Abstract
Purpose
Lateral progression of arthritis following medial unicompartmental knee arthroplasty (UKA), although infrequent, is still the most common reason for revision surgery. Treatment options normally include conversion to total knee arthroplasty. An alternative strategy for some patients may be addition of a lateral UKA. We report the first results of staged bi-compartmental UKA (Bi-UKA) strategy.
Methods
We retrospectively selected from our UKA database patients who underwent a lateral UKA to treat a symptomatic lateral osteoarthritis progression after a medial UKA. The analysis included a clinical and radiological assessment of each patient.
Results
Twenty-five patients for a total of 27 knees of staged Bi-UKA were carried out in a single centre. The mean time interval between primary medial UKA and the subsequent lateral UKA was 8.1 years (SD ± 4.6 years). The mean age at the time of the Bi-UKA was 77.1 years (SD ± 6.5 years). The median hospital stay was 3 (range 2–9 days) days, and the mean follow-up after Bi-UKA was 4 years (SD ± 1.9 years). The functional scores showed a significant improvement as compared to the pre-operative status (paired t test, p = 0.003). There were no radiological evidences of failure. None of the patients needed blood transfusion, and there was no significant complications related to the surgical procedure without further surgeries or revisions at final follow-up.
Conclusions
These results suggest that addition of a lateral UKA for arthritis progression following medial UKA is a good option in appropriately selected patients.
Level of evidence
Observational study without controls, Level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Medial unicompartmental knee arthroplasty (UKA) is a successful treatment for end-stage anteromedial osteoarthritis (OA). It has many advantages compared to total knee arthroplasty (TKA) including less morbidity and mortality, improved tissue preservation, more rapid recovery with reduced hospital stay and greater implant function [13, 14, 17, 19, 22]. Its disadvantage is that it has a higher revision rate due primarily to progression of OA in the lateral compartment [21]. Although the incidence varies in different series and joint registry reports, the risk of developing severe lateral compartment osteoarthritis (LCOA) requiring revision after medial UKA is low, especially if overcorrection is avoided [15, 20]. In a recently published series of 1000 cemented Phase 3 Oxford UKAs with up to 15-year follow-up, 25 (2.5 %) patients required revision for lateral progression at a mean of 7.0 years (range 1.9–11.4 years) [19]. In Svard’s 20-year series, the revision rate for LCOA was 2.3 % [20]. In the National Joint Registry (NJR), lateral progression as the reason for revision following UKA is 2.6 % [6].
The standard treatment for LCOA after medial UKA is revision to TKA. This usually involves the removal of a well-fixed and well-functioning medial UKA and exposes these patients to the risks of revision knee arthroplasty. If the medial UKA is functioning well, then a feasible option is to implant a lateral UKA with the potential advantages of recovery following UKA surgery and lower risks this entails. While simultaneous bi-unicompartmental UKA is regaining interest amongst surgeons to treat bi-compartmental knee OA, this paper focuses on the implementation of a staged unicompartmental knee replacement to be performed in those patients with LCOA progression after medial UKA, as an alternative and less invasive treatment option to revision TKA. At present, there are no clinical data available for this indication using the technique described in this paper. This paper describes indications, key surgical steps and preliminary results of lateral UKA (for progression of osteoarthritis in the lateral compartment after medial UKA) carried out in a consecutive series of 27 patients in a single centre.
Materials and methods
Between 2006 and 2014, 25 patients (27 knees) underwent a “two-stage” Bi-UKA knee replacement for symptomatic “bone-on-bone” arthritis in the lateral compartment following medial Oxford UKA (Zimmer Biomet, Swindon, UK). Before the lateral UKA, a clinical and radiological assessment of each patient was performed. Clinical assessment included Oxford Knee Score (OKS), Tegner score and American Knee Society Score Objective and Functional (AKSS-O and -F) [4, 16, 23], while radiological evaluation included AP, Rosenberg, lateral and skyline views [9].
This is a retrospective study of prospectively collected data. Ethics approval was not requested for the study design as previous communication with the Chair of local ethic committee confirmed that for such a study formal ethical approval is not necessary.
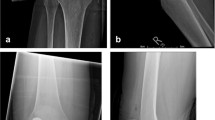
All patients were prospectively followed by an independent physiotherapist at 6 weeks, 1, 2, 5 and 7 years. The pre-operative clinical assessment was repeated along with an aligned AP and lateral radiographs, to study the progression of OA in the retained compartments. The radiographs were taken using fluoroscopy using a method described previously [24]. The X-ray beam was aligned parallel to the tibial base plate for the AP radiograph and centred over the femoral condyle for the lateral radiograph. Progression of OA in the retained lateral compartment was confirmed by comparing the joint space on immediate post-operative radiographs and subsequent ones. In the patients described, there was clear evidence of progression of OA with the presence of bone on bone in the lateral compartment. In addition, in none of the patients there was any evidence of implant loosening (medial UKA) or the presence of pathological radiolucency under the tibial tray [8]. Assessment of post-operative radiographs confirmed satisfactory alignment of the medial UKA in all the patients as recommended by Goodfellow et al. [6]. All the post-operative radiographs were assessed by an independent observer twice with an interval of 4 weeks between the two assessments.
The surgical technique was similar to that for a primary lateral Oxford Domed Lateral UKA. The medial UKA incision was opened and extended proximally and distally. The lateral compartment was approached using a lateral parapatellar arthrotomy. Final decision on LCOA treatment was taken intra-operatively, after direct visualisation and joint evaluation. Thus, prompt availability of total knee implants and both mobile- and fixed-bearing lateral UKA is mandatory. If the PFJ was severely damaged with substantial bone loss laterally, patients were not considered for the current series, as a TKA was performed. If the ACL was found to be non-functional, a decision on whether to do a TKA or a fixed-bearing lateral UKA (Vanguard M tibial component and Oxford femoral component) depended on the patient’s age, health and referred symptoms, with instability being an indication towards TKA. The components were cemented. The post-operative recovery was managed as for primary UKA.
There were 16 males (64 %) and 9 females (36 %). The mean age of the patients at the time of the primary medial UKA was 68.9 years (standard deviation (SD) ± 6.1 years), and the mean age at the time of the lateral UKA was 77.1 years (SD ± 6.5 years). The mean time between implantation of the primary medial UKA and the lateral UKA was 8.1 years (SD ± 4.6 years). The indication for the primary procedure was anteromedial OA in all the patients. The mean follow-up since the lateral UKA was 4.0 years (SD ± 1.9 years). A mobile-bearing Oxford Domed Lateral UKA was used in 19 patients (70 %), while a fixed-bearing lateral UKA was used in eight patients (30 %), as the ACL was non-functional in these patients at the time of implanting a lateral UKA.
Statistical analysis
A paired t test was used to compare the clinical outcome data with pre-operative scores. Survival, with failure defined as any revision, was assessed using the life table method, with 95 % confidence intervals (CI) calculated using the method described by Peto et al. Revision was defined as any further operative intervention. A p value of <0.05 was considered statistically significant.
Primary outcome measure was length of stay. The median length of stay of patients treated with lateral UKA was 3 days with a reduction by 1 day being considered clinically significant. Assuming a standard deviation of 1.25 days (as is the case in our centre), a sample size of 25 knees per arm is required to detect this clinically relevant difference with 80 % power and 5 % two-sided significance.
Results
The median hospital stay was 3 days (range 2–9 days), and none of the patients needed blood transfusion. There were no significant medical complications, no re-admissions, no requirement for manipulation under anaesthesia and no mortality related to the surgical procedure. None of the patients needed a further intervention, one patient died 4.3 years after the second operation (due to unrelated causes) and no patients were lost to follow-up; therefore, the 5-year survival is 100 % (number at risk = 15).
The intra-observer correlation (r) was 0.94. There were no patients with radiological evidence of failure, in terms of progression of PFJ OA or radiolucencies.
The functional outcome is presented in Table 1. All the scores showed a significant improvement as compared to the pre-operative status (p = 0.003). Average knee flexion was 123.0° (SD ± 16.0°).
Discussion
The most important finding of this study was the low complications rate and quicker recovery after a staged Bi-UKA as a viable option to treat symptomatic end-stage lateral compartment arthritis after medial UKA. It is particularly advantageous as many patients with this condition are elderly often with significant comorbidities.
There are many advantages of lateral UKA compared to TKA for treating lateral OA after a primary medial UKA. There is minimal soft tissue or bony damage, recovery is fast, hospital stay is comparable to primary UKA and therefore shorter than TKA. Patients tend to get a good range of flexion. The clinical outcome, as evidenced by the OKS (mean 36.5), is only slightly worse than that of a primary medial UKA if it was implanted in patients of similar age (mean OKS 40.0 (SD ± 8.0) in patients 70 years or above). It is also better than that reported following primary TKA in national databases (mean OKS 34) [2], although this is not necessarily an appropriate comparison. The procedure is not only safe but also still gives the surgeon an option of conversion to a TKA if the need arises in the future.
As regards the surgical technique, extending the previous medial parapatellar skin incision and using a lateral parapatellar approach to implant a lateral UKA decrease the risk of skin necrosis, avoiding a cutaneous bridge between two scars. After the approach, the surgeon can evaluate the state of the lateral compartment, the ACL and the PFJ (the medial compartment is not seen well), and decide how to proceed. The domed lateral mobile UKA is appropriate if the ACL is intact [25]. However, a fixed-bearing UKA may be more appropriate for surgeons inexperienced with the domed lateral or if the ACL is non-functional. In these patients; even though described in simultaneous Bi-UKA [21], a combined lateral UKA and ACL reconstruction may not be considered as a feasible option because of the further difficulties it may add to the procedure. If cruciate ligaments are intact, it is expectable that the final result is comparable to a bicruciate retaining TKA, in terms of proprioception and kinematics. The staged Bi-UKA option shares the same advantages of that implant design, which is nowadays gaining greater interest.
As reported in the original paper on simultaneous Oxford Bi-UKA, convergence or divergence of the components does not matter because of their spherical design and the fully congruous freely mobile bearings (Figs. 1, 2). This may lead to the conclusion that when doing the lateral UKA the position and orientation of the medial UKA components may be ignored. Although the slope of the tibial components should be similar (about 7° as set by the tibial saw guide), the height of the components does not matter as the bearing thickness on the lateral side can be adjusted [7]. In our series, the same thickness bearings were used in the two compartments in 47 % of patients, while a thinner lateral one was used in 24 % of patients and a lateral bearing one size thicker in the remaining. Care should be taken not to undermine the tibial eminence as avulsion is a known complication seen in simultaneous Bi-UKA or bicruciate preserving TKA. Indeed, in the original series of Oxford Bi-UKA there were 5 patients out of 125 (4 %) with an intra-operative avulsion of the tibial eminence [7]. In the current series, we have had no avulsions of the tibial eminence and suspect that it is less likely to occur with staged rather than simultaneous Bi-UKA, as the bone medially will have had time to heal and strengthen.
This paper has some limitations. This is a small series with midterm follow-up. Limited follow-up makes it impossible to draw definite conclusions about the long-term outcome of this treatment option. However, the short-term outcome reported in this series demonstrates that the technique is safe and highly effective. Usually, patients with good short- to midterm outcome after UKA continue to have excellent outcome in the long term. Although the number of patients is limited, this is a relatively uncommon clinical situation, and we have followed each patient without any loss to follow-up. As said before, lateral progression is an infrequent reason to revise an UKA; therefore, it is difficult to enrol larger cohorts. Another weakness of the study is lack of a comparative group. It is hard to compare this treatment option to other treatment options such as a revision to a TKA as the indication for revision needs to be matched for fair comparison.
For the past 30 years, we have not used or recommended Bi-UKA as a primary procedure, as we have not found an appreciable need for this. Recently, simultaneous Bi-UKA are gaining interest with some doing large numbers, but it is probably too soon to consider this operation as a primary and widely indicated procedure. The reason behind the different approach may relate to the implants. Following an Oxford medial UKA, damage to the PFJ, however severe, does not appreciably compromise the outcome, and long-term failure due to PFJ problems is extremely uncommon [3]. However, with fixed-bearing UKAs, such as the Miller-Galante, PFJ problems are the commonest failure mode in the second decade, and it is recommended that damage to the PFJ is a contraindication [1]. Similarly with the Oxford UKA, full-thickness cartilage loss on the medial, not weight-bearing aspect of the lateral femoral condyle, can be ignored [11]. In a hypothetic treatment algorithm, it seems sensitive that the first procedure should be a medial UKA, and if symptomatic arthritis develops in the other compartments, a staged Bi-UKA should be done. The need for a secondary PFJ replacement has been found to be an exception, and the incidence of lateral progression is very rare as well (2.5 % over 15 years) [18]. Most other surgeons using the Oxford UKA have had similarly low rates of progression of disease laterally [20]. However, this is not always the case [5, 12], and there is evidence that the higher incidence of progression is associated with some release of the medial collateral ligament during surgery.
Improved life expectancy and broadening of surgical indications does mean that the incidence of patients presenting with symptomatic LCOA after a successful medial UKA is likely to rise with time. Patients who presented with lateral progression after medial Oxford UKA in our series are typically elderly and have associated comorbidities; thus, performing a UKA-to-TKA revision may be challenging. It is important that they are offered a reliable solution, which has low morbidity and mortality, and a satisfactory functional outcome.
Conclusions
Use of a lateral UKA represents a promising solution in selected patients, provided the medial UKA is functioning well. Thus, this is one more option to consider before performing an UKA-to-TKA revision, according to patient features and surgeon experience. When the Oxford UKA is used as the primary procedure, wear rates are negligible and implant loosening is rare [10, 19]. Therefore, we found staged Bi-UKA represents an extremely good alternative to TKA for the treatment of LCOA after medial UKA, although long-term follow-up and a comparison group are needed to draw definitive conclusions.
References
Argenson JN, Blanc G, Aubaniac JM, Parratte S (2013) Modern unicompartmental knee arthroplasty with cement: a concise follow-up, at a mean of twenty years, of a previous report. J Bone Joint Surg Am 95(10):905–909
Baker PN, Petheram T, Jameson SS, Avery PJ, Reed MR, Gregg PJ, Deehan DJ (2012) Comparison of patient-reported outcome measures following total and unicondylar knee replacement. J Bone Joint Surg Br 94(7):919–927
Beard DJ, Pandit H, Gill HS, Hollinghurst D, Dodd CA, Murray DW (2007) The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. J Bone Joint Surg Br 89(12):1597–1601
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80(1):63–69
Emerson RH Jr, Higgins LL (2008) Unicompartmental knee arthroplasty with the oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg Am 90(1):118–122
Goodfellow J, O’Connor J, Pandit H, Dodd CA, Murray D (2016; In Press) Unicompartmental arthroplasty with the Oxford knee. 2nd edn., Oxford
Goodfellow JW, O’Connor J (1986) Clinical results of the Oxford knee. Surface arthroplasty of the tibiofemoral joint with a meniscal bearing prosthesis. Clin Orthop Relat Res 205:21–42
Gulati A, Chau R, Pandit HG, Gray H, Price AJ, Dodd CA, Murray DW (2009) The incidence of physiological radiolucency following Oxford unicompartmental knee replacement and its relationship to outcome. J Bone Joint Surg Br 91(7):896–902
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Kendrick BJ, Longino D, Pandit H, Svard U, Gill HS, Dodd CA, Murray DW, Price AJ (2010) Polyethylene wear in Oxford unicompartmental knee replacement: a retrieval study of 47 bearings. J Bone Joint Surg Br 92(3):367–373
Kendrick BJ, Rout R, Bottomley NJ, Pandit H, Gill HS, Price AJ, Dodd CA, Murray DW (2010) The implications of damage to the lateral femoral condyle on medial unicompartmental knee replacement. J Bone Joint Surg Br 92(3):374–379
Lewold S, Goodman S, Knutson K, Robertsson O, Lidgren L (1995) Oxford meniscal bearing knee versus the Marmor knee in unicompartmental arthroplasty for arthrosis. A Swedish multicenter survival study. J Arthroplasty 10(6):722–731
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384(9952):1437–1445
Lombardi AV Jr, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA (2009) Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res 467(6):1450–1457
Manzotti A, Cerveri P, Pullen C, Confalonieri N (2014) A flat all-polyethylene tibial component in medial unicompartmental knee arthroplasty: a long-term study. Knee 21(Suppl 1):S20–S25
Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, Dawson J (2007) The use of the Oxford hip and knee scores. J Bone Joint Surg Br 89(8):1010–1014
Murray DW, Goodfellow JW, O’Connor JJ (1998) The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br 80(6):983–989
Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW (2015) The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Joint J 97-B(11):1493–1500
Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW (2011) Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br 93(2):198–204
Price AJ, Svard U (2011) A second decade lifetable survival analysis of the Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res 469(1):174–179
Romagnoli S, Marullo M, Massaro M, Rustemi E, D’Amario F, Corbella M (2015) Bi-unicompartmental and combined uni plus patellofemoral replacement: indications and surgical technique. Joints 3(1):42–48
Sun PF, Jia YH (2012) Mobile bearing UKA compared to fixed bearing TKA: a randomized prospective study. Knee 19(2):103–106
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Tibrewal SB, Grant KA, Goodfellow JW (1984) The radiolucent line beneath the tibial components of the Oxford meniscal knee. J Bone Joint Surg Br 66(4):523–528
Weston-Simons JS, Pandit H, Kendrick BJ, Jenkins C, Barker K, Dodd CA, Murray DW (2014) The mid-term outcomes of the Oxford Domed Lateral unicompartmental knee replacement. Bone Joint J 96-B(1):59–64
Acknowledgments
The authors would like to thank all those who assisted with the collection and processing of data, particularly Jo Brown, Barbara Marks and Jenny Ferris.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution or other non-profit organisation with which one or more of the authors are associated.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Pandit, H., Mancuso, F., Jenkins, C. et al. Lateral unicompartmental knee replacement for the treatment of arthritis progression after medial unicompartmental replacement. Knee Surg Sports Traumatol Arthrosc 25, 669–674 (2017). https://doi.org/10.1007/s00167-016-4075-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4075-4