Abstract
Purpose
The purpose of this study was to investigate the morphology of the discoid lateral meniscus sequentially following a partial meniscectomy with repair using magnetic resonance imaging (MRI).
Methods
Nine patients with a symptomatic discoid lateral meniscus with a peripheral tear were enrolled in this study, and a partial meniscectomy with repair was performed arthroscopically. An MRI examination was performed 2 weeks after surgery (before weight bearing was permitted) and again 6 months after surgery (when sporting activities could resume). The width, height and distance of the discoid lateral meniscus were measured. The distance was defined as the distance between the edges of the discoid lateral meniscus and the tibia.
Results
The width of the anterior, middle and posterior segments significantly decreased from 2 weeks to 6 months after surgery. The height of the middle and posterior segments significantly increased from 2 weeks to 6 months after surgery, whereas the height of the anterior segment did not significantly change. The distance of the anterior, middle and posterior segments significantly decreased from 2 weeks to 6 months after surgery.
Conclusion
The discoid lateral meniscus exhibited deformation and extrusion from 2 weeks to 6 months after a partial meniscectomy with repair. Therefore, the function of load transmission might not be maintained appropriately after surgery.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A discoid lateral meniscus (DLM) is a morphologic abnormality of the knee, first reported by Young in 1889 [38]. The prevalence of DLM has been reported to range from 0.4 to 17%, with higher rates in Asian populations [6, 19, 20, 24, 28, 30]. Many children with a DLM remain asymptomatic and require no treatment, while children and adolescents who have an unstable DLM with a peripheral tear often exhibit symptoms including pain, snapping and a decreased range of motion [9, 35]. Therefore, in these patients, surgical treatment should be considered.
Although the traditional treatment for a symptomatic DLM with a peripheral tear was a total or subtotal meniscectomy [5, 7, 19, 32, 35], long-term studies have shown that there is a high rate of osteoarthritic changes following a total or subtotal meniscectomy [2, 4, 11, 27]. These osteoarthritic changes are expected because the meniscus has important functions, including load transmission, shock absorption and joint conformity [11, 13, 18, 29]. Therefore, a total or subtotal meniscectomy is currently avoided as much as possible.
With the improvement of arthroscopic techniques, a partial meniscectomy with repair has been favoured to restore meniscal function. This procedure involves a partial meniscectomy to reshape the meniscus in conjunction with the repair of any detached or unstable fragments. Recently, some studies have reported successful short-term clinical results following a partial meniscectomy with repair [1, 3, 4, 10, 14, 37]. However, whether the function of the post-operative DLM is maintained remains unclear. The purpose of this study was to investigate the morphology of a DLM sequentially following a partial meniscectomy with repair using magnetic resonance imaging (MRI) to evaluate the remaining function of the post-operative DLM.
Materials and methods
A total of 12 consecutive patients with a symptomatic DLM with a peripheral tear underwent a partial meniscectomy with repair at Hoshigaoka Medical Center between 2011 and 2014. The diagnosis of DLM with a peripheral tear was made via a preoperative MRI [23]. Although all patients provided the informed consent for the post-operative MRI analysis, one patient underwent revision surgery due to reinjury, and two patients were excluded due to low-quality MRI images. Thus, only the remaining nine patients were enrolled in this study. The patients consisted of five males and four females aged between 10 and 26 years (median: 14 years). The average interval from the time of the injury until surgery was 5.5 months (range 5 days–1 year). Eight patients had a complete DLM, and one had an incomplete DLM [36]. All of the patients had an unstable peripheral tear in the vascular zone. The site of the tear was anterior in one patient, posterior in two, anterior–posterior in three, middle–posterior in two and both anterior and posterior in one.
Surgical procedure
A partial meniscectomy with repair was performed arthroscopically while the patient was under general anaesthesia, using anterolateral, anteromedial and far anteromedial portals (Fig. 1). First, a partial meniscectomy was performed to remove the central portion of the DLM and to restore the normal width of the peripheral rim. Second, the peripheral tears were repaired by placing vertical sutures at intervals of 5 mm. Tears in the anterior segment were repaired with an all-inside technique using a suture hook (Linvatec, Largo, FL, USA), whereas tears in the middle to posterior segments were repaired with an inside-out technique using a zone-specific cannula (Linvatec, Largo, FL, USA) or a Henning’s instrument (Stryker, Kalamazoo, MI, USA) [31]. When the tear site could be approached with a Henning’s instrument, stacked sutures were preferred [16, 17].
Arthroscopic views of the right knee. a A complete DLM was displaced. b The central portion of the DLM was retracted with a probe, and a peripheral tear (black arrow) in the posterior segment was visualized. c A partial meniscectomy was performed to remove the central portion of the DLM and to restore the normal width of the peripheral rim. d A peripheral tear in the posterior segment was repaired with an inside-out technique. e An overview following a partial meniscectomy with repair
To enhance the healing of the meniscus, we prepared a fibrin clot from 20 mL of peripheral blood from the patient [16, 26]. The fibrin clot was introduced into the tear site and fixed by fastening the sutures outside the joint.
Rehabilitation program
After immobilization with a brace for 1–2 weeks, range-of-motion exercises were initiated. Partial weight bearing was allowed 3 weeks after surgery, followed by full weight bearing at 4 weeks. Resumption of previous sporting activities was permitted 6 months after surgery.
MRI evaluation
An MRI examination was performed 2 weeks after surgery (before weight bearing was permitted) and again 6 months after surgery (when sporting activities could resume) using a 1.5-Tesla MR scanner (EXCELART Vantage; Toshiba, Tochigi, Japan). During image acquisition, the patient’s knee was at a 15° flexion in the supine position. The MR images were obtained using the following conditions: repetition time of 4000 ms; echo time of 90 ms; 4-mm-thick slice with a 0.8-mm gap between slices; a 16-cm field of view; and a matrix size of 192 × 192.
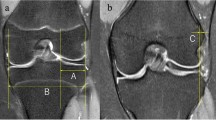
First, the width and height of the anterior segment were measured in the sagittal slice, which passed through the centre of the lateral femoral condyle, and those of the posterior segment were measured in the same slice (Fig. 2a, b). The width and height of the middle segment were measured in the coronal slice on which the middle segment appeared to be the smallest (Fig. 2d, e).
MRI measurements. The width and height of the anterior segment were measured in the sagittal slice, which passed through the centre of the lateral femoral condyle, and those of the posterior segment were measured in the same slice (a, b). The width and height of the middle segment were measured in the coronal slice on which the middle segment appeared to be the smallest (d, e). The distance of the anterior and posterior segments was measured in the above-mentioned sagittal slice. A line perpendicular to the joint line was created tangentially to the anterior edge of the tibia (line A). The distance of the anterior segment was defined as the distance between the anterior edge of the DLM and line A. Line P was created tangentially to the posterior edge of the tibia, and the distance of the posterior segment was measured in the same manner (c). Similarly, in the above-mentioned coronal slice, line M was created tangentially to the lateral edge of the tibia, and the distance of the middle segment was measured (f). With respect to the distance, positive values indicated that the DLM existed inside of the tibial plateau, whereas negative values denoted an extrusion of the DLM
Second, the distance of the anterior and posterior segments was measured in the above-mentioned sagittal slice. A line perpendicular to the joint line was created tangentially to the anterior edge of the tibia (line A). The distance of the anterior segment was defined as the distance between the anterior edge of the DLM and line A. Line P was created tangentially to the posterior edge of the tibia, and the distance of the posterior segment was measured in the same manner (Fig. 2c). Similarly, in the above-mentioned coronal slice, line M was created tangentially to the lateral edge of the tibia, and the distance of the middle segment was measured (Fig. 2f). With respect to the distance, positive values indicated that the DLM existed inside of the tibial plateau, whereas negative values denoted an extrusion of the DLM.
The reliability calculations were based on each parameter measured by the same observer (repeated three times) and by three different observers. The intra- and inter-observer intra-class correlation coefficients (ICC) and limits of agreement (LOA) are presented in Table 1.
We obtained informed consent from all subjects, and the appropriate institutional review board of Hoshigaoka Medical Center for human subject research approved this study (ID: 1603).
Statistical analysis
The Wilcoxon signed-rank test was used to compare the values of the two periods. Differences were considered statistically significant at a value of P < 0.05. A power analysis was performed with the power, α, difference and standard deviation set at 0.8, 0.05, 4.0 and 3.1, respectively, according to the width of the middle segment. The analysis revealed that a minimum of eight patients was required for the Wilcoxon signed-rank test to detect a difference between the two periods.
Results
Six months after surgery, none of the patients experienced pain or any loss of range of motion. In addition, all of the patients were able to return to their previous sporting activities.
The width of the anterior, middle and posterior segments significantly decreased from 2 weeks (12.9 ± 2.9, 11.0 ± 3.9 and 10.9 ± 2.5 mm, respectively) to 6 months (10.5 ± 3.3, 6.9 ± 4.2 and 9.6 ± 2.1 mm, respectively) after surgery (Fig. 3a).
Width (a), height (b) and distance (c) of DLM. White and black bars represent the measured values 2 weeks and 6 months after surgery, respectively. With respect to the distance, positive values indicate that the DLM exists inside of the tibial plateau, whereas negative values denote an extrusion of the DLM. *P < 0.05
The height of the middle and posterior segments significantly increased from 2 weeks (5.7 ± 2.2 and 6.2 ± 1.6 mm, respectively) to 6 months (7.4 ± 2.7 and 7.7 ± 2.6 mm, respectively) after surgery, whereas the height of the anterior segment did not significantly change (Fig. 3b).
The distance of the anterior, middle and posterior segments significantly decreased from 2 weeks (8.7 ± 3.9, 1.6 ± 3.2 and 5.7 ± 3.0 mm, respectively) to 6 months (4.8 ± 2.6, −0.7 ± 2.5 and 4.3 ± 3.0 mm, respectively) after surgery (Fig. 3c).
Discussion
The most important finding of the present study was that the DLM exhibited deformation and extrusion from 2 weeks to 6 months after a partial meniscectomy with repair (Fig. 4). To our knowledge, this is the first report investigating the morphology of a DLM sequentially following a partial meniscectomy with repair.
The shape of the DLM immediately following a partial meniscectomy with repair resembles that of a normal meniscus. However, post-operative deformation and extrusion of the DLM were observed in the current study. One of the potential reasons for this observation is the ultrastructure of a DLM. Some reports have found that there is a decrease in the number of collagen fibres within the matrix of a DLM compared to that observed in a normal meniscus [8, 15]. Additionally, Papadopoulos et al. [25] demonstrated discontinuity and inhomogeneity of the circumferential collagen network in a DLM. According to these previous studies, the ultrastructure of a DLM is different from that of a normal meniscus. Therefore, the remaining DLM cannot effectively resist the hoop stress generated by weight bearing even if the shape immediately following surgery appears similar to a normal meniscus. Moreover, the central portion of the DLM, which is removed in a partial meniscectomy with repair, may include important fibres for the DLM to resist such hoop stress. If this is the case, deformation and extrusion following a partial meniscectomy with repair are expected results.
Meniscus-to-femoral condyle congruity is essential for meniscal function of load transmission and can be altered by abnormalities in the position and coverage of the meniscus (e.g. a meniscal extrusion) [22]. Many studies have reported that a medial meniscus extrusion is associated with the progression of knee osteoarthritis [12, 21, 33], while there are few studies regarding a lateral meniscus extrusion. However, the lateral meniscus bears as much as 70% of the load transmitted across the lateral compartment [34]. Therefore, the post-operative extrusion of the DLM observed in the present study indicates that the function of load transmission might not be appropriately maintained. In addition, the decrease in the width might also reduce the contact area between the DLM and the lateral femoral condyle, thus impairing the function of load transmission.
Previous studies have shown satisfactory clinical results following a partial meniscectomy with repair [1, 3, 4, 10, 14, 37]. Adachi et al. [1] described five cases treated with a partial meniscectomy with repair and reported that four out of five cases achieved excellent scores after more than 2 years of follow-up. Similarly, Ahn et al. retrospectively studied 28 knees after a partial meniscectomy with repair. In their study, the mean Lysholm knee scores improved from 78.5 preoperatively to 95.5 after an average follow-up of 51 months [3]. However, our results suggest that the function of load transmission might not be maintained appropriately, even if the clinical results are favourable. Consistent with our findings, Ahn et al. [4] reported that degenerative changes were observed in 39% of cases treated with a partial meniscectomy with repair after a mean follow-up of 10.1 years. However, they also stated that the partial meniscectomy with repair was associated with less progression of degenerative changes compared to a subtotal meniscectomy [4]. Therefore, we can consider a partial meniscectomy with repair to be a more favourable treatment option than a subtotal meniscectomy, even if the restoration of load transmission is not adequate.
Regarding the degree of meniscus resection, in previous studies, a partial meniscectomy was performed to leave a normal width of the peripheral rim [1, 14]. In the current study, we removed the central portion of the DLM and restored the normal width of the peripheral rim, similar to previous reports. However, the remaining DLM exhibited post-operative deformation and extrusion. Thus, as the clinical relevance, the function of load transmission might not be maintained appropriately after a partial meniscectomy with repair. To maintain the function, it may be advisable to minimize the removal of the DLM and to leave the peripheral rim with more than the normal width under the assumption that deformation and extrusion of the DLM occur after surgery.
There were several limitations associated with this study. First, the follow-up period was extended to only 6 months after surgery. The deformation and extrusion of DLM may progress for longer than 6 months after surgery. However, we expected a drastic change to be caused by weight bearing. Thus, the MRI examination was performed only twice: (1) 2 weeks after surgery (before weight bearing) and (2) 6 months after surgery (after weight bearing). Second, no radiographic evaluation was performed in the present study. However, a minimum of 1 year is required to evaluate any osteoarthritic changes on a radiograph. Therefore, we did not perform a radiographic evaluation 6 months after surgery. Third, the site of the tear lacked uniformity among the patients. Fourth, the sample size was small. However, the lack of uniformity and small sample size could not be avoided due to the rarity of a DLM. Finally, no functional assessment (e.g. Lysholm knee score) was applied in this study.
Conclusion
The DLM exhibited deformation and extrusion from 2 weeks to 6 months after a partial meniscectomy with repair.
References
Adachi N, Ochi M, Uchio Y, Kuriwaka M, Shinomiya R (2004) Torn discoid lateral meniscus treated using partial central meniscectomy and suture of the peripheral tear. Arthroscopy 20:536–542
Aglietti P, Bertini FA, Buzzi R, Beraldi R (1999) Arthroscopic meniscectomy for discoid lateral meniscus in children and adolescents: 10-year follow-up. Am J Knee Surg 12:83–87
Ahn JH, Lee SH, Yoo JC, Lee YS, Ha HC (2008) Arthroscopic partial meniscectomy with repair of the peripheral tear for symptomatic discoid lateral meniscus in children: results of minimum 2 years of follow-up. Arthroscopy 24:888–898
Ahn JH, Kim KI, Wang JH, Jeon JW, Cho YC, Lee SH (2015) Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy 31:867–873
Aichroth PM, Patel DV, Marx CL (1991) Congenital discoid lateral meniscus in children. A follow-up study and evolution of management. J Bone Joint Surg Br 73:932–936
Albertsson M, Gillquist J (1988) Discoid lateral menisci: a report of 29 cases. Arthroscopy 4:211–214
Asik M, Sen C, Taser OF, Alturfan AK, Sozen YV (2003) Discoid lateral meniscus: diagnosis and results of arthroscopic treatment. Knee Surg Sports Traumatol Arthrosc 11:99–104
Atay OA, Pekmezci M, Doral MN, Sargon MF, Ayvaz M, Johnson DL (2007) Discoid meniscus: an ultrastructural study with transmission electron microscopy. Am J Sports Med 35:475–478
Bellier G, Dupont JY, Larrain M, Caudron C, Carlioz H (1989) Lateral discoid menisci in children. Arthroscopy 5:52–56
Carter CW, Hoellwarth J, Weiss JM (2012) Clinical outcomes as a function of meniscal stability in the discoid meniscus: a preliminary report. J Pediatr Orthop 32:9–14
Dickhaut SC, DeLee JC (1982) The discoid lateral-meniscus syndrome. J Bone Joint Surg Am 64:1068–1073
Emmanuel K, Quinn E, Niu J, Guermazi A, Roemer F, Wirth W, Eckstein F, Felson D (2016) Quantitative measures of meniscus extrusion predict incident radiographic knee osteoarthritis—data from the osteoarthritis initiative. Osteoarthr Cartil 24:262–269
Fox AJ, Wanivenhaus F, Burge AJ, Warren RF, Rodeo SA (2015) The human meniscus: a review of anatomy, function, injury, and advances in treatment. Clin Anat 28:269–287
Good CR, Green DW, Griffith MH, Valen AW, Widmann RF, Rodeo SA (2007) Arthroscopic treatment of symptomatic discoid meniscus in children: classification, technique, and results. Arthroscopy 23:157–163
Hamada M, Shino K, Kawano K, Araki Y, Matsui Y, Doi T (1994) Usefulness of magnetic resonance imaging for detecting intrasubstance tear and/or degeneration of lateral discoid meniscus. Arthroscopy 10:645–653
Henning CE, Lynch MA, Yearout KM, Vequist SW, Stallbaumer RJ, Decker KA (1990) Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop Relat Res 252:64–72
Horibe S, Shino K, Nakata K, Maeda A, Nakamura N, Matsumoto N (1995) Second-look arthroscopy after meniscal repair. Review of 132 menisci repaired by an arthroscopic inside-out technique. J Bone Joint Surg Br 77:245–249
Hsieh HH, Walker PS (1976) Stabilizing mechanisms of the loaded and unloaded knee joint. J Bone Joint Surg Am 58:87–93
Ikeuchi H (1982) Arthroscopic treatment of the discoid lateral meniscus. Technique and long-term results. Clin Orthop Relat Res 167:19–28
Kwon SK, Moon HK, Choi CJ, Park SH, Lee JJ, Kim YC, Park YS, Koh YG (2015) Accelerated degeneration of the discoid lateral meniscus after medial opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 23:97–103
Lee DH, Lee BS, Kim JM, Yang KS, Cha EJ, Park JH, Bin SI (2011) Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 19:222–229
Narazaki S, Furumatsu T, Tanaka T, Fujii M, Miyazawa S, Inoue H, Shimamura Y, Saiga K, Ozaki T (2015) Postoperative change in the length and extrusion of the medial meniscus after anterior cruciate ligament reconstruction. Int Orthop 39:2481–2487
Nguyen JC, De Smet AA, Graf BK, Rosas HG (2014) MR imaging-based diagnosis and classification of meniscal tears. Radiographics 34:981–999
Ogut T, Kesmezacar H, Akgun I, Cansu E (2003) Arthroscopic meniscectomy for discoid lateral meniscus in children and adolescents: 4.5 years follow-up. J Pediatr Orthop B 12:390–397
Papadopoulos A, Kirkos JM, Kapetanos GA (2009) Histomorphologic study of discoid meniscus. Arthroscopy 25:262–268
Ra HJ, Ha JK, Jang SH, Lee DW, Kim JG (2013) Arthroscopic inside-out repair of complete radial tears of the meniscus with a fibrin clot. Knee Surg Sports Traumatol Arthrosc 21:2126–2130
Raber DA, Friederich NF, Hefti F (1998) Discoid lateral meniscus in children. Long-term follow-up after total meniscectomy. J Bone Joint Surg Am 80:1579–1586
Rohren EM, Kosarek FJ, Helms CA (2001) Discoid lateral meniscus and the frequency of meniscal tears. Skeletal Radiol 30:316–320
Roumazeille T, Klouche S, Rousselin B, Bongiorno V, Graveleau N, Billot N, Hardy P (2015) Arthroscopic meniscal allograft transplantation with two tibia tunnels without bone plugs: evaluation of healing on MR arthrography and functional outcomes. Knee Surg Sports Traumatol Arthrosc 23:264–269
Ryu K, Iriuchishima T, Oshida M, Saito A, Kato Y, Tokuhashi Y, Aizawa S (2015) Evaluation of the morphological variations of the meniscus: a cadaver study. Knee Surg Sports Traumatol Arthrosc 23:15–19
Scott GA, Jolly BL, Henning CE (1986) Combined posterior incision and arthroscopic intra-articular repair of the meniscus. An examination of factors affecting healing. J Bone Joint Surg Am 68:847–861
Sugawara O, Miyatsu M, Yamashita I, Takemitsu Y, Onozawa T (1991) Problems with repeated arthroscopic surgery in the discoid meniscus. Arthroscopy 7:68–71
Sugita T, Kawamata T, Ohnuma M, Yoshizumi Y, Sato K (2001) Radial displacement of the medial meniscus in varus osteoarthritis of the knee. Clin Orthop Relat Res 387:171–177
Walker PS, Erkman MJ (1975) The role of the menisci in force transmission across the knee. Clin Orthop Relat Res 109:184–192
Washington ER, Root L, Liener UC (1995) Discoid lateral meniscus in children. Long-term follow-up after excision. J Bone Joint Surg Am 77:1357–1361
Watanabe M, Takeda S, Ikeuchi H (1979) Atlas of arthroscopy, 3rd edn. Igaku-shoin, Tokyo
Yoo WJ, Jang WY, Park MS, Chung CY, Cheon JE, Cho TJ, Choi IH (2015) Arthroscopic treatment for symptomatic discoid meniscus in children: midterm outcomes and prognostic factors. Arthroscopy 31:2327–2334
Young RB (1889) The external semilunar cartilage as a complete disc. In: Cleland J, Mackay JY, Young RB (eds) Memoirs and memoranda in anatomy. Williams and Norgate, London, p 179
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
The appropriate institutional review board of Hoshigaoka Medical Center for human subject research approved this study (ID: 1603).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Matsuo, T., Kinugasa, K., Sakata, K. et al. Post-operative deformation and extrusion of the discoid lateral meniscus following a partial meniscectomy with repair. Knee Surg Sports Traumatol Arthrosc 25, 390–396 (2017). https://doi.org/10.1007/s00167-016-4393-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4393-6