Abstract
Purpose
To assess and compare the clinical and MRI outcomes of patients with talus osteochondral defect (OCD) and patients without OCD in a cohort with chronic lateral ankle instability.
Methods
All patients who underwent open or arthroscopic anterior talofibular ligament repair of the lateral ligament complex by a single surgeon were included in this study. Ankle arthroscopic surgery was initially performed to manage any intra-articular OCD, including debridement and microfracture. Functional scores (AOFAS, Karlsson score) and Tegner activity level scores were determined. An MRI scan was performed at follow-up to assess talus OCD after treatment. Spearman’s correlation coefficients were calculated between functional scores and various factors.
Results
A total of 104 patients with chronic ankle instability were included in this study. Among them, 33 patients had cartilage injury on the talus (OCD group), and the other 71 patients had no cartilage injury (control group). After surgery, there was a significant increase in the AOFAS scores (p < 0.001), the Karlsson scores (p < 0.001), and the Tegner activity scores (p < 0.001) in both the OCD group and the control group. However, there was no significant difference in the AOFAS scores (90.7 ± 6.6 vs. 92.5 ± 8.5; n.s.), the Karlsson scores (89.7 ± 9.3 vs. 91.2 ± 9.1; n.s.), or the Tegner activity scores (5 vs. 6; n.s.) between the OCD group and the control group postoperatively. In the OCD group, there was a significant negative association between the functional scores (AOFAS, Karlsson score, or Tegner score) and the number of intra-articular lesions. For the lateral OCD, the mean lesion area significantly decreased from 49.0 ± 10.7 mm2 preoperatively to 18.3 ± 13.1 mm2 at the final follow-up (p < 0.001).
Conclusion
No significant difference in functional outcomes was found between the OCD group and the control group postoperatively. Arthroscopic microfracture is a good option for the long-term treatment of lateral talus OCD.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteochondral defect (OCD) or lesion of the talus can accompany chronic lateral ankle instability (CAI). Cartilage damage was noted in 17–66% of ankles with lateral ligament injuries [3, 12, 21, 26]. For patients with CAI accompanied by talus OCD, simultaneous surgery involving lateral ankle stabilization and cartilage treatment is indicated [10, 30].
Previously, Okuda et al. [22] reported that in patients with CAI, there were no significant differences in the clinical and radiological results of patients with OCD and those without OCD after lateral ligament surgery at a mean follow-up of 38 months. However, Hua et al. [13] treated 33 cases of talus OCD in 79 unstable ankles with debridement or microfracture, and they found that at 2-year follow-up, the patients without OCD had better AOFAS scores than patients with OCD. Thus, there is controversy over postoperative results in patients with chronic ankle instability and osteochondral lesion of the talus, particularly in the short term. Since cartilage tissue quality can be improved after microfracture [28], there is growing interest in whether there are any long-term differences between patients with OCD and patients without OCD.
Therefore, the purpose of this study was to assess and compare the clinical and MRI outcomes of patients with and without talus osteochondral defect (OCD) in a cohort with CAI and to analyse the related factors affecting the clinical and radiological outcomes after OCD treatment and lateral ankle stabilization.
Materials and methods
All patients who underwent anterior talofibular ligament (ATFL) repair of the lateral ligament by a single surgeon were included in this study. Patients were excluded if they had (1) obvious bony deformity of the ankle or foot on the affected side, (2) previous surgery of the affected limb, (3) neuromuscular disorders, (4) generalized hypermobility (apposition of the thumb to the forearm), or (5) medial ankle instability (a feeling of giving way, pain on the medial gutter of the ankle, and a valgus and pronation deformity of the foot).
Surgical technique
The patient was placed in a supine position on an operating table under general anaesthesia. The patient underwent an arthroscopic evaluation of the ankle joint before lateral ligament repair, and intra-articular pathologies were also addressed. The intra-articular lesions (including talus osteochondral defect, syndesmosis injury, synovitis, and anterior impingement syndrome by osteophyte) were evaluated and recorded under the arthroscopy, and debridement was performed if necessary.
After the talus OCD was identified, the treatment was determined by the stage and size of the lesion [9]. For cartilage with a rough surface or fibrillation, only debridement was performed. For lesions with a visible cartilage defect smaller than 15 mm in diameter, microfracture was performed. Osteochondral autograft is recommended as the initial treatment for only patients with a lesion that has a diameter larger than 15 mm.
Next, the lateral ankle ligaments were evaluated and treated. A curvilinear incision was made over the lateral malleoli. The remnant of the anterior talofibular ligament (ATFL) or the calcaneofibular ligament (CFL) was identified and exposed. One or two suture anchors were inserted into the fibula (2.9-mm lupine [DePuy Mitek, Raynham, MA]). The ATFL or the CFL was tensioned with the ankle slightly everted and fixed to the fibula. The proximal extensor retinaculum was drawn and sutured to the distal fibula to reinforce the repair of the ATFL and the CFL.
After surgery, the ankle was immobilized in a neutral position using a short leg cast. Two weeks after the surgery, the cast was changed to an ankle brace (A60, DJO Global, Inc., USA), and passive range of motion was initiated. Weight-bearing was permitted after 4 weeks.
Clinical evaluation
A clinical examination, including subjective functional examinations and physical examinations, was performed by an experienced orthopaedic surgeon. Subjective functional examinations included the American Orthopaedic Foot and Ankle Society (AOFAS), the Karlsson ankle functional score (Karlsson score), and the Tegner activity score. In addition, the physical examination included the anterior drawer test (ADT). The ADT was carried out with the lower leg hanging free with the knee flexed. The ankle was in 10° to 20° of plantar flexion, and the tibia was stabilized with one hand and the heel grasped by the other hand. The ADT was clinically evaluated bilaterally: A <5-mm side-to-side difference in tibiotalar translation was considered normal (grade 0), a 5- to 10-mm side-to-side difference was classified as grade 1, a 10- to 15-mm difference was classified as grade 2, and a >15-mm difference was classified as grade 3.
MRI scan and image analysis
Imaging was performed with the patient in a relaxed neutral position using a 3.0-T magnetic resonance imaging (MRI) scanner (MAGNETOM Verio, A Tim system, Siemens, Germany). All participants had at least 1 h of rest before the MRI scan was performed. Coronal and sagittal images were obtained with short time inversion recovery (STIR): repetition time, 5730 ms; echo time, 34 ms; flip angle, 150°; matrix, 256 × 230; field of view, 15 × 15 cm; slice thickness, 3 mm; and scan time, 2 min, 2 s. The OCD area was calculated using the following equation: OCD area = coronal length × sagittal length × 0.79 [6]. The MRI assessment was performed by a different surgeon than the one that performed the clinical evaluation.
The study was approved by the Health Sciences Institutional Review Board of Huashan Hospital Fudan University (2016-002), and written consent was obtained from all participants.
Statistical analysis
The data analysis was performed using Stata 10.0 software (Stata Corp, USA), and the data are reported as the means and standard deviations. First, a post hoc power analysis was performed. If a difference of at least 10 was detected in the functional score (AOFAS or Karlsson score) between groups, it was considered a clinically significant difference in the functional scores. Given the standard deviation (SD) of the functional score (AOFAS or Karlsson score) in the data, the sample sizes of the OCD group (n = 33) and the control group (n = 71) had a power of 80% when the level of significance was set at 0.05. To quantify the proportion of the variance from the OCD area measurements, the intra-class correlation coefficient (ICC) was assessed by examining intra-observer reliabilities. The ICC was interpreted as poor if ICC < 0.4, marginal if 0.4 ≤ ICC ≤ 0.75, and good if ICC > 0.75. A χ 2 test was used to compare the categorical variables. A two-sample t test or a two-sample Wilcoxon rank-sum test was used to compare the continuous variables between groups. Spearman’s correlation coefficients were calculated between the functional scores (AOFAS, Karlsson score, or Tegner score) and various factors (gender, age, BMI, injury time, follow-up time, and number of intra-articular lesions). The significance level was set at 0.05.
Results
A total of 104 patients with chronic ankle instability were included in this study. Among them, 33 patients had cartilage injury on the talus (OCD group), and the other 71 patients had no cartilage injury (control group). In the OCD group, 19 patients (58%) had lateral lesions, and 14 (42%) had medial lesions. In the OCD group, there were eight patients with synovitis, one patient with syndesmosis injury, and ten patients with anterior impingement syndrome by osteophyte. There was no significant difference in age, BMI, injury time, or follow-up time between the OCD group and the control group (Table 1).
On physical examination, no patient in either group had ankle instability, and the ADTs of all ankles were normal (grade 0). No patients complained of ankle instability at the time of follow-up. Postoperatively, there was no significant difference in the AOFAS, the Karlsson score, or the Tegner activity score between the OCD group and the control group (Table 2).
In the OCD group, 15 patients were treated with debridement treatment (Debridement subgroup), 17 patients underwent microfracture treatment (Microfracture subgroup), and 1 patient had osteochondral autograft implantation. The Debridement subgroup appeared to have better functional scores compared to those of the Microfracture subgroup, but none of these differences were significant (AOFAS: 93.6 ± 5.7 vs. 91.7 ± 10.6, n.s.; Karlsson score: 93.3 ± 4.5 vs. 89.5 ± 11.8, n.s.; and Tegner activity score: 6 vs. 5, n.s.).
For the OCD group, there was no significant association between the functional scores (AOFAS, Karlsson score, or Tegner score) and gender, age, BMI, injury time, and follow-up time (Table 3). Interestingly, there was a significant negative association between the functional scores (AOFAS, Karlsson score, or Tegner score) and the number of intra-articular lesions (p = 0.03, p = 0.001, and p = 0.001, respectively).
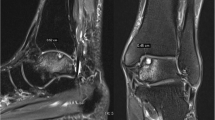
The ICC index of intra-observer reliability was 0.76 for the OCD area value. For the Microfracture subgroup, the OCD lesion area was calculated and compared with preoperative and postoperative MRI images (Fig. 1). For the lateral OCD, the mean lesion area significantly decreased from 49.0 ± 10.7 mm2 preoperatively to 18.3 ± 13.1 mm2 at the final follow-up (p < 0.001; Fig. 2). For the medial OCD, there was no significant difference after surgery (n.s.; Fig. 3).
MRI images of a patient with lateral OCD preoperatively, at 2 years postoperative, and at 4 years postoperatively. The MRI images with three consecutive slices (S1, S2, and S3) revealed that the cartilage lesion area significantly decreased after surgery and that the cartilage quality improved with time. OCD osteochondral defect, CAI chronic ankle instability
Discussion
The most important finding of this study was that no significant differences in functional outcomes were found postoperatively between the OCD group and the control group. Arthroscopic microfracture treatment provides a limited effect for medial talus OCD. Prolonged lateral ankle instability can lead to a cartilage defect of the ankle [26]. If conservative treatment fails, surgery is indicated to not only repair the ATFL, but also treat the accompanying intra-articular problems, such as talus OCD, syndesmosis injury, synovitis, and anterior impingement syndrome by osteophyte [13, 16, 21]. Particularly, an OCD can be a source of pain and clinical failure if it is not addressed [15, 23].
In the present study, the OCD group had a good clinical outcome postoperatively, with no significant difference in AOFAS, Karlsson score, or Tegner activity score compared to the control group. In fact, most of the OCDs were small lesions accepting debridement or microfracture in this study. Previously, Nery et al. [18] reviewed 38 patients who had arthroscopic Broström-Gould repair for the management of lateral ankle instability, and no significantly different outcomes were observed between patients with OCD (microfracture management) and patients without cartilage lesions at a mean follow-up of 9.8 years. It was presumed that the lesion diameter and the site of the OCD in each study may have been different.
In the present study, no significant association was found between the functional scores (AOFAS, Karlsson score, or Tegner score) and gender, age, BMI, injury time, and follow-up time. It has been reported that increasing age, higher body mass index, history of trauma, cartilage degeneration, and osteophyte presence negatively affect outcomes [7, 27]. Becher et al. [1] reported that a BMI of greater than 25 kg/m2 appeared to be a negative prognostic factor. Previously, Van Bergen et al. [29] found that none of the prognostic factors (size, location, and classification of the defect; patient age and body mass index; traumatic aetiology; and symptom duration) was significantly associated with decreased ankle function after arthroscopic debridement and bone marrow stimulation for talar OCD. Interestingly, there was a significant negative association between the functional scores (AOFAS, Karlsson score, or Tegner score) and the number of intra-articular lesions. Previously, Choi et al. [5] found that syndesmosis widening, talus osteochondral lesions, and ossicles are significant predictors of unsatisfactory results after ligament reconstruction. The presence of any combination of associated intra-articular lesions can result in a poor outcome.
Generally, the treatment options for talus OCD include debridement, microfracture, arthroscopic drilling, osteochondral autografts or allografts, and autologous chondrocyte transplantation for symptomatic patients [10, 17, 19, 20, 24, 27]. Arthroscopic microfracture treatment is an effective and reliable technique for treating small- to mid-sized osteochondral lesions of the talus [4, 6, 8, 11, 14]. Previously, Chuckpaiwong et al. [7] demonstrated that excellent results were obtained after microfracture for an OCD smaller than 15 mm in diameter, regardless of the defect location. In the present study, however, it was found that the mean lesion area significantly decreased after surgery for lateral OCDs, whereas there was no significant difference for medial OCDs after microfracture surgery. In a long-term investigation of microfracture in the treatment of OCD, it was observed that lateral lesions had significantly better functional results [24]. Previously, it was reported that the position of the peak strain on the injured ankle also showed significant anterior translation and medial translation after ankle sprain (Fig. 4a) [2]. Medial translation of the pressure centre was still elevated after the ATFL repair compared with the intact condition (Fig. 4b) [25]. Altered ankle kinematics may contribute to the medial side of the tibiotalar joint degeneration that occurs with chronic lateral ankle instability. Thus, it was concluded that microfracture may not be appropriate for medial OCDs in the unstable ankles. This study provides valuable quantitative information comparing the effects and outcomes for ankles with and without OCD in patients with lateral ankle instability. It was demonstrated that functional scores had a significant negative association with the number of intra-articular lesions, and the arthroscopic microfracture is a good option for the treatment of lateral talus OCD in unstable ankles over the long term.
Schematic diagram illustrating the altered ankle kinematics after lateral collateral ligament injury and repair. a The position of the peak strain (red circle) on the injured ankle translated anteriorly and medially compared with the contralateral intact ankle. b Medial translation of the pressure centre (red circle) was still elevated after the ankle lateral ligament repair compared to that of the contralateral intact ankle
This study had several limitations. First, this was a retrospective study. A prospective study would provide more accurate information regarding the true improvement that patients experience with OCD treatment. Another limitation is the small sample sizes of the Debridement subgroup and the Microfracture subgroup. Additional studies with larger sample sizes may be necessary to determine differences in clinical outcomes between the Debridement subgroup and the Microfracture subgroup. This study documents midterm outcomes, and more research is necessary to determine long-term outcomes in this patient population.
Conclusion
No significant differences were found in functional outcomes between the OCD group and the control group postoperatively after the ATFL repair procedure. Arthroscopic microfracture treatment is a good long-term option for talus OCD in select patients. Microfracture has a limited positive effect for medial OCDs in unstable ankles, even after reconstruction.
References
Becher C, Driessen A, Hess T, Longo UG, Maffulli N, Thermann H (2010) Microfracture for chondral defects of the talus: maintenance of early results at midterm follow-up. Knee Surg Sports Traumatol Arthrosc 18:656–663
Bischof JE, Spritzer CE, Caputo AM, Easley ME, DeOrio JK, Nunley JA 2nd, DeFrate LE (2010) In vivo cartilage contact strains in patients with lateral ankle instability. J Biomech 43:2561–2566
Cha SD, Kim HS, Chung ST, Yoo JH, Park JH, Kim JH, Hyung JW (2012) Intra-articular lesions in chronic lateral ankle instability: comparison of arthroscopy with magnetic resonance imaging findings. Clin Orthop Surg 4:293–299
Choi JI, Lee KB (2016) Comparison of clinical outcomes between arthroscopic subchondral drilling and microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc 24:2140–2147
Choi WJ, Lee JW, Han SH, Kim BS, Lee SK (2008) Chronic lateral ankle instability: the effect of intra-articular lesions on clinical outcome. Am J Sports Med 36:2167–2172
Choi WJ, Park KK, Kim BS, Lee JW (2009) Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med 37:1974–1980
Chuckpaiwong B, Berkson EM, Theodore GH (2008) Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy 24:106–112
Donnenwerth MP, Roukis TS (2012) Outcome of arthroscopic debridement and microfracture as the primary treatment for osteochondral lesions of the talar dome. Arthroscopy 28:1902–1907
Ferkel RD, Zanotti RM, Komenda GA, Sgaglione NA, Cheng MS, Applegate GR, Dopirak RM (2008) Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med 36:1750–1762
Georgiannos D, Bisbinas I, Badekas A (2016) Osteochondral transplantation of autologous graft for the treatment of osteochondral lesions of talus: 5- to 7-year follow-up. Knee Surg Sports Traumatol Arthrosc 24:3722–3729
Hannon CP, Smyth NA, Murawski CD, Savage-Elliott I, Deyer TW, Calder JD, Kennedy JG (2014) Osteochondral lesions of the talus: aspects of current management. Bone Joint J 96-B:164–171
Hintermann B, Boss A, Schafer D (2002) Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med 30:402–409
Hua Y, Chen S, Li Y, Chen J, Li H (2010) Combination of modified Brostrom procedure with ankle arthroscopy for chronic ankle instability accompanied by intra-articular symptoms. Arthroscopy 26:524–528
Lee KB, Bai LB, Chung JY, Seon JK (2010) Arthroscopic microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc 18:247–253
Lee M, Kwon JW, Choi WJ, Lee JW (2015) Comparison of outcomes for osteochondral lesions of the talus with and without chronic lateral ankle instability. Foot Ankle Int 36:1050–1057
Maffulli N, Del Buono A, Maffulli GD, Oliva F, Testa V, Capasso G, Denaro V (2013) Isolated anterior talofibular ligament Brostrom repair for chronic lateral ankle instability: 9-year follow-up. Am J Sports Med 41:858–864
Murawski CD, Kennedy JG (2013) Operative treatment of osteochondral lesions of the talus. J Bone Joint Surg Am 95:1045–1054
Nery C, Raduan F, Del Buono A, Asaumi ID, Cohen M, Maffulli N (2011) Arthroscopic-assisted Brostrom-Gould for chronic ankle instability: a long-term follow-up. Am J Sports Med 39:2381–2388
Niemeyer P, Salzmann G, Schmal H, Mayr H, Sudkamp NP (2012) Autologous chondrocyte implantation for the treatment of chondral and osteochondral defects of the talus: a meta-analysis of available evidence. Knee Surg Sports Traumatol Arthrosc 20:1696–1703
O’Loughlin PF, Heyworth BE, Kennedy JG (2010) Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med 38:392–404
Odak S, Ahluwalia R, Shivarathre DG, Mahmood A, Blucher N, Hennessy M, Platt S (2015) Arthroscopic evaluation of impingement and osteochondral lesions in chronic lateral ankle instability. Foot Ankle Int 36:1045–1049
Okuda R, Kinoshita M, Morikawa J, Yasuda T, Abe M (2005) Arthroscopic findings in chronic lateral ankle instability: do focal chondral lesions influence the results of ligament reconstruction? Am J Sports Med 33:35–42
Park KH, Lee JW, Suh JW, Shin MH, Choi WJ (2016) Generalized ligamentous laxity is an independent predictor of poor outcomes after the modified brostrom procedure for chronic lateral ankle instability. Am J Sports Med 44:2975–2983
Polat G, Ersen A, Erdil ME, Kizilkurt T, Kilicoglu O, Asik M (2016) Long-term results of microfracture in the treatment of talus osteochondral lesions. Knee Surg Sports Traumatol Arthrosc 24:1299–1303
Prisk VR, Imhauser CW, O’Loughlin PF, Kennedy JG (2010) Lateral ligament repair and reconstruction restore neither contact mechanics of the ankle joint nor motion patterns of the hindfoot. J Bone Joint Surg Am 92:2375–2386
Sugimoto K, Takakura Y, Okahashi K, Samoto N, Kawate K, Iwai M (2009) Chondral injuries of the ankle with recurrent lateral instability: an arthroscopic study. J Bone Joint Surg Am 91:99–106
Takao M, Komatsu F, Naito K, Uchio Y, Ochi M (2006) Reconstruction of lateral ligament with arthroscopic drilling for treatment of early-stage osteoarthritis in unstable ankles. Arthroscopy 22:1119–1125
Tao H, Shang X, Lu R, Li H, Hua Y, Feng X, Chen S (2014) Quantitative magnetic resonance imaging (MRI) evaluation of cartilage repair after microfracture (MF) treatment for adult unstable osteochondritis dissecans (OCD) in the ankle: correlations with clinical outcome. Eur Radiol 24:1758–1767
van Bergen CJ, Kox LS, Maas M, Sierevelt IN, Kerkhoffs GM, van Dijk CN (2013) Arthroscopic treatment of osteochondral defects of the talus: outcomes at eight to twenty years of follow-up. J Bone Joint Surg Am 95:519–525
Yasui Y, Takao M, Miyamoto W, Matsushita T (2014) Simultaneous surgery for chronic lateral ankle instability accompanied by only subchondral bone lesion of talus. Arch Orthop Trauma Surg 134:821–827
Acknowledgement
This work was supported by National Natural Science Foundation of China (81401812, 81271958, 81572108, 81572209, 81370052).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Funding
This study was funded by National Natural Science Foundation of China (No 81401812) and National Natural Science Foundation of China (No 81572209).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Li, H., Hua, Y., Li, H. et al. Treatment of talus osteochondral defects in chronic lateral unstable ankles: small-sized lateral chondral lesions had good clinical outcomes. Knee Surg Sports Traumatol Arthrosc 26, 2116–2122 (2018). https://doi.org/10.1007/s00167-017-4591-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4591-x