Abstract
Purpose
Quantitative guidelines for radiographic identification of the anterior and posterior ligaments of the proximal tibiofibular joint have not been well defined. The purpose of this study was to provide reproducible, quantitative descriptions of radiographic landmarks identifying the anterior and posterior ligament complexes of the proximal tibiofibular joint. It was hypothesized that consistent quantitative data regarding the radiographic location of the anterior and posterior proximal tibiofibular joint ligament complexes could be identified.
Methods
The footprint centers of the individual ligament bundles of the anterior and posterior complexes of the proximal tibiofibular joint were labeled with radio-opaque markers in ten non-paired, fresh-frozen cadaveric knee specimens. Anteroposterior (AP) and lateral radiographs of the proximal tibiofibular joint were obtained, and distances between the markers and pertinent radiographic landmarks were recorded.
Results
On AP radiographs, the tibial span of the anterior complex was 12.8 ± 3.9 mm and started at a median of 11.4 mm distal to the tibial plateau; the fibular span was 11.6 ± 6.8 mm and started at a median of 5.1 mm from the apex of the fibular styloid. The tibial span of the posterior complex was 11.7 ± 8.4 mm and began at a median of 12.1 mm distal to the tibial plateau; the fibular span was 11.8 ± 7.9 mm and began at a median of 3.1 mm distal to the apex of the fibular styloid. Values were similar for lateral radiographs.
Conclusion
The attachment locations of the proximal tibiofibular anterior and posterior complexes could be quantitatively correlated to reliable osseous landmarks and radiographic lines. This information will allow for consistent radiographic assessments of proper tunnel placement intraoperatively and postoperatively during anatomic reconstructions of the proximal tibiofibular joint.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radiographic identification of the anatomic attachment sites of knee ligament structures allows surgeons to obtain an accurate diagnosis and treatment of knee injuries. The previous studies have provided quantitative and radiographic data for other ligaments [1–6], which has aided surgeons in intraoperative tunnel placement [7, 8] and postoperative assessment of anatomic knee ligament reconstructions [7–10]. The qualitative and quantitative anatomic descriptions of the anterior and posterior ligament complexes of the PTFJ are currently becoming better understood due to recent focus on this topic [11, 12]. However, quantitative guidelines for radiographic identification of the anterior and posterior ligament bundles of the PTFJ are still lacking in the current literature.
Due to the complex anatomy of the posterolateral corner of the knee [13, 14], proper identification of tunnel placement is critical to properly diagnose and treat associated injuries to this area. Therefore, the purpose of this study was to provide reproducible, quantitative descriptions of radiographic landmarks identifying the anterior and posterior ligament complexes of the proximal tibiofibular joint to guide intraoperative tunnel placement and postoperative assessment of an anatomic proximal tibiofibular joint reconstruction.
Materials and methods
Specimen preparation
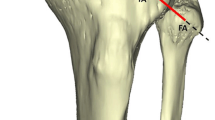
Ten non-paired (n = 10), fresh-frozen human cadaveric knees [median age 57 years (range 47–66 years); 8 male, 2 female] with no history of prior injury, anatomic abnormalities, ligament instability, osteoarthritis, or disease were utilized for the study. The cadaveric specimens utilized in this study were donated to a tissue bank for medical research and then purchased by our institution. Specimens were stored at −20 °C and thawed for 24 h prior to dissection. The femur was disarticulated and all soft tissues (except for the interosseous membrane) were removed distal to the tibiofemoral joint line. Screws were placed through the distal ends of the tibia and fibula of each specimen, with the interosseous membrane intact to ensure native anatomic positioning was obtained, and then potted in polymethyl methacrylate (PMMA) (Fricke Dental, Streamwood, Illinois). The individual bundles of both the anterior and posterior ligament complexes were carefully isolated. The anterior complex was always analyzed before the posterior complex. The tibial side was always analyzed before the fibular side, starting with the most superior bundle on the tibial side, followed by the next bundle inferiorly until the entire ligament complex was analyzed. As each bundle was sectioned from its tibial attachment, a radiopaque marker was placed in the center of its footprint, flush against the bone. This process was repeated on the fibular side.
Data collection
Using a mobile C-arm, standardized, anteroposterior (AP), and lateral radiographs were obtained separately for both the anterior (Fig. 1) and posterior (Fig. 2) ligament complexes of each specimen. The femur of the specimens utilized in this study had been disarticulated, and therefore, the femoral condyles were not available for reference during radiographs. To obtain an AP radiograph, the anterior and posterior margins of the medial tibial plateau were superimposed. To obtain a straight lateral radiograph, both medial and lateral plateaus were overlapped, the tibial tubercle was visualized, and a portion of the proximal head of the fibula (about 1/3 of the fibular head) was superimposed over the tibia, so that an outline of the fibular shaft could be seen posterior to the tibia. A 25.4-mm metal sphere scaling marker was placed at the same height and depth as the proximal tibiofibular joint for each radiograph and used later for magnification/measurement calibration with the PACS OrthoCase Imaging software (Merge Healthcare, Chicago, IL). Measurements obtained with the imaging software were reported to the nearest 0.1 mm.
For both AP and lateral radiographs, the proximodistal position of the center of each ligament bundle of the PTFJ was measured from the tibial plateau for tibial insertions, and from the apex of the fibular head for the fibular insertions. This was done by drawing a straight reference line along the entire tibial plateau for AP views and along the medial tibial plateau for lateral views. A line parallel to the previous reference line was then drawn at the apex of the fibular head for both AP and lateral views. Perpendicular line measurements were made from each respective parallel reference line to obtain the proximodistal distance to each ligament’s tibial and fibular attachment site (Figs. 3, 4). The width of the tibial plateau was measured on AP views as a reference for the size of each specimen and to determine if a correlation existed between the size of the specimen and the location of the ligaments. Two observers, both fellowship-trained orthopaedic surgeons (JC & GM), performed an independent round of measurements on each specimen to obtain inter-class measurement reliability. Institutional review board approval was not required, because the use of cadaveric specimens is exempt at Steadman Philippon Research Institute.
a Anteroposterior and b lateral schematic images of a left knee demonstrating the radiographic measurements of the posterior complex of the proximal tibiofibular joint. The tibial plateau surface line and the apex of the fibula were identified as a reference for the tibial and fibular ligaments, respectively. The blue markings represent the center of ligament attachments on the tibia and the red markings represent the center of ligament attachments on the fibular head
a Anterior and b posterior ligamentous complex of the proximal tibiofibular joint. ALL anterolateral ligament, G Gerdy’s tubercle, TT tibial tubercle, FCL fibular collateral ligament, PCL posterior cruciate ligament. After identification of the individual bundles, radiopaque marker was placed in the center of its footprint, flush against the bone, to be identified for subsequent measurements
Statistical analysis
Summary statistics were used to characterize radiographically measured anatomic distances. Spearman correlations were calculated to test for association between measurements. Interrater measurement reliability was assessed using the random-effects, single measures, absolute agreement definition of the intra-class correlation coefficient (ICC), reported with non-parametric 95% bootstrap confidence intervals. All analyses and figures were produced using the statistical programming language R [15]. Note that ligament span was defined by calculating the difference between the most proximal and most distal ligament bundle of each respective complex and then averaged across all ten specimens.
Results
Interrater agreement across all specimens, for both AP and lateral views, and for both the fibular and tibial sides was excellent. The lowest agreement was for lateral view of fibular measurements [ICC = 0.993; 95% CI (0.977, 0.997)]. Detailed radiographic measurements for the individual separately identified bundles of the anterior and posterior ligament bundles of the proximal tibiofibular joint can be seen in Tables 1 and 2, respectively.
Anterior complex
The anterior complex spanned a proximodistal distance of 12.8 ± 3.9 mm on the tibia for AP radiographs and 13.7 ± 3.2 mm for lateral radiographs. The anterior complex spanned a proximodistal distance of 11.6 ± 6.8 mm on the fibula for AP radiographs and 14.6 ± 7.1 mm for lateral radiographs.
Posterior complex
The posterior complex spanned a proximodistal distance of 11.7 ± 8.4 mm on the tibia for AP radiographs and 12.9 ± 9.1 mm for lateral radiographs. The posterior complex spanned a proximodistal distance of 11.8 ± 7.9 mm on the fibula for AP radiographs and 10.9 ± 7.5 mm for lateral radiographs.
Tibial plateau width
The average width of the tibial plateau across all ten specimens was 73.7 ± 5.3 mm. There was no significant correlation between the tibial plateau width and span of the anterior or posterior ligament complexes on the tibia or fibula for either AP or lateral views (n.s.).
Discussion
The most important finding of this study was that quantitative radiographic assessment of the anatomic attachment sites of the anterior and posterior complexes of the proximal tibiofibular joint on standard radiographs could be consistently performed. Due to the thin nature of each individual bundle of the anterior and posterior ligaments and aiming towards a more clinically relevant measure, the span of the anterior and posterior complex was also assessed. This will aid surgeons in choosing tunnel placement for an anatomic reconstruction and provides guidelines to check this tunnel positioning intraoperatively with fluoroscopy.
Dislocation of the proximal tibiofibular joint (PTFJ) is a complex injury that often results in disruption of the posterior ligament complex [16–20]. Conservative treatment with closed reduction and immobilization is often recommended [18, 19, 21]; however, in cases of persistent joint instability following conservative management, surgical treatment is indicated [18, 19, 21–24]. Different surgical techniques have been proposed which include PTFJ arthrodesis [25, 26], fibular head resection [27, 28], re-routing of the biceps femoris tendon [29–31], closed-wedge high tibial osteotomy [32], and PTFJ ligament reconstruction [24, 33, 34]. Non-anatomic surgical treatments such as arthrodesis and fibular head resection are associated with complications such as chronic knee instability and chronic ankle pain [18, 21, 26, 27]; hence, anatomic reconstructions have been advocated [24, 33, 35–38]. Due to the reported improved biomechanical function and patient outcomes following anatomic reconstruction of torn knee ligaments [36, 38–40], acute traumatic or chronic PTFJ instability should be treated similarly [24].
The body of literature describing the anatomy of the proximal tibiofibular joint ligaments is scant, and to the authors’ knowledge, no radiographic assessment of the PTFJ ligaments has previously been performed. Furthermore, there is still no consensus in the literature on the number of bundles in both the anterior and the posterior complexes; however, due to the relatively small size of the individual bundles, treating the complex as a whole would seem most clinically relevant. The current study provides quantitative radiographic data for both the individual ligament bundles and the entire span of the anterior and posterior complexes. Intraoperative use of radiographs can guide surgeons in placing anatomic-based reconstruction graft tunnels, especially in injuries where the tissue cannot be easily identified.
It is acknowledged that there are some limitations to the present study. First, the relatively small number of specimens (n = 10) may underestimate the true anatomical variability of the PTFJ. In addition, the specimens were from donors who were older than the usual age range of patients who undergo a proximal tibiofibular reconstruction (however, the soft-tissue attachment sites and osseous landmarks of interest do not vary with age and the specimens had no evidence of the previous injury or large osteophyte formation).
Conclusion
The attachment locations of the proximal tibiofibular anterior and posterior complexes could be quantitatively correlated to reliable osseous landmarks and radiographic lines. This information will allow for consistent radiographic assessments of proper tunnel placement both intraoperatively and postoperatively during anatomic reconstructions of the proximal tibiofibular joint.
References
James EW, LaPrade CM, Ellman MB, Wijdicks CA, Engebretsen L, LaPrade RF (2014) Radiographic identification of the anterior and posterior root attachments of the medial and lateral menisci. Am J Sports Med 42(11):2707–2714
Kennedy MI, Claes S, Fuso FA, Williams BT, Goldsmith MT, Turnbull TL et al (2015) The anterolateral ligament: an anatomic, radiographic, and biomechanical analysis. Am J Sports Med 43(7):1606–1615
Pietrini SD, LaPrade RF, Griffith CJ, Wijdicks CA, Ziegler CG (2009) Radiographic identification of the primary posterolateral knee structures. Am J Sports Med 37(3):542–551
Pietrini SD, Ziegler CG, Anderson CJ, Wijdicks CA, Westerhaus BD, Johansen S et al (2011) Radiographic landmarks for tunnel positioning in double-bundle ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 19(5):792–800
Wijdicks CA, Griffith CJ, LaPrade RF, Johansen S, Sunderland A, Arendt EA et al (2009) Radiographic identification of the primary medial knee structures. J Bone Jt Surg Am 91(3):521–529
Williams BT, James EW, Jisa KA, Haytmanek CT, LaPrade RF, Clanton TO (2016) Radiographic identification of the primary structures of the ankle syndesmosis. Knee Surg Sports Traumatol Arthrosc 24(4):1187–1199
Galloway MT, Grood ES, Mehalik JN, Levy M, Saddler SC, Noyes FR (1996) Posterior cruciate ligament reconstruction. An in vitro study of femoral and tibial graft placement. Am J Sports Med 24(4):437–445
Noyes FR, Barber-Westin SD (2005) Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations. Am J Sports Med 33(5):646–654
Lee MC, Seong SC, Lee S, Chang CB, Park YK, Jo H, Kim CH (2007) Vertical femoral tunnel placement results in rotational knee laxity after anterior cruciate ligament reconstruction. Arthroscopy 23(7):771–778
Moisala AS, Jarvela T, Harilainen A, Sandelin J, Kannus P, Jarvinen M (2007) The effect of graft placement on the clinical outcome of the anterior cruciate ligament reconstruction: a prospective study. Knee Surg Sports Traumatol Arthrosc 15(7):879–887
Sarma A, Borgohain B, Saikia B (2015) Proximal tibiofibular joint: rendezvous with a forgotten articulation. Indian J Orthop 49(5):489–495
See A, Bear RR, Owens BD (2013) Anatomic mapping for surgical reconstruction of the proximal tibiofibular ligaments. Orthopedics 36(1):e58–e63
Brinkman JM, Schwering PJ, Blankevoort L, Kooloos JG, Luites J, Wymenga AB (2005) The insertion geometry of the posterolateral corner of the knee. J Bone Jt Surg Br 87(10):1364–1368
Cooper JM, McAndrews PT, LaPrade RF (2006) Posterolateral corner injuries of the knee: anatomy, diagnosis, and treatment. Sports Med Arthrosc 14(4):213–220
R: A language and environment for statistical computing (2016) R Foundation for Statistical Computing [computer program]. Vienna, Austria
Horan J, Quin G (2006) Proximal tibiofibular dislocation. Emerg Med J 23(5):e33
Ogden JA (1972) Dislocation of the proximal fibula. Radiology 105(3):547–549
Ogden JA (1974) Subluxation and dislocation of the proximal tibiofibular joint. J Bone Jt Surg Am 56(1):145–154
Sekiya JK, Kuhn JE (2003) Instability of the proximal tibiofibular joint. J Am Acad Orthop Surg 11(2):120–128
Semonian RH, Denlinger PM, Duggan RJ (1995) Proximal tibiofibular subluxation relationship to lateral knee pain: a review of proximal tibiofibular joint pathologies. J Orthop Sports Phys Ther 21(5):248–257
Ogden JA. (1974) The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res 101:186–191
Jabara M, Bradley J, Merrick M (2014) Is stability of the proximal tibiofibular joint important in the multiligament-injured knee? Clin Orthop Relat Res 472(9):2691–2697
Van Seymortier P, Ryckaert A, Verdonk P, Almqvist KF, Verdonk R (2008) Traumatic proximal tibiofibular dislocation. Am J Sports Med 36(4):793–798
Warner BT, Moulton SG, Cram TR, LaPrade RF. (2016) Anatomic Reconstruction of the Proximal Tibiofibular Joint. Arthrosc Tech 5(1):e207–210
Delos D, Schneidkraut J, Rodeo S. (2013) Successful fusion of the proximal tibiofibular joint with osteogenic protein-1 (OP-1) augmentation. HSS J 9(1):90–95
Halbrecht JL, Jackson DW (1991) Recurrent dislocation of the proximal tibiofibular joint. Orthop Rev 20(11):957–960
Draganich LF, Nicholas RW, Shuster JK, Sathy MR, Chang AF, Simon MA (1991) The effects of resection of the proximal part of the fibula on stability of the knee and on gait. J Bone Jt Surg Am 73(4):575–583
Molitor PJ, Dandy DJ (1989) Permanent anterior dislocation of the proximal tibiofibular joint. J Bone Jt Surg Br 71(2):240–241
Mena H, Brautigan B, Johnson DL (2001) Split biceps femoris tendon reconstruction for proximal tibiofibular joint instability. Arthroscopy 17(6):668–671
Miettinen H, Kettunen J, Vaatainen U (1999) Dislocation of the proximal tibiofibular joint. A new method for fixation. Arch Orthop Trauma Surg 119(5–6):358–359
Tanner SM, Brinks KF (2007) Reconstruction of the proximal tibiofibular joint: a case report. Clin J Sport Med 17(1):75–77
Ozcan O, Eroglu M, Boya H, Kaya Y. (2016) Proximal tibiofibular joint pain versus peroneal nerve dysfunction: clinical results of closed-wedge high tibial osteotomy performed with proximal tibiofibular joint disruption. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4066-5
Horst PK, LaPrade RF (2010) Anatomic reconstruction of chronic symptomatic anterolateral proximal tibiofibular joint instability. Knee Surg Sports Traumatol Arthrosc 18(11):1452–1455
Williams BT, James EW, LaPrade RF (2016) A physeal-sparing fibular collateral ligament and proximal tibiofibular joint reconstruction in a skeletally immature athlete. Knee Surg Sports Traumatol Arthrosc 24(3):661–665
Chahla J, von Bormann R, Engebretsen L, LaPrade RF (2016) Anatomic posterior cruciate ligament reconstruction: state of the art. J ISAKOS 1(5):292–302
Geeslin AG, LaPrade RF (2011) Outcomes of treatment of acute grade-III isolated and combined posterolateral knee injuries: a prospective case series and surgical technique. J Bone Jt Surg Am 93(18):1672–1683
LaPrade RF, Moulton SG, Nitri M, Mueller W, Engebretsen L (2015) Clinically relevant anatomy and what anatomic reconstruction means. Knee Surg Sports Traumatol Arthrosc 23(10):2950–2959
LaPrade RF, Spiridonov SI, Coobs BR, Ruckert PR, Griffith CJ (2010) Fibular collateral ligament anatomical reconstructions: a prospective outcomes study. Am J Sports Med 38(10):2005–2011
Laprade RF, Wijdicks CA (2012) Surgical technique: development of an anatomic medial knee reconstruction. Clin Orthop Relat Res 470(3):806–814
Spiridonov SI, Slinkard NJ, LaPrade RF (2011) Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Jt Surg Am 93(19):1773–1780
Acknowledgements
The authors would like to thank David Civitarese, BA, for his help with specimen acquisition and Grant J. Dornan, M.S. for his assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. LaPrade is a paid consultant and recieves IP royalties and research support from Arthrex, Inc., Össur, and Smith & Nephew. Dr. Moatshe has received research grants from Arthrex Inc. and South Eastern Norway Health Authorities (Helse Sør-Øst), Norway.
Funding
This study was internally funded by the Steadman Philippon Research Institute.
Ethical approval
The article does not contain any studies with human participants or patient data. Cadaveric studies are exempted from IRB at Steadman Philippon Research Institute.
Additional information
Investigation performed at the Department of BioMedical Engineering, Steadman Philippon Research Institute, Vail, Colorado.
Rights and permissions
About this article
Cite this article
Marchetti, D.C., Chahla, J., Moatshe, G. et al. Quantitative radiographic assessment of the anatomic attachment sites of the anterior and posterior complexes of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc 26, 1104–1109 (2018). https://doi.org/10.1007/s00167-017-4511-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4511-0