Abstract
Purpose
The indications, incidence, outcomes, and survivorship of stems in primary total knee arthroplasty (TKA) are lacking in the contemporary literature. Our hypothesis is stems in primary TKA would result in worse outcomes and survivorship.
Methods
All primary TKAs between 2007 and 2011 with 2-year follow-up were identified. Revision TKA or UKA conversion was excluded. Demographic information (age, sex, race, BMI, primary diagnosis, and Charlson–Deyo comorbidity index), outcome measures including KOOS and WOMAC, and any revisions were identified from the registry. A 2:1 matched cohort of non-stemmed/stemmed primary TKA patients was created to compare revision rates and outcomes at baseline and 2 years post-TKA. Subgroup analyses of long versus short stems, 1 versus 2 stems, and cemented versus hybrid stem fixation were completed. Two-sample t tests and Chi-square tests were used to compare conventional and stemmed TKA groups.
Results
The registry review included 13,507 conventional TKA and 318 stemmed TKA resulting in an incidence of 2.3 % in primary TKA. The mean follow-up was approximately 49 months in both groups. No difference was found in revision rates between stemmed TKA (2.5 %) and conventional TKA (2.2 %). Patients with post-traumatic arthritis had an odds ratio of 10.5 (95 % CI 1.2–15.3) of receiving stems. Stem length did not affect revision rates. Patients with two stems had worse KOOS and WOMAC scores at baseline which equalized to single-stem patients at 2 years.
Conclusions
The use of stems may provide a survival benefit in complex primary TKA over the short term and no adverse effect on patient outcomes or satisfaction.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stems are intramedullary extensions of either the femoral or tibial component of a total knee arthroplasty (TKA) and are thought to increase the mechanical stability of the implants and decrease the risk of aseptic loosening. Biomechanical studies have shown that stems increase the mechanical stability of the femoral and tibial components [1, 5, 12, 15]. Stems are thought to transfer load over a larger area and thereby reduce strain at the bone–cement or bone–component interface, for cemented and non-cemented reconstructions. Finite element analysis of tibial stems found cemented and uncemented stems transferred 24 and 6 %, respectively, of an applied axial load to the diaphyseal bone [4]. The cemented and press-fit tibial stems reduced micromotion by 23 and 19 %, respectively, compared to a conventional stemless tibial baseplate [4]. A similar finite element analysis of femoral stems found that cemented and press-fit stems transferred 58 and 17 %, respectively, of the applied axial load from the femoral component to the diaphyseal bone [3]. The cemented and press-fit stems reduced medial–lateral femoral component micromotion by 41 and 24 %, respectively [3]. TKA stems are largely reserved for revision TKA, but indications for stem use in primary TKA include: previous non-arthroplasty implants, obesity, severe deformity, or instability requiring constrained components. A dearth of the literature was found that described the indications, incidence, survivorship, and outcomes of stems in primary TKA. The present study describes these characteristics in a large series from an institutional registry at a high-volume orthopaedic hospital which has not been previously reported in the literature for primary TKA. The survivorship of a primary TKA with stems is unknown, and our hypothesis was that stems portended a worse outcome and survivorship because of the increased complexity of the primary procedure and a patient population that was more challenging than the usual adult with osteoarthritis. The purpose of the current study was to identify the incidence, indications, and outcomes of stems in primary TKA at a single orthopaedic specialty care hospital.
Materials and methods
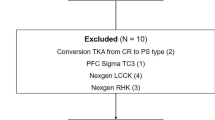
An IRB-approved institutional registry at a high-volume orthopaedic hospital was used to identify all primary TKAs between 1 May 2007 and 31 December 2011 (Hospital for Special Surgery IRB No. 2015-131). All patients who underwent a primary TKA during this time period and had at least 2-year follow-up were included. Knees with previous high-tibial osteotomy, distal femoral osteotomy, intramedullary nails, osteosynthesis plates, or other non-arthroplasty implants were included. Patients with prior TKA or conversion of a UKA were excluded. Patients were also excluded if they had inadequate pre-operative and post-operative imaging. Patients undergoing joint replacement associated with oncologic resection were also excluded.
TKA device information was captured in the registry. Within this cohort of primary TKA, the use of knee stems was identified. Post-operative radiographs were reviewed to verify the presence of stem and stem type for each patient. The minimum length considered a stem in this study was 30 mm. Long stems were defined by length >80 mm, and short stems were ≤80 mm. Digital radiographs from the institutional picture archive and communication system (PACS, Sectra IDS 7, Linköping, Sweden) were calibrated with a sizing ball using electronic templating software. Deformity was assessed using a pre-operative weight-bearing AP radiograph; severe varus/valgus deformity was defined as >15 degrees using the anatomic axes of the femur and tibia. Pre-operative radiographs were reviewed for prior implant, osteotomy, or fracture (Figs. 1–2).
The registry also provides selected baseline demographic information including age, sex, race, BMI, primary diagnosis, and Charlson–Deyo comorbidity index. Clinical outcome measures including the Knee Injury and Osteoarthritis Outcome Score (KOOS) and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) were collected pre-operatively and post-operatively at 2-year follow-up. Patients’ satisfaction was evaluated at 2-year follow-up based on a previously developed satisfaction survey. Patients were asked five questions about their satisfaction with the results of their knee surgery for relieving pain, improving ability to do housework or yard work, improving ability to do recreational activities, improving quality of life, and overall satisfaction. Quality of life responses were collected on a 6-point Likert scale as (1) More improvement than I ever dreamed possible, (2) A great improvement, (3) A moderate improvement, (4) A little improvement, (5) No improvement at all, and (6) The quality of my life is worse. All other satisfaction question responses were collected on a 5-point Likert scale as (1) very satisfied, (2) somewhat satisfied, (3) neither satisfied nor dissatisfied, (4) somewhat dissatisfied, and (5) very dissatisfied. Revisions were identified using ICD-9-CM codes.
To minimize confounding patient characteristics on survivorship and patient-reported outcomes, a match analysis was also performed. Conventional TKA patients were matched to stemmed TKA patients on age (±5), sex, WHO BMI classification, laterality (simultaneous bilateral versus unilateral), and Charlson–Deyo comorbidity index. Differences in 30-day readmission rate, revision rate, surgery satisfaction, and clinical outcome measures (KOOS and WOMAC) measured at baseline and 2 years post-TKA were compared between patients with and without stems in the matched cohort. Differences in revision rate, surgery satisfaction, and clinical outcomes were also analysed in subgroups of long (>80 mm) versus short stem (≤80 mm), 1 versus 2 stems, and cemented versus hybrid stem fixation.
To determine the optimal matching ratio, a power calculation was executed. The power calculation demonstrated that a matching ratio of 2:1, conventional to stemmed, achieves an adequate statistical power and increases the efficiency of estimates compared to a 1:1 matching ratio. Using a standard deviation estimate of 25 points in each group, the available sample size of the stemmed group and its 2:1 matching non-stemmed cohort achieve 99 % power to detect a minimum clinically important difference of 8 points in the KOOS function score. A revision rate of 3.4 % was determined as the threshold for a clinically significant difference at 80 % power between the matching groups.
Statistical analysis
Continuous data were summarized as means and standard deviations. Categorical data were expressed as frequencies and percentages. Two-sample t tests and Chi-square tests were used to compare the difference in the patient demographics, rates of revision, and primary diagnosis between stemmed and conventional TKA groups. The statistical significance level was set at 0.05 for all comparisons. The relationship between primary diagnosis and stem use in TKA was further assessed using logistic regression analysis. Reliability measurements were not completed for this study as only one observer performed radiographic measurements of knee alignment. All statistical analyses were performed with SAS version 9.3 (SAS Institute, Cary, NC, USA).
Results
Overall
The institutional registry review included 13,507 conventional TKA and 318 stemmed TKA resulting in an incidence of stems in primary TKA as 2.3 %. The principal finding of the study was a similar revision rate between stemmed TKA (2.5 %) and conventional TKA (2.2 %). Fifty-one per cent of stemmed TKA had both femoral and tibial stems, 30 % were tibial only, and 19 % were femoral only. In the overall cohort, the mean follow-up was nearly identical at 49 months for both conventional and stemmed TKA patients. The 2-year follow-up rate was 74.0 % in the conventional TKA group and 65.0 % in the stemmed TKA patients. No significant difference existed between age, BMI, and Charlson–Deyo comorbidity index between patients who received a stemmed TKA versus conventional TKA (Table 1). The entire cohort was 63.9 % female, and significantly more females received stemmed TKA (p = 0.04).
The indication for primary TKA was osteoarthritis more commonly in the conventional TKA group compared to the stemmed TKA group (p < 0.01) (Table 1). In comparison, the indication for TKA was post-traumatic arthritis in 11.6 % of the stemmed TKA group compared to only 1.2 % of the conventional group (p < 0.01) (Table 1). Patients with post-traumatic arthritis were 10.5 (95 % CI 1.2–15.3) times more likely to receive stems at primary TKA. In the stemmed TKA group, 9.5 % (n = 21) of females compared to 16.5 % (n = 16) male had post-traumatic arthritis as their primary diagnosis (n.s.) (Table 2). In the conventional TKA group, more females had rheumatoid arthritis (p < 0.01), but no difference in rheumatoid arthritis prevalence was seen between males and females in the stemmed TKA group (Table 2). Patients with inflammatory arthritis were 1.3 (0.5, 3.2) times more likely to require stems at primary TKA. Post-operative and pre-operative radiographs were reviewed to confirm the presence of a TKA stem as well as to assess for constrained components, severe pre-operative deformity (femoral–tibial angle of >15° varus/valgus), or previous orthopaedic implants for fracture or osteotomy. Within the 318 patients with TKA stems, 74 (23.3 %) had previous orthopaedic implants, and 162 (50.1 %) had severe deformity (Figs. 3–4).
Matched cohort
In total, 318 patients were identified in the stemmed TKA group, and of those, 291 met the study inclusion and exclusion criteria for matching 1:2 with the conventional TKA group. In the matched cohort of 291 stemmed TKAs and 582 conventional TKAs, there was no difference in revision rates within the matched cohorts, 2.9 versus 2.4 %, respectively (n.s.). Mean follow-up was 52.6 ± 17.0 months for conventional TKA and 49.8 ± 17.3 months for stemmed TKA patients. The 2-year follow-up rate was 69.0 % in the conventional TKA group and 67.0 % in the stemmed TKA group. Within the matched cohorts, the previous findings regarding indications held true. Significantly more conventional TKA patients had a diagnosis of osteoarthritis (93.8 %) compared to stemmed TKA (82.5 %) (p < 0.01) (Table 3). Stemmed TKA patients more frequently underwent TKA secondary to post-traumatic arthritis (12.4 vs. 2.2 %; p < 0.01) (Table 3). Post-traumatic arthritis was 6.2 (3.2, 11.9) more likely in the stemmed TKA group.
Within the matched cohorts, no difference in WOMAC scores was noted between the matched cohorts at baseline and at 2 years. KOOSs were identical at baseline, but the stemmed TKA had lower KOOS sports and recreation scores (p < 0.01) and KOOS quality of life scores (p = 0.04) at 2-year follow-up (Table 3). When asked “how much has your surgery improved your life”? using a five-point scale, the stemmed TKA patients tended to more frequently answer “more improvement than I ever dreamed possible”, but this was not statistically significant (n.s.) (Table 3).
Short versus long stems
The effect of stem length on survivorship and outcomes in primary TKA was examined. A stem length ≥80 mm was arbitrarily considered a long stem. The incidence of long stems was 35.2 % within the cohort (Table 4). When considering short (≤80 mm) versus long (≥80 mm), there was no difference in revision rates (n.s.) (Table 4). Additionally, there was no difference in patient satisfaction, KOOS, or WOMAC scores at baseline or 2 years between the two groups (Table 4).
One versus two stems
The study compared the effect of a single stem to two stems on the outcome of the primary TKA. The incidence of a single femoral or tibial stem was 64.5 %. Patients requiring both femoral and tibial stems had significantly worse KOOS pain (p < 0.01) and stiffness (p < 0.01) scores at baseline which equalized at 2 years to single-stem patients (Table 5). Patients with both femoral and tibial stems also had worse WOMAC pain (p < 0.01) and symptoms (n.s.) scores at baseline which also equalized to the single-stem cohort at 2 years (Table 5). Patient satisfaction was not significantly different between the one-stem and two-stem cohorts.
Cemented versus uncemented stems
The incidence of cemented versus uncemented stems was determined for the entire stemmed primary TKA cohort by reviewing each post-operative radiograph. Appropriate radiographs were available in 145 patients with a single stem and 152 patients with two stems. The single stem was cemented in 22.1 % (n = 32) of patients. The single tibial stem was cemented 25.0 % (n = 10) of patients, and the single femoral stem was cemented in 17.5 % (n = 22) of patients. The two stems were cemented in 52.6 % (n = 80) of patients (Table 6). The single non-cemented stem TKA revision rate (1.8 %) and the single cemented stem TKA revision rate (3.1 %) were not statistically significant (n.s.). The two non-cemented stems revision rate (4.2 %) and the two cemented stems revision rate (2.5 %) were not statistically significant (n.s.) (Table 7). Overall, the revision rate for primary TKA with cemented and non-cemented stems was identical at 2.7 % (n.s.) (Table 8). A Kaplan–Meier curve comparing non-cemented and cemented TKA with single and two stems found no difference in survivorship (n.s.) (Fig. 5).
Discussion
The most clinically relevant finding of the present study is that stems did not negatively affect survivorship of primary TKA. Stems are intramedullary devices used with femoral or tibial knee arthroplasty components to increase stability. Reports of the outcomes of stems used in primary TKA are sparse. The study hypothesis was that stems portended a worse outcome and survivorship because of the increased complexity of the primary procedure and a patient population that was more challenging than the usual adult with osteoarthritis. The purpose of the current study was to identify the incidence, indications, and outcomes of stems in primary TKA at a single institution. The study found that stems were used in primary TKA in 2.4 % of primary TKA procedures at a high-volume orthopaedic referral centre over a 5-year period. Contrary to our hypothesis, primary TKA requiring stems did not demonstrate an increased revision rate suggesting a survival benefit. Based on the single-institution registry, surgeons were more likely to use stems in patients with post-traumatic or inflammatory arthritis and the results were similar to conventional TKA patients at 2 years. When comparing stemmed TKA versus conventional TKA, no difference in the revision rate was found in either the overall or the matched cohorts. Patients with stemmed TKA had worse KOOS quality of life scores at 2 years than conventional TKA, but the remainder of patient-reported outcome measures including WOMAC and patient satisfaction were not significantly different. The mean BMI in the stemmed group was not higher, though the variability was greater.
As mentioned previously, the predominance of the literature regarding stems focuses on revision TKA. The revision TKA literature was reviewed to assess the survivorship of the stemmed primary TKA compared to the stemmed revision TKA. Haas et al. reviewed 74 patients (76 knees) with 42-month follow-up who underwent a hybrid revision TKA with both femoral and tibial stems between 1980 and 1988. The 8-year survival was 83 %, and the complication rate was 13 %. The authors did not discuss indications for stem fixation [9]. A more recent cohort of hybrid revision TKA with stems from the same institution reported a 9 % failure rate at a mean follow-up of 38 months. Most patients had pain with walking (88 %) and stair climbing (90 %). Again, patient selection was not discussed [2]. Sah et al. reported 100 % survivorship at 5 years and 90 % survivorship at 10 years for revision hybrid stemmed TKA in a group of 83 patients (88 knees) with an average follow-up of 65 months (24–126 months). The authors noted radiosclerotic lines adjacent to the stems were frequently identified, but were not associated with implant loosening [16]. Mabry et al. [11] reported the 98 % survivorship at 5 years and 92 % survivorship at 10 years in a group of 72 revision TKA patients (73 knees) with an average follow-up of 10.2 years. A large series of 184 hybrid stem revision TKAs with stems reported a failure rate of 8.2 % (15/184) at a mean of 49 months. The majority (13/15) were septic failures including nine re-infections and four denovo infections [13, 14]. Good et al. reported 87 % survivorship in 135 hybrid stem revision TKAs (127 patients) at a mean follow-up of 5 years (2–12 years). Re-revisions included two for MCL insufficiency, two for deep infection, and two for aseptic loosening that occurred at a mean of 3.5 years [17]. A recent multicentre study of aseptic revision TKA comparing cemented versus hybrid stem fixation found no difference in aseptic loosening or outcomes between the two groups. The re-revision rate for cemented stems (3 %) versus hybrid stem fixation (4 %) was not statistically different [7]. A similar multicentre study comparing cemented versus hybrid stem fixation for septic TKA revision found no difference in reinfection rate, but found less radiographic loosening in the hybrid stem fixation group (17 vs. 32 %). No correlation was identified between radiographic loosening and level of constraint nor articulating versus static space in the first-stage operation [6]. A recent study of aseptic and septic revision TKA with hybrid stem fixation in 119 patients reported a low re-revision rate of 2.5 % at a mean of 62 months. Radiographic loosening was not observed in any of the surviving patients, and no re-revisions were performed for aseptic loosening [8]. In contrast to the previous study, a recent series of 54 patients undergoing revision of the tibial baseplate only with 30-mm cemented tibial stems reported no tibial revisions for aseptic loosening at a mean follow-up of 5 years although radiolucent lines were observed in 46 % of patients [10]. In summary, the contemporary literature supports both cemented and hybrid stem fixation without a strong survivorship preference for one technique over the other.
Based on the contemporary literature that focuses only on revision TKA, the effect of stems on the survivorship and outcomes on primary TKA is unknown. We suspected that survivorship for a primary TKA requiring stems would be inferior to conventional primary TKA; however, the results proved otherwise by showing similar survivorship over a mean follow-up of approximately 4 years. This suggests that stems have a beneficial effect on the survival of primary TKA in a complex patient, and the arthroplasty surgeon can be confident that a primary TKA requiring stems are not doomed to an inferior outcome.
The major limitations of the current study are less than 80 % follow-up at 2 years and the short mean follow-up for an arthroplasty study. Both of these weaknesses are attributable to a single referral centre registry in which patients are not captured and may not return for continued long-term follow-up due to inconvenience, cost, or geographical distance. Strong registry data require significant resources to achieve robust follow-up. A limitation of the study was the failure to identify the surgeons’ reason for using stems in primary TKA as this information was not reliably conveyed in the operative reports. Rather, the authors inferred the indication for the stem using diagnosis codes and radiographs to assess for previous implants or severe deformity. As the patients were treated at an orthopaedic referral centre, medical complications, such as VTE, DVT, PE, pneumonia, and urinary tract infections, may have been treated elsewhere and could not be accurately assessed. We believe the majority of surgical complications were captured by the registry review as most patients return to their surgeon for revision procedures, but there may be patients with medical complications, implant failure, or joint sepsis who were treated elsewhere. Single-centre registry series are inherently at risk of over-estimating their success depending on how many patients seek care for complications elsewhere.
A strength of the study is the large number of patients who underwent a primary TKA with a stem and the comparison group of nearly 14,000 primary TKAs. Using mandatory implant data records, we are confident that all patients with a stemmed primary TKA were included. The study achieved the goals of determining the incidence, indications, and early outcomes of stemmed primary TKA. This information is clinically relevant to counsel patients pre-operatively and reassures surgeons that a stemmed primary TKA does not portend a worse outcome.
Conclusions
Stems were used in approximately 2.4 % of primary total knee arthroplasties with a similar revision rate to conventional TKA. Survivorship was similar among cemented versus uncemented stems in this series. In conclusion, the study demonstrates that the use of stems may provide a survival benefit in complex primary TKA over the short term and no adverse effect on patient outcomes or satisfaction.
References
Bertin KC (2007) Tibial component fixation in total knee arthroplasty: a comparison of pegged and stemmed designs. J Arthroplasty 22(5):670–678
Bottner F, Laskin R, Windsor RE, Haas SB (2006) Hybrid component fixation in revision total knee arthroplasty. Clin Orthop Relat Res 446:127–131
Completo A, Simoes J, Fonseca F (2009) Revision total knee arthroplasty: the influence of femoral stems in load sharing and stability. Knee 16(4):275–279
Completo A, Simões J, Fonseca F, Oliveira M (2008) The influence of different tibial stem designs in load sharing and stability at the cement–bone interface in revision TKA. Knee 15(3):227–232
Conlisk N, Gray H, Pankaj P, Howie C (2012) The influence of stem length and fixation on initial femoral component stability in revision total knee replacement. Bone Joint Res 1(11):281–288
Edwards PK, Fehring TK, Hamilton WG, Perricelli B, Beaver WB, Odum SM (2014) Are cementless stems more durable than cemented stems in two-stage revisions of infected total knee arthroplasties? Clin Orthop Relat Res 472(1):206–211
Gililland JM, Gaffney CJ, Odum SM, Fehring TK, Peters CL, Beaver WB (2014) Clinical & radiographic outcomes of cemented vs. diaphyseal engaging cementless stems in aseptic revision TKA. J Arthroplasty 29(9):224–228
Greene JW, Reynolds SM, Stimac JD, Malkani AL, Massini MA (2013) Midterm results of hybrid cement technique in revision total knee arthroplasty. J Arthroplasty 28(4):570–574
Haas SB, Insall JN, Montgomery W, Windsor RE (1995) Revision total knee arthroplasty with use of modular components with stems inserted without cement. J Bone Joint Surg Am 77(11):1700–1707
Lachiewicz PF, Soileau ES (2015) A 30-mm cemented stem extension provides adequate fixation of the tibial component in revision knee arthroplasty. Clin Orthop Relat Res 473(1):185–189
Mabry TM, Vessely MB, Schleck CD, Harmsen WS, Berry DJ (2007) Revision total knee arthroplasty with modular cemented stems: long-term follow-up. J Arthroplasty 22(6):100–105
Pérez-Blanca A, Prado M, Ezquerro F, Montañéz E, Espejo A (2008) Addition of a short central extension to surface cemented tibial trays in primary TKA: an in vitro study of the effect on initial fixation stability and its relationship to supporting bone density. Clin Biomech 23(4):483–492
Peters CL, Erickson J, Kloepper RG, Mohr RA (2005) Revision total knee arthroplasty with modular components inserted with metaphyseal cement and stems without cement. J Arthroplasty 20(3):302–308
Peters CL, Erickson JA, Gililland JM (2009) Clinical and radiographic results of 184 consecutive revision total knee arthroplasties placed with modular cementless stems. J Arthroplasty 24(6):48–53
Rawlinson JJ, Peters LE, Campbell DA, Windsor R, Wright TM, Bartel DL (2005) Cancellous bone strains indicate efficacy of stem augmentation in constrained condylar knees. Clin Orthop Relat Res 440:107–116
Sah AP, Shukla S, Della Valle CJ, Rosenberg AG, Paprosky WG (2011) Modified hybrid stem fixation in revision TKA is durable at 2 to 10 years. Clin Orthop Relat Res 469(3):839–846
Wood GC, Naudie DD, MacDonald SJ, McCalden RW, Bourne RB (2009) Results of press-fit stems in revision knee arthroplasties. Clin Orthop Relat Res 467(3):810–817
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barlow, B.T., Oi, K.K., Lee, Yy. et al. Incidence, indications, outcomes, and survivorship of stems in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25, 3611–3619 (2017). https://doi.org/10.1007/s00167-016-4227-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4227-6