Abstract
Purpose
The purpose of the study was to determine the influence of femoral and tibial bone morphology on the amount of femoral and tibial tunnel widening after primary anatomic ACL reconstruction. It was hypothesized that tibial and femoral bone morphology would be significantly correlated with tunnel widening after anatomic ACL reconstruction.
Methods
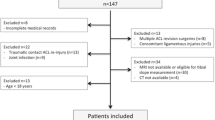
Forty-nine consecutive patients (mean age 21.8 ± 8.1 years) who underwent primary single-bundle anatomic ACL reconstruction with hamstring autograft were enrolled. Two blinded observers measured the bone morphology of tibia and femur including, medial and lateral tibial posterior slope, medial and lateral tibial plateau width, medial and lateral femoral condyle width, femoral notch width, and bicondylar width on preoperative magnetic resonance imaging (MRI) scans. Tibial and femoral tunnel width at three points (aperture, mid-section, and exit) were measured on standard anteroposterior radiograph from 1 week and 1 year postoperatively (mean 12.5 ± 2 months). Tunnel width measurements at each point were compared between 1 week and 1 year to calculate percent of tunnel widening over time. Multivariable linear regression was used to analyze correlations between bone morphology and tunnel widening.
Result
Increase in lateral tibial posterior slope was the only independent bony morphology characteristics that was significantly correlated with an increased tibial tunnel exit widening (R = 0.58). For every degree increase in lateral tibial posterior slope, a 3.2% increase in tibial tunnel exit width was predicted (p = 0.003). Excellent inter-observer and intra-observer reliability were determined for the measurements (ICC = 0.91 and 0.88, respectively).
Conclusion
Increased lateral tibial posterior slope is an important preoperative anatomic factor that may predict tunnel widening at the tibial tunnel exit. In regard to clinical relevance, the results of this study suggest that lateral tibial posterior slope be measured preoperatively. In patients with increased lateral tibial posterior slope, more rigid graft fixation and a more conservative physical therapy regiment may be preferred.
Level of evidence IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tunnel widening after ACL reconstruction (ACLR) is a common finding. The incidence of tunnel widening after single-bundle ACLR has been reported between 30.1–100% on femoral side and 20.9–73.9% on the tibia side [3, 7, 16, 32]. Interplay between biological and mechanical factors is known to be responsible for tunnel widening. Biological factors such as tumor necrosis factor-α and cytokines released into the synovial joint can affect the osteosynthesis process while mechanical factors such as tunnel position, fixation devices, and graft tension can affect and increase the force on the graft, causing tunnel widening [8, 13, 18, 20, 21, 23, 29, 31, 38].
In the clinical setting, concerns about tunnel widening arise when surgeons face delay in graft-tunnel healing after ACLR and revision cases. Although the role of tunnel widening in graft incorporation and subsequent healing is controversial, its importance in revision cases with severe tunnel widening is well known. Staged surgery could increase the cost and risk related to the second surgery, and delay the return to daily living activities and sport [37].
Recently, the role of tibial and femoral bony morphology on the ACL injury mechanism,[30] ACL failure [1, 4], and early graft failure after ACLR [6] has been appreciated. Narrow notch width, shallow medial tibial plateau, and increased medial and lateral posterior tibial slopes are known risk factors for ACL injury [1, 11, 39]. Increased lateral tibia posterior slope has also been found to be related to a grade 3 pivot shift [26, 30]. Bone morphology has a major effect on the forces applied on the knee, and therefore, it is stable during activities. To the best of our knowledge, there are no studies currently in the literature that examine the role of tibial and femoral bone morphology on tunnel widening after primary anatomic ACLR. Therefore, the goal of this study was to determine the correlation of bone morphology of the tibia and femur as measured on preoperative MRI scans, with tibial and femoral tunnel widening measured on standard anteroposterior radiographs 1 year after anatomic ACLR. It was hypothesized that tibial and femoral bone morphology would be significantly correlated with tunnel widening after anatomic ACLR.
Materials and methods
Between 2010 and 2014, patients with complete ACL rupture who underwent primary single bundle anatomic ACL reconstruction with hamstring autograft were included in this study. Exclusion criteria were multi-ligamentous injury, previous knee surgery or injury, limb malalignment, systemic connective tissue disorders, open growth plates, and ACL augmentation. The senior author performed all surgeries based on an anatomic ACLR concept [24, 25]. ACLR was done by a medial portal drilling technique in the center of the femoral footprint and tibial tunnel drilling in the center of the tibial tunnel. Fixation devices were an Endobutton (Smith & Nephew, Andover, MA, USA) and bioabsorbable interference screw on the femoral and tibial side, respectively. A standard postoperative rehabilitation protocol was done for all patients [36]. A rehabilitation program with emphasis on regaining range of motion and partial weight bearing for the first 6–8 weeks and then achieving full motion and return to normal daily activities by 3–6 months was done with all patients. Return to sport ranged from 6 months to 1 year after surgery, based on sport specific testing [36]. The stability of the reconstructions 1 year after anatomic ACLR was confirmed in all patients clinically and also by KT-1000 (MEDmetric® Corporation, San Diego, CA).
Bone morphology measurements
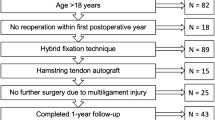
All patients had preoperative MRI scans of the injured knee, with the patients in supine position and extended knee, (3-mm slice thickness, 1.5-T, GE Signa, GE Healthcare, USA). T1 coronal and sagittal image sequences were used to evaluate femoral and tibial bone morphology. Two independent observers, who were blinded to the patients’ medical records, measured tibial and femoral bony morphology on MRIs using a digital image system (iSite, Philips Medical System, Best, the Netherlands—software accuracy = 0.1 mm and 0.1°). A coronal cut in which both tibial spines were most prominent and the roof of the femoral notch was visible was selected to measure medial–lateral (ML) diameter of the medial tibial plateau (MTP), lateral tibial plateau (LTP), medial femoral condyle (MFC), lateral femoral condyle (LFC), femoral notch width (NW), and femoral bicondylar width (BW). The MFC and LFC measurements were done on the articular surface from the intercondylar notch to the borders of the condyles, respectively. For the MTP and LTP, two longitudinal lines passing from the tips of the tibial spines were drawn, then the vertical distance from this line to the border of each tibial plateau was measured (Fig. 1a). NW and BW measurements were done at the level of the popliteal groove (Fig. 1b).
Coronal T1-weighted MRI of the knee was used to measure bone morphology. Medial femoral condyle width was measured from medial border of intercondylar notch to the medial border of medial femoral condyle. Lateral femoral condyle width was measured from lateral border of intercondylar notch to the lateral border of lateral femoral condyle. Medial tibial plateau and lateral tibial plateau widths were measured from medial and lateral borders of tibial plateau to the vertical lines crossing from medial and lateral tibial plateau, respectively. Notch width and bicondylar width measurements were done at the level of the popliteal groove
Medial and lateral tibial posterior slopes were determined based on previously published methods [12]. The central sagittal MRI image with the following criteria was used to determine the longitudinal axis of the tibia: (1) the anterior and posterior proximal tibial cortices be seen in concave shape, and (2) intercondylar eminence and its PCL attachment. A circle was fitted to the proximal tibia, tangential to the cortexes and a second circle was fitted distally with its center placed on the border of the first circle. The line connecting the center of these two circles was known as the longitudinal axis (Fig. 2a). The mid-sagittal images of the medial and lateral femoral condyles were selected and the angle made by longitudinal axis and the line connecting the anterior and posterior articular surface of tibial plateau were considered the medial and lateral tibial posterior slopes, respectively (Fig. 2b, c).
Sagittal T1-weighted MRI of the knee was used to measure medial and lateral posterior tibial slopes. a Mid-sagittal image of knee MRI was selected and two circles fitted to the proximal tibia are drawn. The interconnecting line passing through the center of both circles was considered the longitudinal tibial axis. b Medial tibial plateau posterior slope was determined in the mid-sagittal image of the medial femoral condyle. The angle between the line fitting the medial tibial plateau (dashed line) and the line perpendicular to the longitudinal tibial axis (arrow line) was considered the medial tibial plateau posterior slope. c Lateral tibial plateau posterior slope was determined in the mid-sagittal image of the lateral femoral condyle. The angle between line fitting the lateral tibial plateau (dashed line) and the line perpendicular to the longitudinal tibial axis (arrow line) was considered the lateral tibial plateau posterior slope
Tunnel widening measurement
Standard anteroposterior radiograph of the knee obtained during the first week and 1 year after surgery (mean: 12.5 ± 2 months) was used to measure tibial and femoral tunnel width. The distances between borders of the tunnel perpendicular to the long axis of tunnel were measured at 3 levels as aperture, mid-section, and exit (Fig. 3).
Tunnel width measurements at each point were compared between 1 week and 1 year postoperatively to calculate the percent of tunnel widening.
Institutional review board approval of the University of Pittsburgh (ID: MOD12020619-08/PRO12020619) was obtained prior to the start of this study.
Statistical analysis
Statistical analysis was performed using SPSS (version 22.0. Armonk, NY: IBM Corp). Intra-class correlation coefficients (ICC) were calculated to evaluate the inter-observer and intra-observer reliability of all bone morphology and tunnel diameter measurements. Multivariable linear regression was used to analyze correlation between bone morphology and tunnel widening. Statistical significance was set at p < 0.05.
Results
Forty-nine consecutive patients consisting of 15 males and 34 females were enrolled in the study. Demographics and injury mechanism are shown in Table 1.
Among bone morphology, increase in lateral tibial posterior slope was the only independent bone morphology that was significantly correlated with increased tibial tunnel exit widening (Correlation coefficient = 0.58) (Fig. 4). For every degree increase in lateral tibial posterior slope, a 3.2% increase in tibial tunnel exit width was predicted (p = 0.003). Excellent inter-observer and intra-observer reliability were determined for the measurements (ICC = 0.91 and 0.88, respectively).
There were no significant correlations between other bone morphologies and tunnel widening on the tibia and femur (Table 2).
Discussion
The most important finding of this study was that a significant positive correlation existed between lateral tibial posterior slope and the percentage of tibial tunnel exit widening. Other bone morphologies were not significantly correlated with percentage of femoral or tibial tunnel widening. Bony morphology has been evaluated in patients, but never has been related to tunnel widening, only to pivot shift mechanism, ACL injury, and failure of ACLR. Kujala et al. [17] first described the relationship between a positive pivot shift and configuration of the lateral tibia plateau. Afterward, Brandon et al. [4] confirmed the effect of greater posterior tibial slope on high-grade pivot shift and ACL rupture. A recent study [33] demonstrated an increased posterior inferior lateral tibial articular cartilage slope and a decreased femoral notch width in females as predisposing factors for ACL injury. Another study revealed that a more spherical shape of the femoral condyle was related with disability after ACLR and failure of non-operative treatment [35]. Recently, the effect of increased lateral tibial posterior slope as a predisposing factor for early graft failure after ACL reconstruction has been reported [6].
Severe tunnel widening is an important issue with regard to ACL revision surgery. It may necessitate a two-stage procedure; first with bone grafting followed by a separate revision ACL reconstruction [19]. Furthermore, two stage surgeries have some disadvantages to the patient in terms of expense and time required to return to previous activities [37]. If a one-stage revision is chosen, patients are at risk for suboptimal tunnel placement, further tunnel widening, or even fracture [2, 21]. Etiology and natural history of tunnel widening is not completely understood. The effect of mechanical and biological factors has been evaluated, but the effect of bony morphology of the tibia and femur on tunnel widening has not been assessed.
The implications of tunnel enlargement are not known. One randomized control trial (RCT) [14] found a relationship between tunnel enlargement and both anterior and rotational laxity, as well as clinical outcome scores after primary ACLR. However, other studies revealed no significant correlation between tunnel enlargement and functional outcome scores and anterior or rotational laxity [9, 40]. It could be concluded that the effect of tunnel widening on clinical outcomes and knee stability after primary ACLR is still unclear.
Mechanical factors including excessive graft-tunnel motion, tunnel position, graft tension, type of graft (hamstring or bone patella tendon bone), type of graft fixation, and unprotected rehabilitation [5, 10, 20, 28, 34] are among the reasons for tunnel widening. In an RCT of 100 patents, the authors reported a significant reduction of femoral and tibial tunnel widening using fixation points close to the joint when compared with the system that has long distance between fixation points [9]. Another study showed that tunnel widening is more common and greater with hamstring grafts compared to patellar tendon grafts. The authors postulate that the patellar tendon bone block likely allows improved healing which they believe decreases the incidence and extend of tunnel widening.
Biological factors can also affect tunnel enlargement when osteoclast activity outpaces osteoblast activity, leading to bone resorption. The effect of Inflammatory mediators such as tumor necrosis factor-α and cytokines released into the synovial joint after ACL reconstruction [18, 29, 31], biological reaction to bioabsorbable screws [8, 23], and factors related to the allograft [27] have been identified. In a MRI study evaluating tunnel widening after ACL reconstruction comparing bioabsorbable to metal screw fixation of autologous hamstring graft, the authors demonstrated more femoral tunnel widening in bioabsorbable fixation group [22]. The authors believe a larger inflammatory reaction may occur with bioabsorbable screws which may be the cause for greater tunnel widening compared with metal screw fixation. Another prospective study evaluated tunnel widening comparing hamstring autograft versus anterior tibialis allograft and revealed a higher incidence of tunnel widening in allograft group. They concluded the biological factors in allograft could be the reason for tunnel widening.
In this study, an attempt was made to control the other known mechanical factors that could interfere with tunnel widening. Baumfeld et al. [3] showed that different graft fixation devices can affect the amount of tunnel widening. Therefore, only patients whose grafts were fixed with the same device were enrolled. Endobutton (Smith & Nephew, Andover, MA, USA) and bioabsorbable interference screw were used to fix the femoral and tibial side. Clatworthy et al. [7] found differences in tunnel widening after reconstruction in a patellar tendon group compared with a hamstring tendon group, while Jia et al. [15] demonstrated greater tunnel enlargement with allograft versus autograft. Our study consists of patients only reconstructed with hamstring autograft in an attempt to control for possible differences. Lorio et al. [13] demonstrated less tunnel enlargement in anatomic ACLR when compared with non-anatomic. All patients underwent anatomic ACLR in the present study. Hantes et al. [10] showed that tunnel enlargement occurs after ACL reconstruction in patients with early motion (unrestricted range of motion without brace and full weight bearing with crutch immediately after ACLR) versus late motion (restricted range of motion of 0°–60° for the first 3 weeks and 0°–90° for 3 more weeks and partial weight bearing for all the 6 weeks). All the patients in this study had the same standard rehabilitation protocol (late motion) after surgery.
In the present study, MRI was used to assess bony morphology, thereby eliminating the effect of overlapping of the bony landmarks and increasing the accuracy of measurements. The effect of tibial and femoral bony morphology on tunnel widening may be similar to its effect on the pivot shift mechanism, ACL injury, and early graft failure after reconstruction. Previous studies showed that the lateral tibial plateau is more important than the medial plateau in the pivot shift mechanism and therefore places an increased force on the ACL [17, 30]. The differences in the shapes of tibial plateau could explain the difference in their effect on the forces applied to the ACL. The medial tibial plateau has a concave shape and therefore provides more stability, while the lateral tibial plateau is convex, with greater potential for motion during activities. On the other hand, increased lateral posterior tibial slope can cause increased anterior tibial translation, creating a ramp allowing for more anterior tibial translation. These factors increase the forces on the graft and motion at the graft-tunnel junction, possibly leading to tunnel widening.
This study is the first in which the authors are aware to determine the role of preoperative factors on tunnel enlargement with the goal of avoiding this complication in the future. It could be recommended that patients with greater tibial posterior slope have a preoperative consultation about postoperative rehabilitation programs and undergo a more conservative physical therapy program after surgery to decrease the forces on the graft as well as graft-tunnel motion. Using more rigid fixation on the tibial side of these patients could be another consideration.
This study does have limitations. First, tunnel diameter was evaluated in standard plain radiograph with likely less accuracy than a computed tomography (CT) scan. Further, a larger sample size would strengthen this study and may provide greater insight into other bony morphologies. In particular, distal femoral shape and other soft tissue elements may affect the graft-junction motion and subsequent tunnel enlargement. Although these limitations exist, digital plane radiography is considered an accurate manner to detect tunnel widening after ACLR and has the advantages of easy accessibility and cost-effectiveness [38].
Regarding the clinical relevance, the results of this study suggest that lateral tibial posterior slope be measured preoperatively. Facing increased lateral tibial posterior slope preoperatively, surgeons may be able to avoid tibial tunnel exit widening by considering more rigid graft fixation and more conservative physical therapy postoperatively.
Conclusion
Increased lateral tibial posterior slope is an important preoperative anatomic factor that may predict tunnel widening at the tibial tunnel exit. In regard to clinical relevance, the results of this study suggest that lateral tibial posterior slope be measured preoperatively. In patients with increased lateral tibial posterior slope, more rigid graft fixation a more conservative physical therapy regiment may be preferred.
References
Alentorn-Geli E, Pelfort X, Mingo F, Lizano-Diez X, Leal-Blanquet J, Torres-Claramunt R, Hinarejos P, Puig-Verdie L, Monllau JC (2015) An evaluation of the association between radiographic intercondylar notch narrowing and anterior cruciate ligament injury in men: the notch angle is a better parameter than notch width. Arthroscopy 31(10):2004–2013
Anderson AW, Smith JJ (2009) Proximal tibial fracture after patellar tendon autograft for ipsilateral ACL reconstruction. J Knee Surg 22(02):142–144
Baumfeld JA, Diduch DR, Rubino LJ, Hart JA, Miller MD, Barr MS, Hart JM (2008) Tunnel widening following anterior cruciate ligament reconstruction using hamstring autograft: a comparison between double cross-pin and suspensory graft fixation. Knee Surg Sports Traumatol Arthrosc 16(12):1108–1113
Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF (2006) The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 22(8):894–899
Choi NH, Yang BS, Victoroff BN (2016) Clinical and radiological outcomes after hamstring anterior cruciate ligament reconstructions: comparison between fixed-loop and adjustable-loop cortical suspension devices. Am J Sports Med. doi:10.1177/0363546516674183
Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL (2015) Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med 43(10):2510–2514
Clatworthy MG, Annear P, Bulow JU, Bartlett RJ (1999) Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthrosc 7(3):138–145
Drogset JO, Grontvedt T, Jessen V, Tegnander A, Mollnes TE, Bergh K (2006) Comparison of in vitro and in vivo complement activation by metal and bioabsorbable screws used in anterior cruciate ligament reconstruction. Arthroscopy 22(5):489–496
Fauno P, Kaalund S (2005) Tunnel widening after hamstring anterior cruciate ligament reconstruction is influenced by the type of graft fixation used: a prospective randomized study. Arthroscopy 21(11):1337–1341
Hantes ME, Mastrokalos DS, Yu J, Paessler HH (2004) The effect of early motion on tibial tunnel widening after anterior cruciate ligament replacement using hamstring tendon grafts. Arthroscopy 20(6):572–580
Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck JR, Schutt RC Jr, Dabezies E, Beynnon BD (2010) Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med 38(1):54–62
Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP (2009) Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res 467(8):2066–2072
Iorio R, Vadala A, Argento G, Di Sanzo V, Ferretti A (2007) Bone tunnel enlargement after ACL reconstruction using autologous hamstring tendons: a CT study. Int Orthop 31(1):49–55
Jarvela T, Moisala AS, Paakkala T, Paakkala A (2008) Tunnel enlargement after double-bundle anterior cruciate ligament reconstruction: a prospective, randomized study. Arthroscopy 24(12):1349–1357
Jia YH, Sun PF (2015) Comparison of clinical outcome of autograft and allograft reconstruction for anterior cruciate ligament tears. Chin Med J (Engl) 128(23):3163–3166
Kawaguchi Y, Kondo E, Kitamura N, Kai S, Inoue M, Yasuda K (2011) Comparisons of femoral tunnel enlargement in 169 patients between single-bundle and anatomic double-bundle anterior cruciate ligament reconstructions with hamstring tendon grafts. Knee Surg Sports Traumatol Arthrosc 19(8):1249–1257
Kujala UM, Nelimarkka O, Koskinen SK (1992) Relationship between the pivot shift and the configuration of the lateral tibial plateau. Arch Orthop Trauma Surg 111(4):228–229
Leonardi AB, Duarte Junior A, Severino NR (2014) Bone tunnel enlargement on anterior cruciate ligament reconstruction. Acta Ortop Bras 22 (5):240–244.
Maak TG, Voos JE, Wickiewicz TL, Warren RF (2010) Tunnel widening in revision anterior cruciate ligament reconstruction. J Am Acad Orthop Surg 18(11):695–706
Mermerkaya MU, Atay OA, Kaymaz B, Bekmez S, Karaaslan F, Doral MN (2015) Anterior cruciate ligament reconstruction using a hamstring graft: a retrospective comparison of tunnel widening upon use of two different femoral fixation methods. Knee Surg Sports Traumatol Arthrosc 23(8):2283–2291
Mithöfer K, Gill TJ, Vrahas MS (2004) Tibial plateau fracture following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 12(4):325–328
Moisala A-S, Järvelä T, Paakkala A, Paakkala T, Kannus P, Järvinen M (2008) Comparison of the bioabsorbable and metal screw fixation after ACL reconstruction with a hamstring autograft in MRI and clinical outcome: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 16(12):1080–1086
Park MC, Tibone JE (2006) False magnetic resonance imaging persistence of a biodegradable anterior cruciate ligament interference screw with chronic inflammation after 4 years in vivo. Arthroscopy 22 (8):911 e911–914.
Rahnemai-Azar AA, Sabzevari S, Irarrázaval S, Chao T, Fu F (2016) Anatomical Individualized ACL Reconstruction. Arch Bone Jt Surg 4 (4):291–297
Rahnemai-Azar AA, Sabzevari S, Irarrázaval S, Chao T, Fu F (2016) Restoring nature through individualized anatomic anterior cruciate ligament reconstruction surgery. Arch Bone Jt Surg 4 (4):289–290
Rahnemai-Azar AA, Yaseen Z, van Eck CF, Irrgang JJ, Fu FH, Musahl V (2016) Increased lateral tibial plateau slope predisposes male college football players to anterior cruciate ligament injury. J Bone Joint Surg Am 98(12):1001–1006
Robbrecht C, Claes S, Cromheecke M, Mahieu P, Kakavelakis K, Victor J, Bellemans J, Verdonk P (2014) Reliability of a semi-automated 3D-CT measuring method for tunnel diameters after anterior cruciate ligament reconstruction: A comparison between soft-tissue single-bundle allograft vs. autograft. Knee 21(5):926–931
Rodeo SA, Kawamura S, Kim HJ, Dynybil C, Ying L (2006) Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: an effect of graft-tunnel motion? Am J Sports Med 34(11):1790–1800
Silva A, Sampaio R, Pinto E (2010) Femoral tunnel enlargement after anatomic ACL reconstruction: a biological problem? Knee Surg Sports Traumatol Arthrosc 18(9):1189–1194
Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H (2016) Risk factors associated with grade 3 pivot shift after acute anterior cruciate ligament injuries. Am J Sports Med 44(2):362–369
Starantzis KA, Mastrokalos D, Koulalis D, Papakonstantinou O, Soucacos PN, Papagelopoulos PJ (2014) The potentially positive role of PRPs in preventing femoral tunnel widening in acl reconstruction surgery using hamstrings: a clinical study in 51 patients. J Sports Med. doi:10.1155/2014/789317
Struewer J, Efe T, Frangen TM, Schwarting T, Buecking B, Ruchholtz S, Schuttler KF, Ziring E (2012) Prevalence and influence of tibial tunnel widening after isolated anterior cruciate ligament reconstruction using patella-bone-tendon-bone-graft: long-term follow-up. Orthop Rev (Pavia) 4(2):e21
Sturnick DR, Vacek PM, DeSarno MJ, Gardner-Morse MG, Tourville TW, Slauterbeck JR, Johnson RJ, Shultz SJ, Beynnon BD (2015) Combined anatomic factors predicting risk of anterior cruciate ligament injury for males and females. Am J Sports Med 43(4):839–847
Tsuda E, Fukuda Y, Loh JC, Debski RE, Fu FH, Woo SL (2002) The effect of soft-tissue graft fixation in anterior cruciate ligament reconstruction on graft-tunnel motion under anterior tibial loading. Arthroscopy 18(9):960–967
van Diek FM, Wolf MR, Murawski CD, van Eck CF, Fu FH (2014) Knee morphology and risk factors for developing an anterior cruciate ligament rupture: an MRI comparison between ACL-ruptured and non-injured knees. Knee Surg Sports Traumatol Arthrosc 22(5):987–994
van Eck CF, Fu FH (2014) Anatomic anterior cruciate ligament reconstruction using an individualized approach. Asia-Pacific J Sports Med Arthrosc Rehab Tech 1 (1):19–25
Weber AE, Delos D, Oltean HN, Vadasdi K, Cavanaugh J, Potter HG, Rodeo SA (2015) Tibial and femoral tunnel changes after ACL reconstruction: a prospective 2-year longitudinal MRI study. Am J Sports Med 43(5):1147–1156
Webster KE, Feller JA, Elliott J, Hutchison A, Payne R (2004) A comparison of bone tunnel measurements made using computed tomography and digital plain radiography after anterior cruciate ligament reconstruction. Arthroscopy 20(9):946–950
Wolf MR, Murawski CD, van Diek FM, van Eck CF, Huang Y, Fu FH (2015) Intercondylar notch dimensions and graft failure after single- and double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 23(3):680–686
Yoon SJ, Yoon YC, Bae SY, Wang JH (2015) Bone tunnel diameter measured with ct after anterior cruciate ligament reconstruction using double-bundle auto-hamstring tendons: clinical implications. Korean J Radiol 16(6):1313–1318
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
Patients gave informed consent that data would be published.
Additional information
Investigation performed at the University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania -USA.
Rights and permissions
About this article
Cite this article
Sabzevari, S., Rahnemai-Azar, A.A., Shaikh, H.S. et al. Increased lateral tibial posterior slope is related to tibial tunnel widening after primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 25, 3906–3913 (2017). https://doi.org/10.1007/s00167-017-4435-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4435-8