Abstract
Purpose
Scientific injury data in men’s professional team handball injuries are rare and even less scientific information exists on injury prevention. In 2011, Germany’s national second team handball league was restructured by merging the existing two regional leagues into one league. This study evaluates the injury patterns in professional team handball and compares the injury rates between the first and second league before and after the restructure.
Methods
All players of Germany’s national first and second men’s team handball leagues have mandatory trauma insurance with the same insurance company. This retrospective cohort study analysed the injury data of three consecutive seasons 2010–2013 using standardized injury definitions.
Results
1194 professional team handball players were included in this study. The majority of severe injuries affected the lower extremities, shoulders, and hands. The average injury incidence significantly differed between the first (4.9 injuries per 1000 h) and the second league (3.9 per 1000 h, p < 0.01). The injury incidence in the restructured second league had increased from 3.7 to 4.1 per 1000 h (p < 0.01) and prevalence from 67.1 to 79.3% (p < 0.001), thus almost to the same levels of the first league. The second league showed more time-loss injuries at all severity levels.
Conclusion
This study yielded a high injury incidence after the restructure of the national second team handball league and presents details on prevalence, incidence, and patterns of injury in professional men’s team handball. This study is an important basis for developing injury prevention strategies that should focus on the shoulders, hands, and lower extremities and on reducing the number of matches and travel burden.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Team handball is one of the most popular types of sports in Europe. The game is governed by the International Handball Federation (IHF), founded in 1946 and was introduced to the Summer Olympics in 1972. Currently, approximately 170 members of the IHF include 795,000 teams and an estimated 25 million players worldwide. The game is played by two teams, each consisting of six field players, one goalkeeper, and seven substitutes. Team handball is a dynamic and physically demanding sport, particularly because of the intensive body contact between the players. The increase in game speed, the numbers of matches, and athleticism imposes a high demand on the musculoskeletal system and carries a high risk of injury. However, only a few recent studies on injuries in professional men’s team handball have been published in recent years [5, 6, 11, 13, 16, 17, 19, 20, 22, 24, 25, 27].
In 2011, Germany’s national second league consisting of 18 teams in two regional leagues was restructured to one league with 20 teams. In football, the implementation of a new professional league had increased the rate of ACL and PCL injuries but no data for team handball have been available so far [15]. The purpose of this study was to identify the focus points of injury prevention strategies to decrease injury rates at a national level. Based on previous findings, it was hypothesized that the restructure of the national second team handball league has increased injury incidence [15].
Materials and methods
This retrospective study covered three consecutive German handball seasons from 1 July 2010 to 30 June 2013 and included all professional male handball players who had a contract with one of the first or second league teams and had played at least one official match for their team in one of three seasons. Players who had not participated in any official handball match were excluded.
Injury documentation and data collection
In Germany, all professional athletes are registered with the same insurance company, the German Statutory Accident Insurance (Verwaltungs-Berufsgenossenschaft, VBG). Their database, that had been shown eligible in sports injury research, was used to obtain data on injury in professional men’s team handball [3, 4, 7, 23]. Players who sustain an injury have to present to the responsible physician, in most cases the team physician, who reports the injury data to the VBG. By German law, the VBG has to be informed on every injury with a time-loss of more than three days. In the case of injuries with lesser time loss, sports physicians are advised to report such injuries to the VBG. The injury reports are subsequently coded and electronically registered by the insurance company. Therefore, data collection was identical for all players.
The league, club, nationality, age, height, weight, body-mass index, and field position of each player were documented according to the data obtained from the database of the VBG. Missing data were completed for each season by means of print and online media. For each team, the number of official matches, i.e. the matches in the national first or second league, the German Cup, the EHF-Cup, the Champions League, and the German national team matches, were collected using the electronic match reports of the databases of the German handball league (Handball Bundesliga), SIS-Handball (GateCom GmbH), and the European Handball Federation (EHF). Foreign national matches were excluded. Match exposure was calculated by means of the following formula: number of games × 14 players × 1 h. Data on the training exposure of individual players or teams were not available. Training exposure was therefore calculated by means of the personal experience in both handball training methods and volume of the junior and senior author as a former handball players and current team coaches. This calculation comprised 45 weeks of playing handball per season with an average training volume of 12 h per week.
Injury definition
Injuries were classified into training-related and match-related injuries depending on the date of the reported injury. Without any further information, injuries sustained on competitive match days were registered as match-related injuries and injuries occurring on non-match days as training-related injuries. Injuries were further classified into injuries requiring medical attention and injuries resulting in subsequent time loss. For medical attention injuries, the player had to require treatment by a medical doctor. Any injury disallowing a player’s participation in future training session or match was defined as time-loss injury [8]. The severity of a time-loss injury was based on the duration of the inability to play handball. Time loss injuries were subdivided into slight (1–3 days), mild (4–7 days), moderate (8–28 days), and severe injuries (> 28 days) [Fuller].
Every injury without a code of the specific time loss was classified as injury severity unknown. Injury incidence was defined as injuries in 1000 h (h) of handball exposure per player [8].
No ethics approval was required because of the retrospective study design and the use of anonymized data.
Statistical analysis
Continuous data are expressed as mean and standard deviation (SD) and categorical data as frequency counts (percentages). Proportions between two groups were compared with the Fisher’s exact test and continuous variables with an exact test based on the Poisson distribution. Corresponding 95% confidence intervals (CI) are reported. The significance level was set to p < 0.05 and high significance to p < 0.01. No sample size was calculated for investigating the injury incidence because the aim of the study was to include all players from both national leagues for the seasons before and after the restructure. All analyses were done using IBM SPSS Statistics, version 22.
Results
Over the three consecutive seasons 1194 players participated in official handball matches: 549 players in the national first league and 828 in national second league. 183 of these 828 players had played in both leagues and 645 (54%) only in the second league. The two groups showed similar anthropometric data. First league players were slightly older (in years: 25.8 ± 5.3 vs. 24.8 ± 5.3), taller (in cm: 191.3 ± 6.6 vs. 189.5 ± 6.7), and heavier (in kg: 93.2 ± 8.9 vs. 90.7 ± 9.5) with a higher BMI (in kg/(m2) 25.4 ± 1.6 vs. 25.1 ± 1.8).
930 of the 1194 players had sustained 5456 injuries, which represents a prevalence rate of 77.9% and an incidence rate of 4.3 injuries per 1000 h per player over the complete observation period. Acute injuries were the most common type of injury with 88.8% and the lower extremities (52.0%) including knees (13.8%) and ankles (12.8%) were the most commonly affected. The body sites mostly affected by severe injuries were the shoulders, the hands, and the lower extremities and the most common type of injury were contusions (27.1%) and sprains (26.5%) (Tables 1, 2). 56.0% of all injuries were medical attention injuries (Table 3).
Players in the first league sustained more often medical attention injuries than players in the second league, whereas time-loss injuries of all severity levels were more common in the second league (Table 3). Overall, 7.6% of all injuries resulted in time-loss of more than 28 days (Table 3). Fractures, ruptures, and dislocations occurred more often in the second league (Table 4). 1.0% more overuse injuries occurred in the first league (11.7%) than in the second league (10.7%) (Table 4). No differences were found with regard to skin injuries, concussions, or tooth and internal injuries (Table 4). Players in the first league had a higher prevalence of shoulder and knee injuries but a lower prevalence of wrist and hand injuries than players in the second league (Table 5). No differences were found for other parts of the lower extremities, such as thighs, lower legs, ankles, and feet.
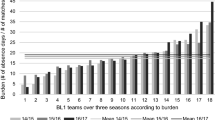
57.1% of all injures occurred during training sessions. The overall injury risk was 26 times higher in matches than in training sessions (Table 6). With 3.3 injuries per 1000 h per player in the second league, the average incidence rate per season was lower than that in the first league (4.9 per players, p < 0.01). The prevalence rate of the restructured second league had increased from 67.1 to 79.3% (p < 0.001) and the incidence rate from 3.7 to 4.1 per 1000 h (p < 0.0.1) from the first to the third seasons; hence almost to the same level of the first league (Table 7).
Taking the value of 1.0 of the first league as a reference for each season, the relative injury risk in the second league had increased from 0.86 (0.78–0.94) in the season 2010–2011 to 0.90 (0.82–0.98) in the season 2011–2012 and to 0.98 (0.91–1.05) in the season 2012–2013. The mean relative risk in the second league was 0.89 (0.83–0.94) in all three seasons. In the two seasons after the restructure, the overall injury risk in the two leagues had increased from 1.0 as a reference value in 2010–2011 to 1.11 (1.05–1.17) in 2011–2012 and to 1.12 (1.06–1.19) in 2012–2013.
Discussion
The most important finding of this study was that—after the restructure of the national second league—injury rates had almost increased to the level of the first national league.
This study presents for the first time detailed information on the injury risk and patterns of professional men’s team handball in the two highest national leagues. The results show significant differences in injury risk between the first and second team handball leagues. First league players had sustained more injuries: this difference may be explained by the increased physical intensity, the higher psychological intensity, and the larger number of players in the first league who also compete in international matches with their respective clubs and national teams.
After the restructure of the national second league, injury prevalence had increased from 67.1 to 79.3% (p < 0.001) and injury incidence from 3.7 to 4.1 per 1000 h (p < 0.01); hence almost to the level of the first league (Table 6, 7). In football, the implementation of a new professional league had increased the rate of ACL and PCL injuries but no data for team handball have been available so far [15]. In this study, the incidence of time-loss injuries, particularly ruptures, dislocations, and fractures was higher in the second league, although the training exposure was calculated to be the same in both leagues. This calculated incidence rate may be different; thus the difference between the two leagues may even be larger, if a higher training exposure had been calculated for first league players. This difference in time loss with a higher injury incidence rate of second league players may be due to the rapidly changing higher physical impact on the players [9, 15]. In addition, league matches in the second league were increased from 2 × 17 matches in the previous regional two league system to 2 × 19 matches after the restructure; thus, the travel burden was increased, subsequently decreasing the time and quality of regeneration.
Increased training and playing intensity as a possible risk factor for severe injuries, such as ACL tears, has been discussed in the literature [18, 26]. A study conducted during the World Men’s Handball Championship in 2015 had yielded a higher injury incidence rate of 104.5 per 1,000 h match exposure [6]. The rapid increase in physical impact during the professional tournaments also seems to directly influence injury rates, similar to the restructure of the team handball league. This increase could be one explanation for the overall higher incidence rates of time-loss injuries between the two leagues, particularly ruptures, dislocations, and fractures.
The increasing professionalism of the national second league after its restructure should therefore be matched by the availability of medical infrastructure that is equal to the medical service available to first league players. Injury prevention strategies for similar situations in professional team handball should be combined with already existing prevention programs to reduce time-loss injuries, such as ruptures, dislocations, and fractures as well as their long-term consequences. Prevention strategies should therefore focus on reducing the number of matches, monitoring and managing the training and match load, identify dangerous load peaks, decrease the travel burden, and increase regeneration.
The injury risk in the second league had also increased in the second season after the restructure, indicating a longer process to adapt to the specific demands of professional team handball. Psychological and mental influencing factors on contact and non-contact injuries are well known but were not considered in this study [2, 10].
The first league showed a higher incidence rate of acute shoulder and knee injuries but a lower prevalence of wrist and hand injuries than the second league (Table 6). Knees and shoulders may be more affected by the higher training and match load of first league teams, whereas wrist and hand injuries may be higher in the second league because of different (tactical) match plays. Players of the first league also showed 1.0% more overuse injuries than players of the second league (Table 5). This increase may be explained by the higher training and match load for some teams and players, i.e. German Cup matches, international matches, and matches with the national teams, which is a known risk factor for shoulder overuse injuries [19].
Injury severity differed between the two leagues. More medical attention injuries occurred in the first league than in the second league, whereas time-loss injuries of all severity levels were more common in the second league (Table 3). This difference may be explained by the higher rate of fractures, ruptures and dislocations occurring in the second league (Table 5). These types of injury require extensive medical intervention and result in more time loss than other types of injuries, such as contusions and sprains that occurred more often in the first league. In addition, a better medical infrastructure, greater availability of equipment, increased support in return-to-competition, and higher pressure to play may be reasons for first league players to continue playing or to return to competition more quickly.
In our study, the majority of injuries were acute injuries. Acute injuries with severe time-loss mainly affected the shoulders, hands, and the lower extremities, particularly the knees and ankles. A study by Giroto et al. showed an injury incidence rate of 3.7 per 1000 h training exposure and 20.3 per 1000 h match exposure for both men and women. Similar to our results, ankles (19.4%) and knees (13.5%) were the body regions most affected by traumatic injuries. The overall injury incidence and overall injury risk were comparable to that of previous studies on professional team handball [5, 6, 9, 17, 20, 22, 25]. However, most studies have focused on female players and tournament setting, such as the Olympic Games. Only a few studies have recently investigated the injuries in professional men’s team handball in a league setting [9, 25].
So far, injury prevention programs have focused on acute knee injuries, such as ACL tears, and these studies have shown good results in preventing non-contact injuries in females and adolescents [1, 21]. But studies should also be conducted in the important group of professional male players to confirm the previous promising results. Additionally, more studies should investigate injury-prone situations. For example, video analysis may help to identify injury-inciting events, and subsequently result in the appropriate adjustment of existing preventive approaches. The data of this study recommend investing in injury prevention of acute shoulder and hand injuries in addition to the established injury prevention programs for acute knee injuries. The only study available so far on shoulder injury prevention has focused on overuse injury [5].
This study has a number of methodological limitations. Its retrospective design necessitated calculation of training exposure from the personal experiences of the first and senior author. Because many lower-ranked teams in the second league only had a few training sessions per week, especially during the first investigated season before the restructure, the different levels of professionalism had decreased the weekly average. Training exposure was not calculated for different periods of the seasons because such calculation would have been on too many unknown variables.
Second league teams might have increased their training hours after the restructure of the national second league; therefore, the calculated injury incidence had not increased as much as calculated. Nonetheless, the prevalence in this subpopulation had risen after the restructure. Another limitation was that 2-min suspensions in matches were not accounted for in the approximated estimation of match exposure. In addition, foreign national team matches were not included, and pre-season and in-season friendly matches were calculated as training exposure if they had not been announced to the VBG.
The number of non-reported slight injuries with less than 3 day absence is unknown, and report rate of minimal and slight injuries probably differs among the team physicians. Another limitation is that no differentiation could be made between medical attention injuries and time-loss injuries of 0 days. Due to the registration methods, chronic injuries were likely to be underrepresented. Chronic injuries are typically not eligible for financial reimbursement by the VBG. Thus, team physicians may have less incentive to report chronic injuries than acute injuries. Career-ending injuries were not assessed and should be investigated in the future.
The strength of the study is the unique data sample of professional men’s team handball injuries, the size of the study population, and the length over three consecutive seasons. Moreover, the study includes data before and after the rare event of restructuring a professional team handball league. A further advantage is the high accuracy and validity of the data on injuries with more than 3 days time loss using the injury data from professional sports physicians in contrast to other studies using injury self-reports from team coaches and players.
This study is the largest study on professional men’s team handball so far. The aim was to provide objective data to all people involved in this sport, including medical personnel, coaches, officials, and athletes. Several recommendations can be made in support of a potentially safer environment, such as better equipment, a set of handball rules and regulations, and warm-up exercises [14]. Active prevention must be mandatory and may be addressed by reducing the training and match load combined with sufficient regeneration between matches. Teams who move up in a professional league should invest in qualified medical staff as well as in appropriate equipment and infrastructure to be able to professionally counteract the increasing injury incidence and prevalence. To prevent rapid changes in training intensity, teams who expect moving up into a higher league should slowly increase their training load to the level of the training volume expected in the following season.
Conclusion
In conclusion, professional team handball shows significant differences in injury incidence and prevalence between the first and second leagues. After the restructure of the national second league, injury rates had almost increased to the same level of the first league, probably due to the increase in match and training load as well as travel burden. Prevention strategies should therefore focus on reducing the number of matches, monitoring and managing the match and training load, identifying dangerous load peaks, decreasing the travel burden, and increasing the quality and time of regeneration for each individual player. Injury prevention is mandatory for players with high injury profiles, and professional prevention strategies should particularly focus on injuries of the shoulders, hands, and lower extremities.
References
Achenbach L, Krutsch V, Weber J, Nerlich M, Luig P, Loose O, Angele P, Krutsch W (2017) Neuromuscular exercises prevent severe knee injury in adolescent team handball players. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4758-5
Alentorn-Geli E, Myer GD, Silvers HJ, Samitier G, Romero D, Lazaro-Haro C, Cugat R (2009) Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: mechanism of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc 17(7):705–729
Åman M, Forssblad M, Henriksson-Larsén K (2014) Insurance claims data: a possible solution for a national sports injury surveillance system? An evaluation of data information against ASIDD and consensus statements on sports injury surveillance. BMJ Open 4(6):e005056
Åman M, Forssblad M, Larsén K (2017) Incidence and body location of reported acute sports injuries in seven sports using a national insurance database. Scand J Med Sci Sports. https://doi.org/10.1111/sms.12956
Andersson SH, Bahr R, Clarsen B, Myklebust G (2017) Preventing overuse shoulder injuries among throwing athletes: a cluster-randomised controlled trial in 660 elite handball players. Br J Sports Med 51(14):1073–1080
Bere T, Alonso J-M, Wangensteen A, Bakken A, Eirale C, Dijkstra HP, Ahmed H, Bahr R, Popovic N (2015) Injury and illness surveillance during the 24th Men’s Handball World Championship 2015 in Qatar. Br J Sports Med 49(17):1151–1156
Finch C (2014) How useful are insurance claim data for sports injury prevention purposes? BMJ Open 10(3):181–183
Fuller CW, Ekstrand J, Junge A, Andersen TE, Bahr R, Dvorak J, Hägglund M, McCrory P, Meeuwisse WH (2006) Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Clin J Sport Med 16(2):97–106
Giroto N, Hespanhol Junior LC, Gomes MR, Lopes AD (2017) Incidence and risk factors of injuries in Brazilian elite handball players: a prospective cohort study. Scand J Med Sci Sports 27(2):195–202
Hägglund M, Waldén M (2016) Risk factors for acute knee injury in female youth football. Knee Surg Sports Traumatol Arthrosc 24(3):737–746
Henke T, Schulz D, Wilke G (2005) Sportunfälle im Berufshandball. Ruhr-Universität Bochum, Bochum
Junge A, Langevoort G, Pipe A, Peytavin A, Wong F, Mountjoy M, Beltrami G, Terrell R, Holzgraefe M, Charles R, Dvorak J (2005) Injuries in Team Sport Tournaments during the 2004 Olympic Games. Am J Sports Med 34(4):565–576
Junge A, Engebretsen L, Mountjoy ML, Alonso JM, Renstrm PAFH., Aubry MJ, Dvorak J (2009) Sports injuries during the Summer Olympic Games 2008. Am J Sports Med 37(11):2165–2172
Klügl M, Shrier I, McBain K, Shultz R, Meeuwisse WH, Garza D, Matheson GO (2010) The prevention of sport injury: an analysis of 12.000 published manuscripts. Clin J Sports Med 20(6):407–412
Krutsch W, Zeman F, Zellner J, Pfeifer C, Nerlich M, Angele P (2016) Increase in ACL and PCL injuries after implementation of a new professional football league. Knee Surg Sports Traumatol Arthrosc 24(7):2271–2279
Langevoort G, Myklebust G, Dvorak J, Junge A (2007) Handball injuries during major international tournaments. Scand J Med Sci Sports 17(4):400–407
Laver L, Myklebust G (2014) Handball injuries: epidemiology and injury characterization. In: Doral MN, Karlsson J (eds) Sports injuries: prevention, diagnosis, treatment and rehabilitation. Springer, Berlin
Mihata LC, Beutler AI, Boden BP (2006) Comparing the incidence of anterior cruciate ligament injury in collegiate lacrosse, soccer, and basketball players. Implications for anterior cruciate ligament mechanism and prevention. Am J Sports Med 34(6):899–904
Moller M, Nielsen RO, Attermann J, Wedderkopp N, Lind M, Sorensen H, Myklebust G. Handball load and shoulder injury rate: a 31 week cohort study of 679 elite youth handball players. Br J Sports Med 51(4):231–237
Moller M, Attermann J, Myklebust G, Wedderkopp N (2012) Injury risk in Danish youth and senior elite handball using a new SM text message approach. Br J Sports Med 46(10):531–537
Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R (2003) Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med 13(2):71–78
Oehlert K, Drescher W, Petersen W, Zantop T, Gro V, Hassenpflug J (2004) Verletzungen im olympischen Handballturnier: eine Videoanalyse. Sportverletz Sportschaden 18:80–84
Otago L, Peake J (2007) The role of insurance data in setting priorities for netball injury prevention strategies. J Sci Med Sport 10(2):105–109
Pieper HG, Kohlhaas K, Zinser W, Reiners V, Jarmuth M (1998) Epidemiologie von Verletzungen in der 1. Handballbundesliga der Herren. Sport Orthopädie Sport Traumatolgie 14:58–62
Rafnsson ET, Valdimarsson Ö, Sveinsson T, Arnason A (2017) Injury pattern in Icelandic elite male handball players. Clin J Sport Med. https://doi.org/10.1097/JSM.0000000000000499
Roi GS, Nanni G, Tencone F (2006) Time to return to professional soccer matches after ACL reconstruction. Sport Sci Health 1(4):142–145
Seil R, Rupp S, Tempelhof S, Kohn D (1998) Sports injuries in team handball: a one-year prospective study of sixteen men’s senior teams of a superior nonprofessional level. Am J Sports Med 26(5):681–687
Acknowledgements
This study was conducted in coopertation with the insurancy company Verwaltungs-Berufsgenossenschaft who provided the dataset on professional handball players. Funding was received by the VBG in the framework of the project “Entwicklung und Evaluierung” (Development and evaluation). The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Luig, P., Krutsch, W., Nerlich, M. et al. Increased injury rates after the restructure of Germany’s national second league of team handball. Knee Surg Sports Traumatol Arthrosc 26, 1884–1891 (2018). https://doi.org/10.1007/s00167-018-4851-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4851-4