT–TGa (girls 20.3° SD 8.8° vs. boys 21.3° SD 7.7°, n.s.) between sexes. No statistically significant correlations were observed between age and TT–TGd (n.s.) and also between age and TT–TGa (n.s.) measurements in the PI group.
Assessment of the both TT–TGd and TT–TGa measurements by a logistic regression model revealed similar amounts of odd ratios for the prediction of patellar instability (Table 2).
Discussion
The most important findings of the presented study were between 5 and 15 years of age: (1) TT–TGd showed a positive correlation with age; (2) TT–TGa values in all ages are showing consistency; (3) gender has no effect on TT–TGd measurements; and (4) TT–TGd and TT–TGa reveal similar amount of odd ratios in predicting patellar instability.
Surgical management for patients with patellar instability is mainly based on lateral quadriceps vector malalignment. TT–TGd measurement is often used as an objective tool for the assessment [3]. In the present study, children with PI showed higher TT–TGd than a normal control group (P = 0.001). We found that the mean TT–TGd of our control group was 10.4 (SD 3.8) mm. This was consistent with the previous studies that have similar age group of patients with TT–TGd means ranging from 8.6 to 11.7 mm [1, 5, 6, 18]. In the literature, there is contradiction in regards of age effect on TT–TGd measurements. First, Balcarek et al. reported that in a patient sample of young athletes, age did not correlate with TT–TGd. Several studies have also supported the same finding afterwards [1, 6, 18]. However, the study of Dickens et al., which TT–TGd was calculated from an age group of infancy to 16 years, showed that TT–TGd is advancing with age and increasing toward skeletal maturity. Dickens et al. suggested that it might be appropriate to devise an age-based approach for evaluating children with recurrent patellar instability [5]. Although having the largest sample size and a good age range compared to the current literature, our study was not conducted to assess the children less than 5 years of age, since PI is uncommon under this age group except for congenital causes. However, the present study also showed a modest positive correlation between age and the TT–TGd in the control group (r = 0.243, P < 0.001).
In the study of Pennock et al., age showed a negative correlation with TT–TGd in PI group. They suggested that this could be explained by the fact that older patients sustain higher energy involving injuries than younger patients [18]. Although the present study had a larger sample size of PI patients than the study of Pennock et al., no correlation was detected between age and TT–TGd measurements (n.s.).
In the literature, for the evaluation of rotational patellofemoral alignment, several radiological measurements have been described [11, 13, 14, 20]. We chose TT–TGa measurement, because of being a simple and easy applicable technique in immature knee. The present study showed excellent inter- and intra-rater reliability for the TT–TGa measurement. In the control group, TT–TGa was (mean 12.5° SD 4.6°) significantly lower than the PI group (mean 20.8° SD 8.3°, P < 0.001). In addition, unlike TT–TGd, TT–TGa did not correlate with age and average values of each age group remained similar with the mean of the total control cohort (Table 1). In the control group, average TT–TGa values for girls were higher than that of boys with a mean difference of 1.4°, which was consistent with the study of Hinckel et al. [11]. However, further studies are needed to evaluate the clinical relevance of such low value of angular difference.
For the treatment of PI, skeletal immaturity limits the surgical options as osteotomies around the knee due to increased risk of growth plate injuries [2, 10]. In skeletal immature children with diseases related to patellofemoral alignment disorders, several soft-tissue procedures have been developed in an effort to avoid these complications [8, 15, 17]. However, soft-tissue surgeries may be prone to failure, since the structural deformity (increased TT–TGd) of the patellar alignment cannot be changed until skeletal maturity. Control data of this study can be used for further studies with having both angular and distant measurements of tibial tubercle–trochlear groove in descent amount of children between 5 and 15 years of age. In addition, as a clinical importance of this study, the data showed that tibial tubercle–trochlear groove distance could be affected by age. As Dickens et al. suggested, for better assessment, TT–TGd can be evaluated according to the chronological age, or as another option, TT–TGa can be used.
There are some limitations of the present study. First, due to being a retrospective chart review, the skeletal age and growth metrics of the children (lower limb length, weight etc.) could not be collected. However, it is accepted that growth metrics are routinely associated with chronological age [5]. Second, ideal control group might be healthy subjects. For that reason, special attention was paid to collect the subjects with MRI without a known disease history that could affect the patellofemoral alignment. Third, in the control group, there were fewer patients in younger age group than older age groups. However, according to our knowledge, current study has the largest control group population in the literature. And last, clinical or radiological rotational measurements of the subjects could not be collected to show correlations with TT–TGa measurements.
For the treatment of PI, special attention must be paid to patellar alignment. Clinicians must consider that in children with PI, TT–TGd, and TT–TGa are higher than normal pediatric population. Measurement of TT–TGd or TT–TGa can save the surgeons from inadequate surgical treatment or help them to plan further intervention after skeletal maturity.
Conclusion
This study is a guide for further investigation into the role of rotational and axial distant measurements of patellofemoral alignment for evaluating skeletally immature individuals with recurrent patellar instability. Both measurement techniques are reliable tools and can be used for the evaluation of children with and without PI. However, it must be considered that TT–TGd is increasing in growing patients.
References
Askenberger M, Janarv PM, Finnbogason T, Arendt EA (2017) Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations: a prospective magnetic resonance imaging study in skeletally immature children. Am J Sports Med 45:50–58
Balcarek P, Jung K, Frosch KH, Sturmer KM (2011) Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med 39:1756–1761
Dejour D, Le Coultre B (2007) Osteotomies in patello-femoral instabilities. Sports Med Arthrosc 15:39–46
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Dickens AJ, Morrell NT, Doering A, Tandberg D, Treme G (2014) Tibial tubercle–trochlear groove distance: defining normal in a pediatric population. J Bone Joint Surg Am 96:318–324
Duppe K, Gustavsson N, Edmonds EW (2016) Developmental morphology in childhood patellar instability: age-dependent differences on magnetic resonance imaging. J Pediatr Orthop 36:870–876
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA et al (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Gordon JE, Schoenecker PL (1999) Surgical treatment of congenital dislocation of the patella. J Pediatr Orthop 19:260–264
Goutallier D, Bernageau J, Lecudonnec B (1978) [The measurement of the tibial tuberosity. Patella groove distanced technique and results (author’s transl)]. Rev Chir Orthop Reparatrice Appar Mot 64:423–428
Hennrikus W, Pylawka T (2013) Patellofemoral instability in skeletally immature athletes. Instr Course Lect 62:445–453
Hinckel BB, Gobbi RG, Kihara Filho EN, Demange MK, Pecora JR, Camanho GL (2015) Patellar tendon-trochlear groove angle measurement: a new method for patellofemoral rotational analyses. Orthop J Sports Med 3:2325967115601031
Kuroda R, Nagai K, Matsushita T, Araki D, Matsumoto T, Takayama K et al (2017) A new quantitative radiographic measurement of patella for patellar instability using the lateral plain radiograph: ‘patellar width ratio’. Knee Surg Sports Traumatol Arthrosc 25:123–128
Muneta T, Yamamoto H, Ishibashi T, Asahina S, Furuya K (1994) Computerized tomographic analysis of tibial tubercle position in the painful female patellofemoral joint. Am J Sports Med 22:67–71
Nagamine R, Miura H, Inoue Y, Tanaka K, Urabe K, Okamoto Y et al (1997) Malposition of the tibial tubercle during flexion in knees with patellofemoral arthritis. Skeletal Radiol 26:597–601
Nelitz M, Theile M, Dornacher D, Wolfle J, Reichel H, Lippacher S (2012) Analysis of failed surgery for patellar instability in children with open growth plates. Knee Surg Sports Traumatol Arthrosc 20:822–828
Nietosvaara Y, Aalto K, Kallio PE (1994) Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 14:513–515
Novacheck TF, Stout JL, Gage JR, Schwartz MH (2009) Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. Surgical technique. J Bone Joint Surg Am 91(Suppl 2):271–286
Pennock AT, Alam M, Bastrom T (2014) Variation in tibial tubercle-trochlear groove measurement as a function of age, sex, size, and patellar instability. Am J Sports Med 42:389–393
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J (2006) The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13:26–31
Tsujimoto K, Kurosaka M, Yoshiya S, Mizuno K (2000) Radiographic and computed tomographic analysis of the position of the tibial tubercle in recurrent dislocation and subluxation of the patella. Am J Knee Surg 13:83–88
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Ethical approval
This study was approved by Baltalimani Bone Diseases Education and Research Hospital Institutional Review Board (03.08.2017/12).
Informed consent
Informed consent was waived, because the study was a retrospective cross-sectional review.
Rights and permissions
About this article
Cite this article
Bayhan, I.A., Kirat, A., Alpay, Y. et al. Tibial tubercle–trochlear groove distance and angle are higher in children with patellar instability. Knee Surg Sports Traumatol Arthrosc 26, 3566–3571 (2018). https://doi.org/10.1007/s00167-018-4997-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4997-0