Abstract
Purpose
Anterior cruciate ligament (ACL) injury is associated with a pathologic gait pattern and increased energy cost during locomotion. ACL reconstruction could improve the gait pattern. Hamstrings tendon (HAM) and bone–patellar tendon–bone (BPTB) grafts are usually used for reconstruction. The aim of this study was to compare the efficacy of anatomic ACL reconstruction with HAM and BPTB grafts on improving and normalizing the energy cost and physiologic reserves during flat, uphill, and downhill walking.
Methods
Twenty male subjects with unilateral ACL injuries were randomly assigned to ACL reconstruction with a HAM (n = 10) or BPTB (n = 10) graft. Ten matched controls were also enrolled. All participants performed three 8-min walking tasks at 0, +10, and −10 % gradients before and 9 months after surgery. Energy cost (oxygen consumption, VO2), heart rate (HR), and ventilation (VE) were measured. Lysholm/IKDC scores were recorded.
Results
Pre-operatively, VO2, HR, and VE were higher in the HAM and BPTB groups than in controls during walking at 0, +10, and −10 % gradients (p < 0.001–0.01). Post-operatively, both HAM and BPTB groups showed reduced VO2, HR, and VE during the three walking tasks (p < 0.001–0.01). Although the post-operative VO2 in both surgical groups reached 90–95 % of the normative (control) value during walking, it remained elevated against the value observed in controls (p < 0.001–0.01). The HAM and BPTB groups showed no differences in post-surgical VO2 or HR during walking at all three gradients.
Conclusion
Anatomic ACL reconstruction with either HAM or BPTB graft resulted in similar short-term improvements in energy cost and nearly normalized locomotion economy and cardiorespiratory reserves during flat, uphill, and downhill walking. The improved locomotion economy is an additional benefit of anatomic ACL reconstruction, irrespective of the type of graft used, that the orthopaedic surgeons should consider.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
ACL insufficiency results in joint instability, increases the load on knee compartments during anterior and rotational joint loading [39], and alters the electromyographic profile [27] and gait kinematics [3, 25]. Because ACL rupture, unlike other ligament injuries, does not heal, the orthopaedic society has largely adopted surgical treatment to correct the ACL deficiency [9].
ACL reconstruction improves knee kinematics [6, 12, 38, 43], reverses abnormal anteroposterior laxity [15, 37, 41], and prevents further damage to other knee structures [21, 39, 48]. Currently, the most widely used grafts for anatomic ACL reconstruction are bone–patellar tendon–bone and hamstring tendon auto grafts [32]. It has been shown that changes in biomechanics of the knee joint after ACL reconstruction are graft specific and are related to the donor site [47]. It has also been reported that the two grafts have advantages and disadvantages, but neither has been qualified as clearly superior [35].
Apart from the adverse effects on joint laxity and kinematics, ACL deficiency may also decrease metabolic economy (i.e. increase energy demands) during locomotion [22, 30]. It has been suggested that ACL-deficient patients increase their muscle contractions (thereby increasing the energy cost) in an effort to avoid abnormal anterolateral rotatory laxity during locomotion [20, 28]. It is therefore conceivable that the disappearance of joint laxity and the restoration of kinematics after surgery might improve, or even normalize, the energy cost during locomotion. Indeed, the only study that investigated the impact of ACL reconstruction on walking economy reported that patients with reconstructed ACLs (using the hamstring tendon auto graft) exhibited improved energy cost during walking [4]. Colak et al., however, examined the energy demand only during flat walking using a “within-subject” design. Thus, the impact of ACL reconstruction on energy cost during more demanding tasks of daily living (e.g. ascending and descending stairs), which might unmask various aspects of ACL reconstruction outcomes (e.g. functional), is not known. There is evidence that although ACL reconstruction nearly restores gait patterns during level walking, the asymmetric gait pattern persists for ascending and descending walking [18]. Furthermore, it is not clear whether patients with reconstructed ACL normalize their energy cost to levels observed in those with healthy ACL. Most important, however, is that the efficacy of ACL reconstruction using the bone–patellar tendon–bone (BPTB) graft for reducing the energy cost during locomotion, and how it compares with the efficacy of using a hamstring tendon graft, have yet to be examined. This is despite the knowledge that different types of tendon graft contribute uniquely to gait mechanics and knee laxity and even lead to different gait patterns [26, 47].
Reduced energy demand during locomotion may increase the physiologic reserves of the body and the individual’s tolerance to daily tasks and exercise, thereby reducing the risk of musculoskeletal injury. Hence, knowledge regarding improvements in energy cost in patients with reconstructed ACL following hamstring tendon and BPTB grafts could be important for sports medicine practitioners. It could help them establish safe and effective rehabilitation protocols, thereby avoiding the undesirable musculoskeletal conditions associated with increased physiologic effort and fatigue.
The current study included two novel elements: (1) The effect of ACL reconstruction on improving and normalizing the energy cost was assessed during flat, uphill, and downhill walking and (2) the effect of hamstring and BPTB grafts was compared on improving the energy cost of locomotion at three gradients after ACL reconstruction.
Materials and methods
Twenty male patients with unilateral ACL rupture and ten healthy controls participated in the study. The participants with ACL injury were recruited from the sports injury outpatient clinic of our hospital. The inclusion criterion was an ACL rupture, proven both clinically and by radiologic evaluation. The exclusion criteria included more complex knee joint injuries (i.e. meniscal tears, other knee ligament ruptures) and active infection. Patients with cardiovascular, pulmonary, or other orthopaedic, systemic, or metabolic diseases were also excluded. Female patients were not included in the study because of known effects of the menstrual cycle on energy cost [40]. All participants were active athletes, participating three to six times per week in sporting activities before the injury. In addition, their ACL injury was sport related. All participants signed a written informed consent and completed a health history questionnaire prior to their participation in the study.
Surgical protocols
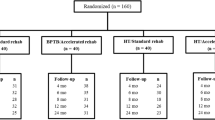
The patients with ACL injuries were randomly and equally divided into two groups according to the type of graft used for the ACL reconstruction: Hamstrings group (n = 10) and BPTB group (n = 10). Randomization was generated using a computer-based program. The order of walking tasks for each patient was specified by creating random permutations of treatments for situations in which subjects have to undergo the treatments in random order. A control group matched for physical characteristics and physical activity was included in the study (Table 1). The participants in the “Hamstring” group underwent arthroscopically guided, single-bundle, anatomic ACL reconstruction using a hamstring tendon autograft. Endobutton was used for femoral fixation and an interference screw for tibial fixation (ConMed Linvatec, Largo, FL, USA). The BPTB group underwent arthroscopically guided, single-bundle, anatomic ACL reconstruction using a BPTB autograft. An interference screw was used for both femoral and tibial fixation (ConMed Linvatec). All patients with reconstructed ACLs participated in the same post-operative conventional rehabilitation program. Six months after the operation, the patients were allowed to return gradually to their sporting activities.
Patient’s evaluation
Standardized clinical and radiologic evaluations were performed on all patients prior to inclusion in the study. The clinical evaluation was carried out by an experienced blinded examiner in the outpatient clinic just prior to starting the walking tasks, both before and after ACL reconstruction. The evaluation included Lachman’s test, lateral pivot shift test, and anterior drawer test. Participants were also evaluated with the Lysholm Knee Scoring Scale [42] and the International Knee Documentation Committee (IKDC) subjective knee evaluation score [17] (Table 2). The injured knee underwent magnetic resonance imaging to confirm the ACL tear and to exclude any other knee injuries.
Measurement of energy cost
The energy cost of walking was measured in all participants prior to and 9 months after ACL reconstruction. All tests to assess energy cost were performed at the hospital at the same time of day (± 1 h) and in similar atmospheric conditions (temperature 22–23° C; relative humidity 40–50 %). The participants were instructed to abstain from caffeinated drinks and tobacco products 12 h prior to testing, from alcohol consumption for at least 24 h before testing, and from any exercise for 48 h prior to testing.
Upon arrival at the laboratory, height and body mass were measured using a stadiometer to the closest 0.1 kg and a weighing scale to the nearest 0.1 cm (Seca, Hamburg, Germany). Next, the participants performed three 8-min walking tasks on a motorized treadmill (Leisure Works; Maurice Pincoffs, ON, Canada) with a 10-min rest interval. The three walking tasks were performed in a randomized order at 5 km/h at flat (0 %), uphill (+10 %), and downhill (−10 %) gradients. This speed was selected because it is within the adult functional range of walking speeds [45] and is associated with the lowest walking metabolic cost for men [5, 23]. The K4b2 metabolic system (Cosmed, Rome, Italy) was used to collect (breath-by-breath) and analyse the respiratory gas samples. The measurement accuracies of the flow meter and O2 and CO2 analysers of this device are ± 2, ± 0.02 and ± 0.01 %, respectively [7, 36]. A high test–retest reliability has been reported for this device during submaximal and maximal exercises (intraclass coefficient = 0.85–0.96) (ICC = 0.85–0.96) [7, 8, 31]. Following the manufacturer’s guidelines, we performed room air and reference gas calibrations of the O2 and CO2 analysers (16 and 5 %, respectively) as well as turbine calibrations prior to and after each test.
The participant’s heart rate was continuously recorded using chest belt telemetry (Polar Electro, Kempele, Finland). The respiratory data from each walking task were averaged over the last 3 min (steady-state metabolic condition) and analysed for oxygen consumption (VO2, mL/kg/min), ventilation (VE, L/min), and the respiratory exchange ratio.
The Ethics Committee of Aristotle University of Thessaloniki, Greece, approved this study (ID No. 65/18.02.2014).
Statistical analysis
All data are presented as mean ± SD and were analysed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). Shapiro–Wilk tests were used to examine whether the data were normally distributed. Two-way analysis of variance (three groups × two time points) with repeated measures on “time” (before and after surgery) was used to determine the main effects and interaction effects on dependent variables. Newman–Keuls post hoc tests were used to identify the significantly different means. The level of statistical significance was set at p = 0.05. A prospective power analysis was performed for our main variable (VO2) for estimating sample size. Based on the results of our previous study [22], a standard deviation of 2 mL∙kg−1∙min−1 (10–15 %) with an effect of at least 2.8 mL∙kg−1∙min−1 (20 %) was expected. The calculation indicated that at least nine subjects per group were needed to identify statistical significance at an alpha of 0.05 with a power of 0.80.
Results
Figure 1 and Table 3 present the mean ± SD for VO2, heart rate (HR), ventilation (VE), and respiratory exchange ratio for the surgical groups before and after surgery and for controls. The analyses of variance revealed a significant “group × time” interaction effect on VO2, HR, and VE (p < 0.001–0.01) for all three walking gradients. For the respiratory exchange ratio, only the main effect of “time” (before vs. after surgery) was significant (p < 0.001–0.05).
Pairwise comparisons on pre-operative values revealed that VO2, HR, and VE were significantly higher in the two graft groups than in the controls during walking at 0, +10, and −10 % gradients (p < 0.001–0.01). Post hoc comparisons within groups showed that the post-operative VO2, HR, and VE values were significantly lower than the pre-operative values for both graft groups during walking at all three gradients (p < 0.001–0.01). No changes were observed between the pre-operative and post-operative measurements for the above variables in the controls.
When the post-operative means of the groups were compared, the results indicated that HR and VE were not different for the two graft groups versus the control at all walking gradients. The VO2 in the graft groups reached on average 95 % of the normative (control) value for the flat gradient, 90 % for uphill walking, and 91 % for downhill walking; it remained, however, significantly elevated in both graft groups over the control value (p < 0.001–0.01). There were no significant differences between BPTB and hamstrings groups for post-operative VO2 and HR. The post-operative VE, however, was lower in the BPTB group than in the hamstrings group (p < 0.05). Analysis of data using delta scores between pre-operative and post-operative values (to correct for numerical baseline differences) showed no differences between the two experimental groups in the magnitude of reductions for the above variables.
The respiratory exchange ratio decreased post-operatively in both graft groups during flat and uphill walking (p < 0.05), with no differences among the three groups at the pre-operative and post-operative time points for all three walking tasks.
Discussion
The most important findings of the present study were: (1) ACL-deficient patients have impaired energy cost when walking at level, uphill, and downhill gradients compared with individuals with healthy ACLs, (2) ACL reconstruction using either BPTB or hamstrings grafts improved the walking economy of patients with ACL deficiency at three gradients, reaching approximately 92 % of the value observed in individuals with intact ACLs, and (3) BPTB and hamstrings grafts confer similar improvements in walking economy.
Energy cost in ACL-deficient patients
There is a consensus that pathologic gait patterns owing to orthopaedic disabilities—e.g. hip or ankle arthrodesis, flexed-knee gait, amputation, residual leg length, prosthesis (total knee arthroplasty), are linked with higher energy cost [29, 46]. We showed that the energy cost in ACL-deficient patients is higher than that of those with healthy ACL by 19, 25, and 23 % during level, uphill, and downhill walking, respectively. HR and VE were also increased in ACL-deficient patients, by 15 and 11 %, respectively. These findings demonstrate that patients with ACL deficiency work at higher physiologic reserves during locomotion to overcome their abnormal knee laxity.
In support of our findings, another recent study documented a similar reduction in walking efficiency in a different set of ACL-deficient patients [22]. A previous study also demonstrated 8 % decreased economy in patients with ACL deficiency during jogging, but not during flat walking [30]. The increased muscle contraction to overcome abnormal anteroposterior and rotatory laxity in the knee and to stabilize walking [20], as well as reduced strength [3, 30] in ACL-deficient patients has been proposed as potentially contributing factors to the reduced locomotion economy. Recent findings, however, showed that the energy cost is not increased in ACL-deficient limb when exercising in the supine position. This finding suggests that the reduced walking economy of ACL-deficient patients is mostly a result of the altered neuromuscular control (increased contraction of primary and subsidiary muscles) in the lower limb in an effort to increase gait stability [20]. Another possible explanation for the reduced walking efficiency in ACL-deficient individuals is that they adopt a gait pattern for walking that entails significantly less knee extension [14]. Numerous studies have shown that submaximal oxygen consumption increases as stride length is lengthened or shortened from the typically used stride. The reason is that shorter strides increase the internal work of muscles by increasing frequency and reciprocal movements, which results in increased energy cost and decreased locomotion economy [2].
Impact of ACL reconstruction on walking economy
This study is the first to evaluate the extent to which the walking efficiency is normalized following ACL reconstruction. ACL reconstruction restores the normal laxity and kinematics of the knee joint [24]. Thus, it was expected that both grafts used in our study would improve mechanical walking efficiency to some degree. Indeed, our findings demonstrated that 9 months following ACL reconstruction using either a hamstring or BPTB graft, the patients improved their flat, uphill, and downhill walking economy by an average of 9–12 %, attaining 90–95 % of the value observed in individuals with an intact ACL. In support, the only study that examined the effects of ACL reconstruction (using quadruple hamstring auto grafts) on energy cost has also reported improved locomotion efficiency (by 15 %) during level walking at 5.4 km/h both 6 and 12 months post-operatively [4]. Unfortunately, because the authors did not include healthy participants in their study to examine the degree of normalization of the energy cost after ACL reconstruction, direct comparisons with our findings are not possible. Our observations are further supported by biomechanical studies that showed improved, although still impaired, gait knee kinematics at 6 and 12 months post-operatively when compared with healthy subjects [16, 18, 38, 44]. The reduced heart rate and ventilatory responses after ACL reconstruction, irrespective of the type of surgical graft, may well imply an increase in physiologic reserves during locomotion at various walking gradients.
This study assessed whether the energy cost of locomotion returns to normal after ACL reconstruction. Such knowledge is important for orthopaedic surgeons’ daily practice because it provides information on the restoration levels of physiologic reserves and functional capacity after anatomic ACL reconstruction. In practical terms, the increased locomotion economy that we observed after ACL reconstruction implies that a patient may perform the same daily tasks with less effort or more daily tasks with the same effort. Similarly, the athlete or an exercising individual (walker or runner) may train/exercise with increased volume or intensity with similar effort compared with those they were using prior to surgery. This is of major importance because exercise adaptations (exercise-related benefits) are associated with the training load and stimulus [1, 10]. Thus, the improved walking economy may be an additional benefit of ACL reconstruction surgery, irrespective of the type of graft used, that the orthopaedic surgeons should consider.
Treadmill walking was used in this study. Although different energy cost would arise during more vigorous activity (e.g. running), there are physiologic grounds to believe that some of the improvements in the muscles’ efficiency that was observed with walking would be also evident at submaximal running speeds. Further studies are needed to examine the improvement in running economy when performing more vigorous tasks, including “cutting” and “turning” after ACL reconstruction.
Effects of hamstring tendon versus BPTB grafts on walking economy
The present study also examined whether the magnitude of improvement in mechanical energy cost after ACL reconstruction depends on the graft type. Currently, the two main grafts from which to select are the hamstring tendon and BPTB grafts [34]. Although it has been reported that the gait pattern adopted after ACL reconstruction is related to the donor site of the graft [47], both grafts appear to have comparable outcomes regarding the anterior laxity of the knee [13], function of the knee joint, and activity level [26, 33]. Our findings of similar improvements in efficiency and physiologic reserves during locomotion after hamstring tendon and BPTP grafting support the latter observations of similar functional outcomes after ACL reconstruction using either graft. It should be pointed out, however, that straight-line walking tasks were used, with no changes in direction. Based on previous findings [26], it is possible that implementing more vigorous tasks involving rotations of the knee (e.g. steady-state submaximal running with 45° and 90° changes of direction) would unmask differences between the two grafts regarding locomotion efficiency. This point should be examined experimentally. Of note, however, our findings of relatively similar magnitude of improvement in energy cost across conditions of different metabolic demands and types of exercise (uphill and downhill), irrespective of the type of graft, do not support such a view.
Locomotion economy was lower in ACL-deficient patients than in those with healthy ACLs. From a practical point of view, this means that these patients work at higher physiologic reserve and stress for a given exercise than they did prior to the injury, which may lead to greater overall exertion and neuromuscular fatigue. There is consensus in the literature that exertion and fatigue could reduce central motor output and muscular function [11], compromising movement control, reaction time, knee joint kinetics/kinematics, and lower limb joint stability and absorption capacity. Such changes, in turn, could increase the risk of musculoskeletal injury [19]. Sports medicine practitioners should consider these facts when prescribing rehabilitation programs for patients with deficient ACLs, making the appropriate changes to avoid overuse injuries. In particular, the training load should be carefully monitored using subjective (Borg’s scale) and objective (heart rate) measures of exertion. Additionally, some modifications of the aerobic and strength training programs the patients used prior to their injury could be considered, including adjustments to the overall training volume and/or to exercise-to-recovery ratio. The depressed locomotion economy in our study was nearly recovered after ACL reconstruction, with only small attenuation still evident. Thus, post-operative rehabilitation regimens for patients who have undergone ACL reconstruction should aim to increase their aerobic capacity, in conjunction with muscular strength, to restore their metabolic and contractile efficiency.
There were some potential limitations in this study. Only physically fit male patients who had a unilateral ACL injury were included. Our findings might have been different if we had included unfit subjects, female patients, or patients with more complex injuries who may have different oxygen consumption and cardiorespiratory adjustments. Another limitation is that we treated our patients with the same technique for both grafts (i.e. single-bundle anatomic ACL reconstruction). Operations using other techniques (e.g. double-bundle or a traditional technique) might have different effects on the patient’s walking economy. In addition, the patients were evaluated 9 months post-operatively. It is possible that the energy cost of walking for these patients improved earlier, as was evident in a previous study [4].
Conclusion
The present study demonstrated that 9 months after ACL reconstruction with a hamstring tendon or BPTB graft, the patients improved and nearly normalized their walking economy. The cardiorespiratory physiologic reserves also improved, approaching levels observed in individuals with intact ACL. In addition, hamstring tendon and BPTB grafts using a single-bundle anatomic technique elicited similar improvements in walking efficiency and cardiorespiratory effort during flat, uphill, and downhill walking tasks. This study showed that anatomic ACL reconstruction is an operation, with satisfactory short-term results regarding improvements in mechanical energy cost.
References
Baar K (2009) The signaling underlying FITness. Appl Physiol Nutr Metab 34:411–419
Barnes KR, Kilding AE (2015) Running economy: measurement, norms, and determining factors. Sport Med Open 1(1):1–15
Berchuck M, Andriacchi TP, Bach BR, Reider B (1990) Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am 72:871–877
Colak M, Ayan I, Dal U, Yaroglu T, Dag F, Yilmaz C, Beydagi H (2011) Anterior cruciate ligament reconstruction improves the metabolic energy cost of level walking at customary speeds. Knee Surg Sport Traumatol Arthrosc 19:1271–1276
Corcoran PJ, Brengelmann GL (1970) Oxygen uptake in normal and handicapped subjects, in relation to speed of walking beside velocity-controlled cart. Arch Phys Med Rehabil 51:78–87
Czamara A, Markowska I, Królikowska A, Szopa A, Domagalska Szopa M (2015) Kinematics of rotation in joints of the lower limbs and pelvis during gait: early results—SB ACLR approach versus DB ACLR approach. Biomed Res Int 2015:707168
Darter BJ, Rodriguez KM, Wilken JM (2013) Test-retest reliability and minimum detectable change using the K4b 2: oxygen consumption, gait efficiency, and heart rate for healthy adults during submaximal walking. Res Q Exerc Sport 84:223–231
Duffield R, Dawson B, Pinnington HC, Wong P (2004) Accuracy and reliability of a Cosmed K4b2 portable gas analysis system. J Sci Med Sport 7:11–22
Duthon VB, Barea C, Abrassart S, Fasel JH, Fritschy D, Ménétrey J (2006) Anatomy of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 14:204–213
Egan B, Zierath JR (2013) Exercise metabolism and the molecular regulation of skeletal muscle adaptation. Cell Metab 17:162–184
Enoka RM, Duchateau J (2008) Muscle fatigue: what, why and how it influences muscle function. J Physiol 586(1):11–23
Ferber R, Osternig LR, Woollacott MH, Wasielewski NJ, Lee JH (2002) Gait mechanics in chronic ACL deficiency and subsequent repair. Clin Biomech 17:274–285
Gadikota HR, Hosseini A, Asnis P, Li G (2015) Kinematic analysis of five different anterior cruciate ligament reconstruction techniques. Knee Surg Relat Res 27:69–75
Gao B, Zheng N (2015) Alterations in three-dimensional joint kinematics of anterior cruciate ligament-deficient and -reconstructed knees during walking. Clin Biomech 25:222–229
Georgoulis AD, Ristanis S, Chouliaras V, Moraiti C, Stergiou N (2007) Tibial rotation is not restored after ACL reconstruction with a hamstring graft. Clin Orthop Relat Res 454:89–94
Hasegawa T, Otani T, Takeda K, Matsumoto H, Harato K, Toyama Y, Nagura T (2015) Anterior cruciate ligament reconstruction does not fully restore normal 3D knee kinematics at 12 months during walking and walk-pivoting-a longitudinal gait analysis study. J Appl Biomech 31(5):330–339
Hefti F, Müller W (1993) Current state of evaluation of knee ligament lesions. The new IKDC knee evaluation form. Orthopade 22:351–362
Hooper DM, Morrissey MC, Drechsler WI, Clark NC, Coutts FJ, McAuliffe TB (2002) Gait analysis 6 and 12 months after anterior cruciate ligament reconstruction surgery. Clin Orthop Relat Res 403:168–178
Hughes G, Watkins J (2006) A risk-factor model for anterior cruciate ligament injury. Sports Med 36:411–428
Hurd WJ, Snyder-Mackler L (2007) Knee instability after acute ACL rupture affects movement patterns during the mid-stance phase of gait. J Orthop Res 25:1369–1377
Ichinohe S, Yoshida M, Murakami H, Takayama H, Izumiyama S, Shimamura T (2000) Meniscal tearing after ACL reconstruction. J Orthop Surg (Hong Kong) 8:53–59
Iliopoulos E, Galanis N, Iosifidis M, Zafeiridis A, Papadopoulos P, Potoupnis M, Geladas N, Vrabas IS, Kirkos J (2015) Anterior cruciate ligament deficiency reduces walking economy in “copers” and “non-copers.” Knee Surg Sport Traumatol Arthrosc. doi:10.1007/s00167-015-3709-2
Kang J, Chaloupka EC, Mastrangelo MA, Hoffman JR (2002) Physiological and biomechanical analysis of treadmill walking up various gradients in men and women. Eur J Appl Physiol 86:503–508
Kim HS, Seon JK, Jo AR (2013) Current Trends in Anterior Cruciate Ligament Reconstruction. Knee Surg Relat Res 25:165–173
Knoll Z, Kiss RM, Kocsis L (2004) Gait adaptation in ACL deficient patients before and after anterior cruciate ligament reconstruction surgery. J Electromyogr Kinesiol 14:287–294
Li S, Chen Y, Lin Z, Cui W, Zhao J, Su W (2012) A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone–patellar tendon–bone autografts for the reconstruction of the anterior cruciate ligament. Arch Orthop Trauma Surg 132:1287–1297
Limbird TJ, Shiavi R, Frazer M, Borra H (1988) EMG profiles of knee joint musculature during walking: changes induced by anterior cruciate ligament deficiency. J Orthop Res 6:630–638
Malatesta D, Simar D, Dauvilliers Y, Candau R, Borrani F, Prefaut C, Caillaud C (2003) Energy cost of walking and gait instability in healthy 65- and 80-yr-olds. J Appl Physiol 95(6):2248–2256
Mattsson E, Broström LA, Linnarsson D (1990) Changes in walking ability after knee replacement. Int Orthop 14:277–280
McHugh MP, Spitz AL, Lorei MP, Nicholas SJ, Hershman EB, Gleim GW (1994) Effect of anterior cruciate ligament deficiency on economy of walking and jogging. J Orthop Res 12:592–597
McLaughlin JE, King GA, Howley ET, Bassett DR, Ainsworth BE (2001) Validation of the COSMED K4 b2 portable metabolic system. Int J Sports Med 22:280–284
Middleton KK, Hamilton T, Irrgang JJ, Karlsson J, Harner CD, Fu FH (2014) Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1. Knee Surg Sport Traumatol Arthrosc 22:1467–1482
Razi M, Sarzaeem MM, Kazemian GH, Najafi F, Najafi MA (2014) Reconstruction of the anterior cruciate ligament: a comparison between bone-patellar tendon-bone grafts and fourstrand hamstring grafts. Med J Islam Repub Iran 28:134
Romanini E, D’Angelo F, De Masi S, Adriani E, Magaletti M, Lacorte E, Laricchiuta P, Sagliocca L, Morciano C, Mele A (2010) Graft selection in arthroscopic anterior cruciate ligament reconstruction. J Orthop Traumatol 11:211–219
Samuelsson K, Andersson D, Karlsson J (2009) Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy 25:1139–1174
Schrack JA, Simonsick EM, Ferrucci L (2010) Comparison of the cosmed K4b2 portable metabolic system in measuring steady-state walking energy expenditure. PLoS ONE 5(2):e9292
Schurz M, Tiefenboeck TM, Winnisch M, Syre S, Plachel F, Steiner G, Hajdu S, Hofbauer M (2015) Clinical and functional outcome of all-inside anterior cruciate ligament reconstruction at a minimum of 2 years’ follow-up. Arthroscopy 32(2):332–337
Shabani B, Bytyqi D, Lustig S, Cheze L, Bytyqi C, Neyret P (2014) Gait knee kinematics after ACL reconstruction: 3D assessment. Int Orthop 39(6):1187–1193
Simon D, Mascarenhas R, Saltzman BM, Rollins M, Bach BR, MacDonald P (2015) The relationship between anterior cruciate ligament injury and osteoarthritis of the knee. Adv Orthop 2015:928301
Solomon SJ, Kurzer MS, Calloway DH (1982) Menstrual cycle and basal metabolic rate in women. Am J Clin Nutr 36:611–616
Steckel H, Murtha PE, Costic RS, Moody JE, Jaramaz B, Fu FH (2007) Computer evaluation of kinematics of anterior cruciate ligament reconstructions. Clin Orthop Relat Res 463:37–42
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:42–49
Tengman E, Grip H, Stensdotter AK, Häger CK (2015) Anterior cruciate ligament injury about 20 years post-treatment: a kinematic analysis of one-leg hop. Scand J Med Sci Sports 25(6):818–827
Timoney JM, Inman WS, Quesada PM, Sharkey PF, Barrack RL, Skinner HB, Alexander AH (1993) Return of normal gait patterns after anterior cruciate ligament reconstruction. Am J Sport Med 21:887–889
Waters RL, Lunsford BR, Perry J, Byrd R (1988) Energy-speed relationship of walking: standard tables. J Orthop Res 6:215–222
Waters RL, Mulroy S (1999) The energy expenditure of normal and pathologic gait. Gait Posture 9:207–231
Webster KE, Wittwer JE, O’Brien J, Feller JA (2005) Gait patterns after anterior cruciate ligament reconstruction are related to graft type. Am J Sports Med 33:247–254
Wong JM-L, Khan T, Jayadev CS, Khan W, Johnstone D (2012) Anterior cruciate ligament rupture and osteoarthritis progression. Open Orthop J 6:295–300
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iliopoulos, E., Galanis, N., Zafeiridis, A. et al. Anatomic single-bundle anterior cruciate ligament reconstruction improves walking economy: hamstrings tendon versus patellar tendon grafts. Knee Surg Sports Traumatol Arthrosc 25, 3155–3162 (2017). https://doi.org/10.1007/s00167-016-4229-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4229-4