Abstract
Purpose
The aim of this study was to assess the progression of radiological cartilage changes and to document the functional, long-term results during a follow-up of 10 years after osteoautograft transplantation (OAT) knee surgery.
Methods
The study was a retrospective analysis of all patients who underwent OAT at Turku University Hospital from 1999 to 2007. Pre- and postoperative cartilage changes were estimated based on standardised radiographs. The extent of osteoarthritis (OA) was graded according to the Kellgren–Lawrence scale. Clinical outcomes were evaluated with the Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaire.
Results
A total of 60 patients (64 knees) with a median age of 30 years (range 14–62) were included. The median follow-up was 140 months (range 47–205). Of the 64 knees examined, 14 (22%) had a traumatic chondral lesion and 50 (78%) had osteochondritis dissecans (OCD). Preoperatively, 71% of the patients had Kellgren–Lawrence grades of 0–1; during the follow-up period, 50% of the patients showed radiographical progression of OA. OA progressed most significantly in patients with normal preoperative Kellgren–Lawrence grades (p = 0.0003). Patients with no progression in joint space narrowing had statistically significantly better overall KOOS (p = 0.02) than patients whose Kellgren–Lawrence grades worsened. Patients with defect sizes > 3.0 cm2 scored statistically significantly better in all subscales than patients with smaller defect sizes (p = 0.02). Patients with OCD had statistically significantly better KOOS than patients with chondral defects (p = 0.008).
Conclusions
OAT surgery for treating patients with cartilage defects of the knee had good clinical results after a mean follow-up of 11 years. Radiological analyses revealed a progression of cartilage degeneration in 50% of the operated knees. Patients with no progression of the degenerative changes scored statistically significantly better on the KOOS self-assessment test. These results indicate that OAT surgery appears to be a reasonable therapeutic option to restore knee function in patients with cartilage lesions.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
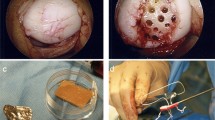
Injured articular cartilage has a limited ability to regenerate, and full-thickness lesions may contribute to the development of osteoarthritis (OA) [12, 16]. However, the best method for repairing full-thickness cartilage defects remains a great debate, and a number of different treatment options have been used to address this injury with variable success rates [2]. In this context, the osteoautograft transplantation (OAT) involves the transfer of a healthy osteochondral plug from minimally weight-bearing portions of the femur to a small- or medium-sized focal chondral or osteochondral defect in high weight-bearing regions. Depending on the size of the defect, additional donor plugs can be placed next to each other to fill the defect. OAT aims to capitalise on bone-to-bone healing because mature cartilaginous tissue has limited healing potential, and the transferred cartilage surface heals by fibrocartilaginous repair to the surrounding articular tissue. This technique has the advantage of resurfacing the defect with normal hyaline cartilage, but has the disadvantage of leaving an articular cartilage defect in another location in the treated knee. Nevertheless, good short- and intermediate-term outcomes have been reported with the use of the OAT system [5, 8, 9, 11, 13, 15, 20].
Based on previously reported results on the long-term natural course of knee cartilage defects, the study hypothesis was that, by utilising OAT surgery, it is possible to achieve good functional results with an acceptable rate of knee OA progression even after 10 years of follow-up. Thus, the aim of this study was twofold: (a) to assess the progression of radiological cartilage changes and (b) to document the functional, long-term results during a follow-up period of 10 years after OAT knee surgery.
Materials and methods
The study design is a retrospective analysis of an historical cohort identified with the current NGF40 procedural terminology code from the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) and confirmed with a retrospective review of medical records. Altogether, 71 patients underwent OAT at Turku University Hospital from 1999 to 2007. At the time of the follow-up, two patients were found to have died, eight patients could not be contacted and one patient declined to participate, leaving 60 patients in the study cohort. The information retrieved from the medical charts included patient characteristics, knee symptoms and surgical details related to the cartilage injuries. In addition, the preoperative knee standing radiographs and knee magnetic resonance imaging (MRI) were retrieved from the radiology database for further analyses.
Knee radiographs with the knee in a semi-flexed (20°) position (standing PA, lateral and mechanical axis) were required for all study participants, who were asked to complete the Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaire. The KOOS is a self-reported assessment tool consisting of 42 questions distributed among five separately scored subscales: symptoms, pain, activities of daily living (ADL), function in sport and recreation (sport) and knee-related quality of life (QoL). A score ranging from 0 to 100, where 100 represents the best result, is calculated for each subscale [18].
Pre- and postoperative cartilage changes were estimated on standardised radiographs by two independent observers, one orthopaedic surgeon (EE) and one musculoskeletal radiologist (IK) using the Kodak Carestream PACS system workstation (version 11.4; Carestream Health, Rochester, NY, USA). The extent of OA of the knee was graded according to the Kellgren–Lawrence OA scale. Scores are not compartment specific; therefore, a patient with a grade-3 change in the patellofemoral compartment who underwent an OAT procedure on the medial compartment was still recorded as having a grade-3 change. The mechanical alignment of the leg was assessed on full-length, weight-bearing radiographs within an accuracy of one degree by an experienced musculoskeletal radiologist (IK). Knee MR studies were used to obtain a more detailed estimate of degenerative cartilage changes in the knee before the operation and to determine, within an accuracy of 1 mm, the size, depth and location of the defect by the same radiologist (IK). The majority of MR studies were obtained using 1.5 T MRI scanners; three studies were performed using low magnetic field equipment. For the patients who did not have a preoperative MR study (n = 27), preoperative radiographs and medical records from their operations were used to determine the size and location of the defects. The study was approved by the Regional Ethical Review Board in Turku (Dnro TO1/003/14).
Statistical analysis
Relationships between the KOOS total and independent variables (gender, aetiology of defect, size of the defect, duration of symptoms, knee alignment axis, concomitant procedures, Kellgren–Lawrence grade from the preoperative radiographs, Kellgren–Lawrence grade from the postoperative radiographs and a variable indicating a change between the Kellgren–Lawrence grade from the preoperative radiographs and the Kellgren–Lawrence grade from the postoperative radiographs) were studied with descriptive statistics, correlation, Fisher’s exact test and a multi-way analysis of variance (ANOVA). KOOS subscales (pain, symptoms, ADL, sport and QoL) were also used as dependent variables. The normality of variables was evaluated visually and tested with the Shapiro–Wilk test. Nonparametric methods were used due to the skewness of the continuous variables. Spearman’s correlation was used to examine two continuous variables, and the Kruskal–Wallis test was used to compare groups of two or more variables. Due to small frequencies, Fisher’s exact test was used to study two categorical variables. The main analysis was completed via a multi-way ANOVA. The KOOS total was used as a dependent variable, and defect size, gender and change in the Kellgren–Lawrence grade were included as factors. Change in the Kellgren–Lawrence grade was used as a two-class variable to examine the mean difference between patients whose cartilage injuries had worsened and those whose injuries had remained the same. The statistical significance level was set at 0.05 in all tests (two tailed). The analyses were performed using the SAS system, version 9.4 for Windows (SAS Institute Inc., Cary, NC, USA).
Results
A total of 60 patients (64 knees) with a median age of 30 years (range 14–62) were included in the study analysis. Characteristics of the study cohort and lesion location and size are summarised in Table 1. The median follow-up period after OAT surgery was 140 months (range 47–205). Of the 64 knees examined, 14 (22%) had traumatic chondral lesions, and 50 (78%) of the cartilage lesions were osteochondritis dissecans (OCD) lesions extending significantly (> 5 mm) to the subchondral bone. The median size of the defects was 2.6 cm2 (0.6–7.8 cm2). Of the 60 patients, 25% had combined procedures related to OAT surgery, and, during the follow-up period, additional surgery was performed on 28% of the knees (Table 2).
Preoperatively, 71% of the patients did not have any significant cartilage degeneration (Kellgren–Lawrence grades of 0–1); at the time of follow-up, 50% of the patients showed radiographical progression of joint space narrowing (at least one grade level on the Kellgren–Lawrence scale) (Table 3). Most commonly, the progression of joint space narrowing was one grade compared to zero or two grades (p = 0.0018). No patient had joint space narrowing by three or four grades. OA progressed mostly in patients with normal preoperative Kellgren–Lawrence grades (p = 0.0003). All patients whose Kellgren–Lawrence grades worsened by two grades had normal preoperative Kellgren–Lawrence grades.
The KOOS at the final follow-up for the different defect sizes and different Kellgren–Lawrence grades (both preoperative and postoperative) is given in Fig. 1 and Table 3. Furthermore, the final KOOS related to the grade of joint space narrowing is shown in Table 3. There were no statistically significant differences in the KOOS self-assessment test among patients whose Kellgren–Lawrence grade worsened by one or two grades. Therefore, we compared patients with no change in their Kellgren–Lawrence grades and patients with a change in their Kellgren–Lawrence grades of one or two grades. Patients with no progression in joint space narrowing had statistically significantly better overall KOOS (p = 0.02) than patients whose Kellgren–Lawrence grades worsened. In terms of the KOOS subscales, however, this was true only with symptoms (p = 0.003), ADL (p = 0.01) and quality of life (p = 0.04). There were no statistically significant differences in the subscales pain (n.s.) and sport (n.s.).
Patients with defect sizes > 3.0 cm2 scored statistically significantly better in all subscales than patients with smaller defect sizes (p = 0.02). Two patients had remarkably low KOOS; however, the statistical significance remained even after exclusion of these two patients (p = 0.02). When evaluating only patients with OCD, the connection between the size of the defect and a better clinical outcome remained statistically significant (p = 0.02). The size of the defect did not influence the progression of the Kellgren–Lawrence grade (n.s.).
Patients with OCD had statistically significantly better KOOS than patients with chondral defects (p = 0.008). Progression of OA (worsening of the Kellgren–Lawrence grade) at the final follow-up was observed in 47% of the patients with OCD and in 70% of the patients with chondral defects. Women tended to have better KOOS than men; however, this difference was not statistically significant. The average KOOS was 84% for women and 76% for men. This tendency remained even after adjusting the groups for age and the aetiology of the defect (OCD versus chondral defect).
Preoperative duration of symptoms (n.s.), knee alignment axis (n.s.) and concomitant surgical procedures during OAT procedure (n.s.) had no effect on outcome (KOOStotal or progression of radiological cartilage changes, respectively).
Discussion
The main finding of the present study is that utilising OAT surgery for treating patients with cartilage defects of the knee showed good clinical results during long-term follow-up, and 50% of the patients showed no radiographical progression of cartilage degeneration. Data from 60 symptomatic patients (64 knees) who underwent OAT surgery for focal cartilage lesions were analysed. The mean functional scores of the KOOStotal were 80 at a mean follow-up of 11 years and 2 months after OAT surgery. After OAT surgery, 50% of the study patients showed no progression of radiological OA during post-OAT follow-up. Patients with defect sizes > 2.5 cm2 had higher clinical outcome scores compared to patients with defect sizes < 1.5 cm2. To the best of our knowledge, this is the largest series of patients reporting radiological and functional outcomes of OAT surgery with more than 10 years of follow-up.
The long-term results of untreated focal cartilage defect of the knee have been shown to be unsatisfying, with a high percentage of radiological OA progression [1, 19]. It has been shown that a defect in the weight-bearing surface of the knee causes increased local mechanical stress, which might lead to increased wear of the surrounding cartilage [7]. In this context, there are promising reports of clinical outcomes after OAT procedures [5, 8, 11, 13, 15, 20, 21]; however, for small chondral lesions, less invasive methods such as microfracture might be considered, i.e. to avoid harvest site symptoms. Promising short-term results have been reported with microfracture, but long-term results have been less predictable [14, 22].
Studies reporting the possible progression of OA of the operated knee joint after OAT surgery are limited and generally include small numbers of patients [5, 15, 23]. Gudas et al. reported a study of 28 patient athletes less than 40 years of age with symptomatic cartilage lesions of the knee. At the 10-year follow-up, 25% (n = 7) of the patients had progression of cartilage wear that was at a level of Kellgren–Lawrence grade 1. In the study, the progression of OA did not influence the final functional outcome (ICRS score) [4, 5]. Ulstein et al. reported a radiological study of 14 patients who had OAT surgery with a median follow-up of 9.8 years [23]. None of the study patients had OA changes (Kellgren–Lawrence of 0) preoperatively, but 17% of the patients had a progression of OA (Kellgren–Lawrence ≥ 2) at the time of follow-up. In our study, we found that half of the patients who underwent an OAT procedure for their cartilage defects had a worsening of one or two grades on the Kellgren–Lawrence scale. Based on our results, it seems that even mild/moderate radiographical progression is related to worsening of the functional results. Study patients with no progression in their Kellgren–Lawrence grades had excellent functional results (KOOStotal of 87%), whereas patients with a one or two grade progression on the Kellgren–Lawrence scale experienced worsening of the functional scores (KOOStotal of 71 and 73%, respectively).
The size of the cartilage defect seems to be a factor affecting the final outcome after OAT surgery. However, the results of previous studies have been contradictory because they have found that either there is no association between defect size and clinical outcome at a 4-year follow-up [5, 6], or that smaller lesions correlate with better functional outcomes at a 7-year follow-up [13]. Interestingly, our results showed that patients with a mean defect size > 3.0 cm2 scored statistically significantly better in all KOOS subscales than patients whose defect sizes were smaller (< 1.5 cm2). This finding might be explained by the selection bias: It is more likely that the knee symptoms are due to the cartilage issues in the case of a large defect size, and that the risk of other origins for knee symptoms theoretically increases with a cartilage defect of a small size.
In the subgroup analysis of our study results, we found that the preoperative size of the cartilage defect did not influence the rate of OA progression. However, Filardo et al. found that knees implanted with three to four plugs (larger lesions) presented a significantly higher OA progression rate, compared with those treated with one or two plugs (smaller lesions). Also, no significant correlation between inferior radiographical findings and clinical outcome (IKDC) was found [3]. The comparison of OA progression was made between index and contralateral knees, and no preoperative radiographs were available for the radiological analysis. Further, in our series, the patients with OCD had statistically significantly better KOOS and less progression of OA (worsening in the Kellgren–Lawrence grade) at the final follow-up. We found no difference in clinical outcomes between female and male patients. Kramer et al. reported that women have statistically significantly more pain after the OAT procedure for OCD of the patella or trochlea at a 1–9 year follow-up. Females had nine times the odds of reporting either mild residual pain or pain similar to that experienced preoperatively [10].
During the follow-up, two knees with prior OAT surgery were converted to arthroplasty (one total knee arthroplasty and one unicondular knee arthroplasty). Both of these patients were female, and they were 42 and 45 years of age, respectively, at the time of the index surgery. A recent systematic review identified female sex and increased age at the time of the surgery as risk factors for failure [17]. Furthermore, in both patients, the preoperative cartilage status was classified as Kellgren–Lawrence grade 2, and the indication for the OAT surgery was chondral lesion, without any significant subchondral bone damage. Thus, it can be assumed that the underlying disease was, in fact, OA and that the OAT failed because the procedure cannot change the natural course of the disease. The clinical relevance of the present study is that OAT surgery offers good clinical results especially for patients with large OCD lesions in their knees.
Some limitations in our study design require consideration. Our data were collected in a retrospective manner; thus, the initial patient-reported outcome measures were not available for the comparison of clinical outcomes. In addition, not all patients who underwent surgery agreed to participate in the present study, and, theoretically, this may have biased the results because the dropouts may have had well functioning as well as poorly functioning knees. The lack of a control group and the short-term follow-up preclude definite conclusions regarding the benefits of OAT in treating cartilage defects of the knee. However, our series included a uniquely large number of OAT patients with clinical outcomes and radiological long-term follow-up.
Conclusions
OAT surgery for patients with cartilage defects of the knee had good clinical results after a mean follow-up of 11 years. However, the radiological analyses revealed a mild or moderate progression of cartilage degeneration in 50% of the operated knees. As expected, the progression of radiological cartilage changes was related to a worsening of the functional scores.
References
Anderson AF, Pagnani MJ (1997) Osteochondritis dissecans of the femoral condyles. Long-term results of excision of the fragment. Am J Sport Med 25:830–834
Biant LC, McNicholas MJ, Sprowson AP, Spalding T (2015) The surgical management of symptomatic articular cartilage defects of the knee: consensus statements from United Kingdom knee surgeons. Knee 22:446–449
Filardo G, Kon E, Perdisa F, Tetta C, Di Martino A, Marcacci M (2015) Arthroscopic mosaicplasty: long-term outcome and joint degeneration progression. Knee 22:36–40
Gudas R, Gudaite A, Pocius A, Gudiene A, Cekanauskas E, Monastyreckiene E, Basevicius A (2012) Ten-year follow-up of a prospective, randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint of athletes. Am J Sports Med 40:2499–2508
Gudas R, Kalesinskas RJ, Kimtys V, Stankevicius E, Toliusis V, Bernotavicius G, Smailys A (2005) A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy 21:1066–1075
Gudas R, Simonaityte R, Cekanauskas E, Tamosiūnas R (2009) A prospective, randomized clinical study of osteochondral autologous transplantation versus microfracture for the treatment of osteochondritis dissecans in the knee joint in children. J Pediatr Orthop 29:741–748
Guettler JH, Demetropoulos CK, Yang KH, Jurist KA (2004) Osteochondral defects in the human knee: influence of defect size on cartilage rim stress and load redistribution to surrounding cartilage. Am J Sports Med 32:1451–1458
Hangody L, Dobos J, Balo E, Panics G, Rudolf Hangody L, Berkes I (2010) Clinical experiences with autologous osteochondral mosaicplasty in an athletic population: a 17-year prospective multicenter study. Am J Sports Med 38:1125–1133
Hangody L, Fules P, Füles P (2003) Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am 85–A Suppl:25–32
Kramer DE, Yen Y-M, Simoni MK, Miller PE, Micheli LJ, Kocher MS, Heyworth BE (2015) surgical management of osteochondritis dissecans lesions of the patella and trochlea in the pediatric and adolescent population. Am J Sports Med 43:654–662
Krych AJ, Harnly HW, Rodeo SA, Williams RJ (2012) Activity levels are higher after osteochondral autograft transfer mosaicplasty than after microfracture for articular cartilage defects of the knee: a retrospective comparative study. J Bone Joint Surg Am 94:971–978
Loken S, Heir S, Holme I, Engebretsen L, Aroen A (2010) 6-year follow-up of 84 patients with cartilage defects in the knee. Knee scores improved but recovery was incomplete. Acta Orthop 81:611–618
Marcacci M, Kon E, Delcogliano M, Filardo G, Busacca M, Zaffagnini S (2007) Arthroscopic autologous osteochondral grafting for cartilage defects of the knee: prospective study results at a minimum 7-year follow-up. Am J Sports Med 35:2014–2021
Mithoefer K, Williams RJ, Warren RF, Potter HG, Spock CR, Jones EC, Wickiewicz TL, Marx RG (2005) The microfracture technique for the treatment of articular cartilage lesions in the knee. A prospective cohort study. J Bone Joint Surg Am 87:1911–1920
Muller S, Breederveld RS, Tuinebreijer WE (2010) Results of osteochondral autologous transplantation in the knee. Open Orthop J 4:111–114
Murray JRD, Chitnavis J, Dixon P, Hogan NA, Parker G, Parish EN, Cross MJ (2007) Osteochondritis dissecans of the knee; long-term clinical outcome following arthroscopic debridement. Knee 14:94–98
Pareek A, Reardon PJ, Maak TG, Levy BA, Stuart MJ, Krych AJ (2016) Long-term outcomes after osteochondral autograft transfer: a systematic review at mean follow-up of 10.2 years. Arthrosc J Arthrosc Relat Surg 32:1174–1184
Roos EM, Toksvig-Larsen S (2003) Knee injury and Osteoarthritis Outcome Score (KOOS)—validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1:17
Sanders TL, Pareek A, Obey MR, Johnson NR, Carey JL, Stuart MJ, Krych AJ (2017) High rate of osteoarthritis after osteochondritis dissecans fragment excision compared with surgical restoration at a mean 16-year follow-UP. Am J Sports Med 45:1799–1805
Smolders JMH, Kock NB, Koeter S, Van Susante JLC (2010) Osteochondral autograft transplantation for osteochondritis dissecans of the knee preliminary results of a prospective case series. Acta Orthop Belg 76:208–218
Solheim E, Hegna J, Strand T, Harlem T, Inderhaug E (2018) Randomized study of long-term (15–17 years) outcome after microfracture versus mosaicplasty in knee articular cartilage defects. Am J Sport Med 46:826–831
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (2003) Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthrosc J Arthrosc Relat Surg 19:477–484
Ulstein S, Årøen A, Røtterud JH, Løken S, Engebretsen L, Heir S (2014) Microfracture technique versus osteochondral autologous transplantation mosaicplasty in patients with articular chondral lesions of the knee: a prospective randomized trial with long-term follow-up. Knee Surg Sports Traumatol Arthrosc 22:1207–1215
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AI designed and coordinated the study and helped to draft the manuscript. EE collected the data, drafted the manuscript and studied the patients’ X-rays. IK studied the patients’ X-rays and MRIs. KM, AH, AI and EE contributed to the interpretation of the data and results and to the preparation of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
Regional Ethical Review Board approval was obtained from the Regional Ethical Review Board in Turku (Dnro TO1/003/14) prior to initiation of this study.
Rights and permissions
About this article
Cite this article
Ekman, E., Mäkelä, K., Kohonen, I. et al. Favourable long-term functional and radiographical outcome after osteoautograft transplantation surgery of the knee: a minimum 10-year follow-up. Knee Surg Sports Traumatol Arthrosc 26, 3560–3565 (2018). https://doi.org/10.1007/s00167-018-4995-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4995-2