Abstract
Purpose and hypothesis
Improvements in pain, function and sports activity are the main goals of patients following total knee arthroplasty (TKA). Participation in sports has become an increasingly important contributor to patients’ quality of life (QoL). Hiking is one of the most popular summer activities among elderly people in alpine regions. Consequently, this randomized controlled trial investigates the impact of a 3-month guided hiking programme on patients’ functional abilities and QoL following TKA. It was hypothesized that patients who participate in this programme would demonstrate improvements in functional and QoL parameters compared with a control group.
Methods
Forty-eight TKA patients were included and randomized into either the intervention group (IG; n = 25) or the control group (CG; n = 23). The IG participated in a 3-month hiking programme (2–3 times a week), whereas the CG performed activities of daily living. The stair climb test (SCT), QoL questionnaires and isokinetic force measurements were completed at three time points (i.e. pre-test, post-test, retention-test). ANOVAs for repeated measurements were conducted for the SCT results. The Friedman test and the Mann–Whitney U test were performed for the QoL parameters.
Results
After the 3-month hiking programme, the IG achieved faster overall walking times on the SCT. The time decreased from 4.3 ± 0.6 s (pre-test) to 3.6 ± 0.4 s (post-test) for the stair ascent (p = 0.060) and from 3.6 ± 0.6 s (pre-test) to 3.2 ± 0.5 s (post-test) for the stair descent (p = 0.036). The IG showed significant improvement on some of the subscales of the Knee Injury and Osteoarthritis Outcome Score from pre-test to retention-test (p < 0.01). In the CG, no significant changes were observed (n.s.).
Conclusions
The results indicate moderate improvement in the functional abilities and QoL of TKA patients who participated in a 3-month guided hiking programme compared with the patients in the CG. Hiking did not have any acute detrimental effects on the TKA patients during this study period.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the 1980s, pain relief was the main goal for patients electing to undergo TKA, followed by improved knee function. Today, improvements in health-related quality of life (HRQoL) [13, 20] and a return to desired activities play an increasing role [3, 42, 46] in the decision to undergo surgery. Basically, younger patients are more physically active than elderly patients, and a return to an active life and to sports plays an important role [12, 16, 42]. However, the most common outcome measurements following TKA are still clinical and physical examinations and radiographs. It has been suggested that patient-reported outcomes be considered the most important primary outcome in clinical trials [40].
To date, a considerable amount of literature has been published on quality of life (QoL) outcomes for patients following TKA comparing pre-operative to post-operative QoL [8, 14, 32, 33]. For many patients, sports participation is closely related to their QoL. While increased sports participation following TKA is a concern for many surgeons in terms of polyethylene wear and early loosening [11, 15, 24, 41], patients’ desire to return to a certain sports activity has become an important factor in the decision to undergo TKA.
A highly debated question is whether participating in sports after a TKA is safe and in addition has positive effects. Previous studies have reported that sports activity leads to wear and loosening of the implant [11, 15, 24, 41]. This is in contrast to other studies showing that adjusted physical activity reduces wear and loosening [18, 20, 27, 30, 31, 43]. Previous studies have reported that patients with a TKA regularly participate in sports and have shown that skiing has a positive effect on patients with TKA [28, 34].
Despite these facts, there are only limited data on the various effects of sports participation among patients with a TKA. A study of Korean patients with TKAs verified that regular physical activity was associated with greater patient satisfaction [10]. More recently, an intervention study on the impact of alpine skiing [2, 21, 34] on patients following TKAs was published. This 12-week intervention study documented a positive influence of alpine skiing on a variety of important aspects for TKA patients, such as improvements in activities of daily living (ADL), QoL and well-being in the intervention group [35, 47].
While alpine skiing is a common winter sport in alpine regions, hiking is the most common summer activity and is especially desirable for the elderly. A significant number of patients with TKA participate in sports with a high knee load such as alpine skiing and mountain hiking [28]. The knee joint is loaded with eight times body weight when going downhill. There are recommendations that patients following TKA should use skipoles and walk slowly when descending to reduce the load on the knee joint [22, 23]. However, the impact of hiking or mountaineering on the implants of TKA patients is not yet clear. The existing recommendations are more often based on experience rather than on research [16, 29, 42].
Thus, to our knowledge this is the first study of the effects of hiking on patients with TKAs. Our hypothesis is that TKA patients who participate in a 3-month controlled hiking programme will demonstrate improvements in functional abilities and QoL criteria compared with a control group of TKA patients.
Materials and methods
This present study was a randomized, controlled, monocentric study of patients following TKA (EudraCT: 2015-001451-80). The study was conducted between July and December 2015. The study was approved by the ethics committee of Medical University Innsbruck (AN2015-0080).
Patients with knee osteoarthritis who underwent primary TKA were considered for recruitment. First, the subjects were examined to determine whether they met the inclusion criteria. Patients (55–75 years old) with a TKA met the inclusion criteria if they were 1–5 years post-operative, committed to hiking 2–3 times a week over a 3-month period and willing to participate. Additionally, written informed consent and medical approval from the study physicians were required for inclusion. Exclusion criteria were a painful contralateral knee, acute illnesses or injuries prior to or during the study, injuries that could affect the study results, and chronic diseases for which hiking is a contraindication. The patients were randomized into either the intervention group (IG) or the control group (CG) using block randomization. The study coordinator was responsible for allocating the patients to either the IG or the CG. The IG had a full medical check with routine laboratory analyses, spirometry and ECG at rest and an incremental cycle ergometry until exhaustion.
Over a 3-month period, the patients in the IG participated in a guided hiking programme, while those in the CG continued their ADLs. The CG was not allowed to go hiking during this time. The IG hiked 2–3 times a week (25 days total) with a certified hiking guide. The IG was allowed to be absent two times and participated on average 23.6 days. An average hiking tour consisted of a vertical distance of about 400 m, 7 km walking distance and took 3.5 h. The hiking tours took place in the area Innsbruck and surroundings between an altitude of 563 and 2148 m above sea level. The hiking paths were well established, including gravel paths and forest tracks. The ascent was moderate steep, and an adjusted descent was chosen, considering slippery terrain. The mean altitude of the hikes was 9870 m for ascent and 9870 m for descent, and the mean distance was 194 km. All of the patients used hiking poles. The hiking speed was self-selected by the patients. All patients measured their heart rate (HR) during the hike with a HR watch. The average HR during the hikes was on average 55–65 % of the maximum HR, which was based on the ergometry data.
All of the subjects underwent a thorough examination prior to the intervention period (pre-test), immediately after the 3-month intervention period (post-test) and 2 months after (retention-test). The IG received radiographs and a clinical examination prior to and after the intervention, and the Knee Society Clinical Rating Score (KSS) was used for clinical scoring. The KSS consists of two parts (knee joint and functional score), but we only used the total KSS in this study [19].
The primary objective was to demonstrate whether functional abilities, as measured with the SCT, were superior in the IG compared with the CG. The secondary objective was to evaluate whether the patient-reported outcomes of the IG were superior to those of the CG. Additional outcomes were to compare the objective functional parameters with the subjective functional parameters and to illustrate the isokinetic force measurements of the subjects with one TKA.
The SCT, the isokinetic measurements and the QoL questionnaires were completed at the pre-test, post-test and retention-test.
The functional parameter was measured with the SCT [6, 9], with stair ascent and stair descent measured separately. The SCT showed high test–retest reliability (r = 0.87) [36] and good interrater reliability (intraclass correlation (ICC) 0.94, 95 % confidence interval (CI) of 0.55–0.98) in patients following TKA [1]. The stair ascent test started at the bottom of the stairs, and the patients were asked to walk as quickly and as safely as possible. For the stair descent, the patients began at the top of 10 steps (height 17 cm, depth 28 cm). The test instruction was to walk safely. The time it took to ascend and descend a flight of stairs was recorded with a stopwatch, starting from the time that the subject raised his/her foot off of the first step to the time that the subject placed both feet on the ground. All of the patients were allowed to practise first. The same stairs were used for the pre-test, post-test and retention-test. The tester remained at the starting position until the participant completed the test. All of the participants were able to complete the SCT. Two subjects in the IG preferred to use a handrail for safety reasons as they completed the stair descent test (pre-test).
The patient-reported outcome was measured with different types of questionnaires. To address the secondary objective, the Knee Injury and Osteoarthritis Outcome Score (KOOS) was used. The KOOS consists of five subscales, including pain, symptoms, function in daily living (ADL), function in sport and recreation (Sport/Rec) and knee-related QoL. The possible scores for each subscale range from 0 (extreme knee problems) to 100 (no knee problems) [37–40]. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [4, 5] is included in the KOOS questionnaire [39] and consists of the pain, stiffness and function subscales. Additionally, all of the subjects completed the Short Form (SF)-36 [7, 44, 45]. All of the questionnaires were completely filled out (i.e. there were no missing values).
An isokinetic dynamometer (Con-Trex® MJ, CMV AG, Zurich, Switzerland) was used to measure the extensor and flexor torque. All of the subjects completed a warm-up that consisted of 10 min of cycling on a stationary ergometer with a cadence of 60–80 rpm. The non-operated knee was tested first. The test consisted of a 90-s warm-up on the Con-Trex, during which the patients were asked to follow the movement and increase their force slowly. Afterwards, the patients had 30 s to rest. The testing was performed at 60°/s with the quadriceps and hamstring in concentric contraction. Each participant performed four consecutive repetitions without a pause between repetitions [26]. The participants were instructed to push as forcefully as possible without invoking pain. Afterwards, the contralateral leg was tested.
Statistical analysis
For the statistical analysis, IBM® SPSS® Statistics 23 (SPSS, Armonk, NY, USA) was used. A power calculation was performed with G*Power 3.1. A total of 20 subjects in each group was needed to provide 95 % power to detect the primary objective with an expected difference between IG and CG of 1.0 ± 0.84 s, assuming a two-sided alpha error of 0.05 [34]. To account for possible dropouts, the study team aimed to recruit a total of 50 subjects. The mean and standard deviation were calculated for descriptive statistics and were used for statistical comparison. The Kolmogorov–Smirnov-test was performed to test for normal distribution. ANOVAs for repeated measurements were performed to assess the differences between and within groups. The analyses were conducted for the stair ascent and stair descent. The primary hypothesis was tested with a two-sided significance level of 0.05. All of the QoL scores did not follow a normal distribution. To analyse the patient-reported outcomes (measured with the KOOS, WOMAC and SF-36), the Friedman test and the Mann–Whitney U test were performed. To correct for multiple comparison, we used a Bonferroni correction (QoL: p < 0.01; SCT: p < 0.025 was considered statistically significant). To show an association between the objective (SCT) and subjective (KOOS ADL subscale) functional parameters, Spearman’s rank correlation was used. A subgroup analysis of isokinetic force in patients with one TKA (IG: n = 14; CG: n = 18) was performed.
Results
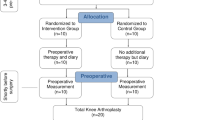
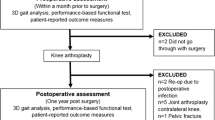
A total of forty-eight patients were enrolled (IG: n = 25, CG: n = 23), of which two did not complete the study. Thus, forty-six patients completed the study (Fig. 1). In both groups, approximately 60 % of the subjects were female, and the average age was 67 years. Regarding the patients’ demographics at baseline, no statistically significant differences between the groups were detectable (Table 1).
Primary outcomes
The mean walking times for stair ascent and stair descent are shown in Table 2. For the stair ascent, subjects in the IG reduced their measured time from 4.3 ± 0.6 s at the pre-test to 3.6 ± 0.4 s at the post-test, whereas in the CG the measured time increased from 4.2 ± 0.9 s at the pre-test to 4.3 ± 0.9 s at the post-test. For the stair ascent, the group difference was not significant (n.s.). However, there was a strong significant interaction between time and group, suggesting improvement in the IG compared with no improvement in the CG. For the stair descent, only the time effect was significant due to the Bonferroni correction (Table 2).
Secondary outcomes
The KOOS profiles are shown in Fig. 2. Although QoL data were not normal distributed, mean and median values were similar, and therefore only mean and standard deviation were reported. The IG showed significant improvement from pre-test to retention-test in three subscales of the KOOS (p < 0.01), whereas the CG showed no significant changes (n.s.). However, direct comparison between IG and CG at post-test and retention-test did not show any statistically significant differences (n.s.) (Table 3).
The descriptive statistics for the transformed WOMAC are shown in Table 4. No significant changes (n.s.) between and within groups were observed in both groups after Bonferroni correction (Table 4).
No statistically significant (n.s.) changes for any of the SF-36 subscales were observed for either group at the pre-test, post-test or retention-test.
Clinical outcome
No acute detrimental effects (such as swelling or increased pain) occurred within the study period. Radiographs did not document any signs of loosening or increased wear. In the IG, the KSS increased significantly from 93.8 ± 4.7 at the pre-test to 96.6 ± 2.6 at the post-test (p = 0.002), in contrast with the pre-test (93.4 ± 4.4) and post-test (93.3 ± 4.3) results for the CG (p = 0.732). The body mass index (BMI) did not change within the study period.
Additional outcomes
The correlations between the SCT and the ADL subscale of the KOOS at the pre-test, post-test and retention-test were calculated. A statistically significant correlation was only found for the CG at the pre-test (r = −0.447) and the retention-test (r = −0.460). For the IG, the mean KOOS ADL increased from 86.5 ± 13.5 at pre-test to 92.3 ± 9.7 at post-test. For the CG, the mean KOOS ADL was almost consistent (94.3 ± 4.7 at pre-test; 94.9 ± 5.0 at post-test) (Table 3).
The subgroup analysis (of patients with only one TKA) of isokinetic force measurement showed that there was no significant difference between the IG and the CG. Additionally, no significant extensor torque difference between the operated and unoperated leg occurred. However, a strong time effect occurred (p < 0.001). A significant time effect was shown for the flexor torque (p = 0.006) and for the extensor–flexor torque ratio (p = 0.028).
Discussion
The most important finding of the present study was that patients with a TKA who hiked regularly for a period of 3 months showed moderate improvements in functional abilities, as measured with the SCT, compared with patients who only performed ADLs.
A recent study aimed to examine the effect of a 12-week recreational skiing intervention on functional gait performance in patients following unilateral TKA. Twenty-three patients (IG: n = 10; CG: n = 13) completed the SCT and the timed up-and-go test [34]. That study showed stair descent test results that were similar to ours. Pötzelsberger et al. found a reduced walking time in the IG only for the stair descent test from pre-test to post-test, while there was no change in the CG. This result is consistent with our data for the stair descent test. Additionally, the IG of the present study showed statistically significant improvements in walking times for the stair ascent test. This effect was likely the result of the hiking intervention; the patients in the IG were used to such efforts as they had practised ascents for 3 months while hiking.
Another important finding was that the TKA patients who hiked regularly showed a moderately improved QoL. We found an enhancement in the QoL of the TKA patients who participated in the 3-month guided hiking programme compared with the QoL of the patients who only performed ADLs. The patients in the IG showed significant improvements in their scores from pre-test to retention-test on three subscales of the KOOS. In the CG, no significant changes were observed. This might be because the CG achieved better QoL scores than the IG at pre-test and post-test. This fact could lead to a ceiling effect. Nevertheless, the result shows that regular hiking had a positive effect on the patient-reported outcome, as measured with the KOOS. The SF-36 showed no statistically significant changes in any of the subscales for both groups. A possible explanation might be that this questionnaire addresses QoL in general and is not disease related, unlike the KOOS [39].
A few studies have compared the pre-operative QoL to the post-operative QoL of patients following TKA [8, 14, 32, 33]. Most of these studies compare the pre- and post-operative status of patients who have undergone TKA. Núñez et al. [33], for example, demonstrated that post-operative patients show significant improvements on all three subscales of the WOMAC compared with pre-operative patients. Gandhi et al. found similar results regarding the WOMAC; additionally, they investigated the change in the SF-36 scores. The physical functioning and role physical subscale scores improved significantly from pre-operation to 1 year post-operation [14]. In a prospective study, Nilsdotter et al. [32] reported improvements on all of the subscales of the KOOS at 6 months post-operation compared with the pre-operative scores. One study showed KOOS results separated by 5 years that were comparable with the present results, except for the Sport/Rec subscale [32]. Compared with the results of Bruyère et al., the results of the present study show similar scores for the WOMAC pain and stiffness subscales. We observed significant differences in the function subscale, in contrast with the study of Bruyère (Bruyère: 14.4 vs. present study: 6.6) [8]. This difference might have occurred because the patients in our study were generally very physically active and not only maintained but increased their sports activity following TKA surgery [17].
A 12-week skiing intervention study showed the positive influence of skiing on well-being in the IG [47]. The present study found that the 3-month hiking intervention also had a positive impact. However, different QoL questionnaires were used; therefore, it is difficult to compare the results of the skiing study with our results.
The present study showed that hiking has a positive impact on the functional abilities of TKA patients. People who had undergone TKA and regularly went hiking were able to climb stairs more quickly, and because of the hiking, they felt more confident and safe while climbing stairs and during ADLs. Therefore, hiking also affects everyday activities; for example, climbing the stairs with grocery bags is easier for people with a TKA who hike regularly. The results of the present study can also be used to support physicians in their decision making. The KSS increased significantly in the IG, even if it is less than the minimal clinical important difference identified by Lee [25]. The clinical examination prior to and after the intervention showed no detrimental effects on short-term clinical outcomes with respect to radiographic changes.
Moreover, regular hiking by TKA patients led to improved QoL, as measured with the KOOS questionnaire. This result indicates that the benefits of hiking extend to daily life activities, such as doing housework, putting on socks or getting into a car. Patients should be informed of the positive effect of regular hiking on everyday life. Hiking is “allowed with experience”, according to the 1999 recommendations from the Knee Society; however, this recommendation is based on surgeons’ experience and not on evidence-based research [29, 42]. The present study provides evidence that supports the recommendation of the Knee Society.
One limitation of the study concerns the measurement tool used during the SCT. According to the literature, a stopwatch is appropriate for recording time, but it yields measurements that are less accurate than, for example, a light barrier. The utilisation of another functional test would have been helpful to support and verify the results of the SCT. Despite randomization there is the risk for selection and ascertainment bias. Another limitation is that this study did not include a third group that met regularly to spend time together doing social activities, such as playing cards or playing chess. The psychological effect of group activities on the IG patients may have been underestimated. Thus, further research is needed to verify that the impacts measured in this study are the result of hiking and not the psychological effect of social activities. A follow-up is planned 1 year after the end of the study to investigate the effects on functional abilities, QoL and clinical outcomes.
Conclusions
The group that completed the 3-month hiking programme showed moderate improvement in functional parameters and QoL. Therefore, it can be concluded that patients who have undergone TKA should be encouraged to hike to improve their daily lives.
References
Almeida GJ, Schroeder CA, Gil AB, Fitzgerald GK, Piva SR (2010) Interrater reliability and validity of the stair ascend/descend test in subjects with total knee arthroplasty. Arch Phys Med 91:932–938
Amesberger G, Müller E, Würth S (2015) Alpine skiing with total knee arthroplasty (ASWAP): physical self-concept, pain, and life satisfaction. Scand J Med Sci Sports 25:82–89
Bauman S, Williams D, Petruccelli D, Elliott W, de Beer J (2007) Physical activity after total joint replacement: a cross-sectional survey. Clin J Sport Med 17:104–108
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Bellamy N, Campbell J, Stevens J, Pilch L, Stewart C, Mahmood Z (1997) Validation study of a computerized version of the Western Ontario and McMaster Universities VA3.0 Osteoarthritis index. J Rheumatol 24:2413–2415
Bennell K, Dobson F, Hinman R (2011) Measures of physical performance assessments: self-paced walk test (SPWT), stair climb test (SCT), 6-m walk test (6MWT), chair stand test (CST), timed up & go (TUG), sock test, lift and carry test (LCT), and car task. Arthritis Care Res (Hoboken) 63:350–370
Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, Westlake L (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305:160–164
Bruyère O, Ethgen O, Neuprez A, Zègels B, Gillet P, Huskin JP, Reginster JY (2012) Health-related quality of life after total knee or hip replacement for osteoarthritis: a 7-year prospective study. Arch Orthop Trauma Surg 132:1583–1587
Butler AA, Menant JC, Tiedemann AC, Lord SR (2009) Age and gender differences in seven tests of functional mobility. J Neuroeng Rehabil 6:31
Chang M, Kim S, Kang Y, Chang C, Kim T (2014) Activity levels and participation in physical activities by Korean patients following total knee arthroplasty. BMC Musculoskelet Disord 15:240
Chen L, Tan Y, Al-Aidaros M, Wang H, Wang X, Cai S (2013) Comparison of functional performance after total knee arthroplasty using rotating platform and fixed-bearing prostheses with or without patellar resurfacing. Orthop Surg 5:112–117
Dahm DL, Barnes SA, Harrington JR, Sayeed SA, Berry DJ (2008) Patient-reported activity level after total knee arthroplasty. J Arthroplasty 23:401–407
Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY (2004) Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg Am 86:963–974
Gandhi R, Dhotar H, Razak F, Tso P, Davey JR, Mahomed NN (2010) Predicting the longer term outcomes of total knee arthroplasty. Knee 17:15–18
Hamai S, Miura H, Higaki H, Shimoto T, Matsuda S, Okazaki K, Iwamoto Y (2008) Three-dimensional knee joint kinematics during golf swing and stationary cycling after total knee arthroplasty. J Orthop Res 26:1556–1561
Healy WL, Sharma S, Schwartz B, Iorio R (2008) Athletic activity after total joint arthroplasty. J Bone Joint Surg Am 90:2245–2252
Hepperger C, Abermann E, Herbst E, Hoser C, Gföller P, Fink C (2016) Free papers. Knee Surg Sports Traumatol Arthrosc 24(Suppl 1):S4–S114
Hofstaedter T, Fink C, Dorn U, Pötzelsberger B, Hepperger C, Gordon K, Müller E (2015) Alpine skiing with total knee arthroplasty (ASWAP): clinical and radiographic outcomes. Scand J Med Sci Sports 25:10–15
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Jones DL, Cauley JA, Kriska AM, Wisniewski SR, Irrgang JJ, Heck DA, Kwoh CK, Crossett LS (2004) Physical activity and risk of revision total knee arthroplasty in individuals with knee osteoarthritis: a matched case–control study. J Rheumatol 31:1384–1390
Kösters A, Pötzelsberger B, Dela F, Dorn U, Hofstaedter T, Fink C, Müller E (2015) Alpine skiing with total knee arthroplasty (ASWAP): study design and intervention. Scand J Med Sci Sports 25:3–9
Kuster MS, Grob K, Gachter A (2000) Problems of total knee replacement from a sports orthopedics point of view. Orthopade 29:739–745
Kuster MS, Grob K, Gachter A (2000) Knee endoprosthesis: sports orthopedics possibilities and limitations. Orthopade 29:739–745
Lavernia CJ, Sierra RJ, Hungerford DS, Krackow K (2001) Activity level and wear in total knee arthroplasty: a study of autopsy retrieved specimens. J Arthroplasty 16:446–453
Lee WC, Kwan YH, Chong HC, Yeo SJ (2016) The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4208-9
Liebensteiner MC, Krismer M, Koller A, Semenitz B, Mayr E (2012) Does minimally invasive total knee arthroplasty improve isokinetic torque? Clin Orthop Relat Res 470:3233–3239
Marques EA, Mota J, Carvalho J (2012) Exercise effects on bone mineral density in older adults: a meta-analysis of randomized controlled trials. Age (Dordr) 34:1493–1515
Mayr HO, Reinhold M, Bernstein A, Suedkamp NP, Stoehr A (2015) Sports activity following total knee arthroplasty in patients older than 60 years. J Arthroplasty 30:46–49
McGrory BJ, Stuart MJ, Sim FH (1995) Participation in sports after hip and knee arthroplasty: review of literature and survey of surgeon preferences. Mayo Clin Proc 70:342–348
Mont MA, Marker DR, Seyler TM, Gordon N, Hungerford DS, Jones LC (2007) Knee arthroplasties have similar results in high- and low-activity patients. Clin Orthop Relat Res 460:165–173
Mont MA, Marker DR, Seyler TM, Jones LC, Kolisek FR, Hungerford DS (2008) High-impact sports after total knee arthroplasty. J Arthroplasty 23(Suppl1):80–84
Nilsdotter A, Toksvig-Larsen S, Roos EM, Nilsdotteryz A, Rooszx EM (2009) A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthr Cartil 17:601–606
Núñez M, Núñez E, Luis del Val J, Ortega R, Segur JM, Hernández MV, Lozano L, Sastre S, Maculé F (2007) Health-related quality of life in patients with osteoarthritis after total knee replacement: factors influencing outcomes at 36 months of follow-up. Osteoarthr Cartil 15:1001–1007
Pötzelsberger B, Lindinger SJ, Stöggl T, Buchecker M, Müller E (2015) Alpine skiing with total knee arthroplasty (ASWAP): effects on gait asymmetries. Scand J Med Sci Sports 25:49–59
Pötzelsberger B, Stöggl T, Lindinger SJ, Dirnberger J, Stadlmann M, Buchecker M, Hofstaedter T, Gordon K, Müller E (2015) Alpine skiing with total knee arthroplasty (ASWAP): effects on strength and cardiorespiratory fitness. Scand J Med Sci Sports 25:16–25
Rejeski WJ, Ettinger WH, Schumaker S, James P, Burns R, Elam JT (1995) Assessing performance-related disability in patients with knee osteoarthritis. Osteoarthr Cartil 3:157–167
Roos EM, Lohmander LS (2003) The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64
Roos EM, Roos HP, Ekdahl C, Lohmander LS (1998) Knee injury and Osteoarthritis Outcome Score (KOOS)—validation of a Swedish version. Scand J Med Sci Sports 8:439–448
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther 28:88–96
Roos EM, Toksvig-Larsen S (2003) Knee injury and Osteoarthritis Outcome Score (KOOS)—validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1:17
Schmalzried TP, Szuszczewicz ES, Northfield MR, Akizuki KH, Frankel RE, Belcher G, Amstutz HC (1998) Quantitative assessment of walking activity after total hip or knee replacement. J Bone Joint Surg Am 80:54–59
Swanson EA, Schmalzried TP, Dorey FJ (2009) Activity recommendations after total hip and knee arthroplasty: a survey of the American Association for Hip and Knee Surgeons. J Arthroplasty 24:120–126
Vogel LA, Carotenuto G, Basti JJ, Levine WN (2011) Physical activity after total joint arthroplasty. Sports Health 3:441–450
Ware JE, Gandek B (1998) Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol 51:903–912
Ware JE, Sherbourne CD (1992) The MOS 36-ltem Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care 30:473–483
Weiss JM, Noble PC, Conditt MA, Kohl HW, Roberts S, Cook KF, Gordon MJ, Mathis KB (2002) What functional activities are important to patients with knee replacements? Clin Orthop Relat Res 404:172–188
Würth S, Finkenzeller T, Pötzelsberger B, Müller E, Amesberger G (2015) Alpine skiing with total knee arthroplasty (ASWAP): physical activity, knee function, pain, exertion, and well-being. Scand J Med Sci Sports 25:74–81
Acknowledgments
The study group would like to thank all of the study participants for their efforts.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest related to this study.
Funding
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Hepperger, C., Gföller, P., Hoser, C. et al. The effects of a 3-month controlled hiking programme on the functional abilities of patients following total knee arthroplasty: a prospective, randomized trial. Knee Surg Sports Traumatol Arthrosc 25, 3387–3395 (2017). https://doi.org/10.1007/s00167-016-4299-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4299-3